Introduction to Cheilitis
Cheilitis, broadly defined as lip inflammation, encompasses a diverse range of conditions, from common chapped lips to more complex and persistent disorders. Accurate Cheilitis Diagnosis is crucial, yet the variety of presentations and underlying causes often poses a challenge for clinicians. This condition can manifest as an isolated issue or as a symptom of systemic diseases, infections, allergic reactions, or environmental factors. Understanding the nuances of cheilitis is particularly relevant for professionals who may encounter this condition indirectly or in the context of broader health discussions. This article aims to provide a detailed guide to cheilitis diagnosis, enhancing understanding and diagnostic approaches.
Classifying Cheilitis: Duration and Etiology
Classifying cheilitis is complex due to varied nomenclature and overlapping symptoms. While numerous classifications exist, a practical approach categorizes cheilitis based on duration and etiology. This framework helps streamline cheilitis diagnosis and management. We propose a classification system that divides cheilitis into three primary groups:
- Mostly Reversible Cheilitis: These are typically transient conditions that resolve with appropriate management of the underlying cause.
- Mostly Persistent Cheