Neck pain is a widespread issue, affecting millions globally. While many cases resolve on their own or with simple treatments, persistent or severe neck pain can significantly impact daily life. One potential, yet often overlooked, cause of chronic neck pain and related symptoms is cervical spine instability (CSI). Accurate Cervical Spine Instability Diagnosis is crucial for effective management and treatment. This article will delve into understanding cervical instability, its symptoms, causes, and most importantly, the diagnostic process.
Understanding Cervical Spine Instability
Cervical spine instability, also known as cervical instability, arises when the ligaments in your neck become excessively loose or lax. These ligaments are vital connective tissues that hold the vertebrae of your cervical spine (neck) together, ensuring stability and controlled movement. When these ligaments are weakened or damaged, they can no longer adequately support the cervical spine. This laxity leads to an abnormal, excessive range of motion between the vertebrae, affecting the structural integrity of the cervical spine and potentially impacting surrounding muscles, nerves, and even the spinal cord.
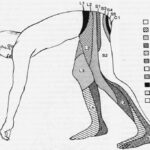
To better grasp cervical instability, it’s helpful to understand the basic anatomy of your spine.
Anatomy of the Spine and Cervical Region
Your spine, or vertebral column, is a complex structure divided into three main sections:
- Cervical Spine (Neck): The uppermost section, consisting of 7 vertebrae (C1-C7), forming a natural inward curve known as the cervical curve. This region is remarkably flexible, supporting the weight of the head and allowing for a wide range of head movements.
- Thoracic Spine (Middle/Upper Back): Located in the mid-back, composed of 12 vertebrae (T1-T12) and forming an outward curve. It provides stability and attachment points for the ribs.
- Lumbar Spine (Lower Back): The lower section of the spine, with 5 vertebrae (L1-L5), forming an inward curve. It bears the majority of the body’s weight and provides flexibility for bending and twisting.
 the-ligaments-of-the
the-ligaments-of-the
Image: Illustration depicting the spinal column and highlighting the intricate network of ligaments that provide stability and support to the vertebrae.
When viewed from the side, a healthy spine exhibits a gentle “S” shape due to these natural curves. These curves are essential for strength, flexibility, and shock absorption. The vertebrae themselves are separated and cushioned by intervertebral discs, which act as shock absorbers, provide spacing, and enable flexible movement. Furthermore, ligaments play a critical role in connecting vertebrae, providing stability, and protecting the spinal cord and discs. The major spinal ligaments include the ligamentum flavum, anterior longitudinal ligament (ALL), and posterior longitudinal ligament (PLL), which work together to limit excessive vertebral movement and maintain spinal alignment.
Symptoms and Causes of Cervical Instability
The symptoms of cervical instability can be diverse and vary significantly between individuals, depending on the severity of the instability and the underlying cause. Due to the intricate network of nerves and muscles in the neck and its connection to the central nervous system, cervical instability can manifest in a wide array of symptoms, both physical and neurological.
Common symptoms associated with ligament laxity and cervical instability include:
- Headaches: Including tension headaches, migraines, and headaches originating from the base of the skull (cervicogenic headaches).
- Neck Pain and Stiffness: Chronic or recurring neck pain, often exacerbated by movement or prolonged postures.
- Muscle Spasms: Involuntary muscle contractions in the neck and shoulders as the body attempts to stabilize the unstable joint.
- Shoulder and Jaw Pain: Pain radiating to the shoulders and jaw, sometimes mimicking temporomandibular joint (TMJ) disorders.
- Dizziness and Vertigo: Feelings of imbalance, lightheadedness, or spinning sensations due to disrupted proprioceptive input from the neck.
- Tinnitus: Ringing, buzzing, or other noises in the ears, potentially linked to nerve irritation or vascular compression in the neck.
- Blurred Vision and Light Sensitivity: Visual disturbances and increased sensitivity to light, possibly due to nerve or vascular issues.
- Cognitive Issues: Including memory loss, difficulty concentrating, and brain fog, potentially resulting from altered blood flow to the brain or neurological dysfunction.
- Limb Weakness or Numbness: Weakness, tingling, or numbness in the arms and hands, indicating nerve compression or irritation.
- Fatigue: Unexplained and persistent tiredness, possibly due to chronic pain, muscle tension, and neurological stress.
- Feeling of Instability: A subjective sensation of looseness, clicking, popping, or grinding in the neck, particularly at the base of the skull.
Cervical instability can be triggered by various factors, including:
- Traumatic Injuries: Whiplash from car accidents, sports injuries, falls, or direct blows to the neck can damage cervical ligaments.
- Repetitive Strain Injuries: Overuse or repetitive motions, especially those involving poor posture, can gradually weaken ligaments over time.
- Degenerative Conditions: Cervical spondylosis, age-related degeneration of the spinal discs and joints, can contribute to ligament laxity.
- Genetic Conditions: Certain genetic disorders like Down syndrome and Ehlers-Danlos syndrome are associated with connective tissue weakness, predisposing individuals to ligament laxity.
- Connective Tissue Disorders: Conditions like rheumatoid arthritis can cause inflammation and damage to ligaments and joints, including those in the cervical spine.
- Poor Posture: Prolonged forward head posture, often referred to as “tech neck,” strains the cervical ligaments and muscles, potentially leading to instability over time. For every inch the head protrudes forward, the weight on the cervical spine increases by approximately 10 pounds.
The Crucial Role of Cervical Spine Instability Diagnosis
Given the wide range of non-specific symptoms associated with cervical instability, obtaining an accurate cervical spine instability diagnosis is paramount. Misdiagnosis or delayed diagnosis can lead to prolonged suffering and ineffective treatment. The diagnostic process typically involves a combination of a thorough physical examination and advanced imaging techniques.
Diagnostic Process for Cervical Spine Instability
-
Medical History and Physical Examination: A comprehensive evaluation begins with a detailed discussion of your medical history, including the onset, nature, and duration of your symptoms, as well as any relevant injuries or pre-existing conditions. The physical examination will assess:
- Range of Motion (ROM): Evaluating the extent and quality of neck movements, identifying any limitations or pain with specific motions.
- Neurological Examination: Assessing reflexes, muscle strength, sensation, and nerve function to identify any neurological deficits that might indicate nerve compression or damage.
- Palpation: Carefully feeling the cervical spine to identify areas of tenderness, muscle spasm, or abnormal vertebral alignment.
- Provocative Tests: Specific maneuvers designed to reproduce or exacerbate symptoms, helping to pinpoint the source of pain and instability.
-
Imaging Techniques: To visualize the structures of the cervical spine and assess for instability, various imaging modalities may be employed:
-
Magnetic Resonance Imaging (MRI): MRI is highly sensitive in visualizing soft tissues, including ligaments, discs, and the spinal cord. It can help identify ligament damage, disc herniations, spinal cord compression, and other soft tissue abnormalities that may contribute to or result from cervical instability. MRIs can be performed in different positions, such as supine (lying down) and upright (sitting or standing), to assess for instability under gravitational load.
-
Computed Tomography (CT) Scans: CT scans provide detailed images of bony structures. They are useful in evaluating vertebral alignment, fractures, and bony abnormalities that may be associated with instability.
-
Digital Motion X-rays (DMX) or Fluoroscopy: These dynamic imaging techniques capture real-time movement of the cervical spine during flexion, extension, and rotation. They can reveal abnormal motion patterns, excessive vertebral translation (slippage), and angular changes that are indicative of ligamentous laxity and instability. Upright or positional X-rays can also be taken to assess spinal alignment and stability under weight-bearing conditions.
-
Stress Radiography: In some cases, stress radiographs (flexion-extension X-rays) may be performed to further assess the degree of vertebral movement and identify instability.
-
-
Diagnostic Criteria and Key Measurements: While there isn’t a single definitive test for cervical instability, diagnosis relies on a combination of clinical findings, imaging results, and specific measurements. Radiographic measurements, such as the atlanto-dens interval (ADI) and cervical vertebral translation, can help quantify the degree of instability. These measurements are compared to established normal ranges to determine if excessive motion is present. Clinical correlation with patient symptoms is crucial in interpreting these findings.
Image: Depiction of a patient undergoing chiropractic evaluation, highlighting the importance of specialized assessment in diagnosing and addressing conditions like cervical instability.
Challenges in Cervical Spine Instability Diagnosis
Diagnosing cervical spine instability can be challenging for several reasons:
- Non-Specific Symptoms: The symptoms of CSI often overlap with other conditions, such as muscle tension, whiplash-associated disorders, migraines, and fibromyalgia, making differential diagnosis crucial.
- Lack of Awareness: Cervical instability is not always readily considered as a primary diagnosis, leading to potential delays in recognition and appropriate management.
- Subtle Instability: In some cases, the degree of instability may be subtle and not easily detected on standard imaging, requiring specialized dynamic imaging techniques.
- Subjectivity: Some diagnostic criteria rely on clinical judgment and interpretation of imaging findings, which can introduce a degree of subjectivity.
Despite these challenges, a thorough and systematic approach, incorporating a detailed history, comprehensive physical examination, and appropriate imaging studies, is essential for accurate cervical spine instability diagnosis.
Treatment Approaches and the Importance of Accurate Diagnosis
Once a cervical spine instability diagnosis is confirmed, a tailored treatment plan can be developed. Treatment approaches vary depending on the severity of the instability, the underlying cause, and individual patient factors. Conservative management options often include:
- Chiropractic Care: Gentle chiropractic adjustments may help restore proper cervical alignment and improve joint mechanics. Specific techniques, like those used in CLEAR-certified scoliosis chiropractic, may be beneficial.
- Physical Therapy: Targeted exercises to strengthen neck muscles, improve posture, and enhance neuromuscular control can provide support and stability.
- Prolotherapy and Platelet-Rich Plasma (PRP) Injections: These regenerative injection therapies aim to stimulate ligament repair and strengthen weakened ligaments.
- Cervical Collar: Short-term use of a cervical collar may provide external support and limit excessive motion during the acute phase of injury or symptom exacerbation.
- Pain Management: Medications, such as pain relievers and muscle relaxants, may be used to manage pain and muscle spasms.
In severe cases of cervical instability, where conservative measures are insufficient, surgical stabilization may be considered as a last resort.
Accurate cervical spine instability diagnosis is not only crucial for guiding appropriate treatment but also for setting realistic expectations and improving patient outcomes. By identifying the root cause of neck pain and related symptoms, healthcare professionals can develop individualized management strategies to address the specific needs of each patient and improve their quality of life.
Conclusion
Cervical spine instability is a condition characterized by excessive movement in the neck due to lax ligaments, leading to a variety of symptoms ranging from neck pain and headaches to dizziness and cognitive issues. Obtaining a precise cervical spine instability diagnosis is the first and most vital step towards effective management. If you are experiencing persistent neck pain or any of the symptoms mentioned, seeking a comprehensive evaluation from a qualified healthcare professional is essential. With accurate diagnosis and appropriate treatment, individuals with cervical instability can find relief and improve their overall well-being.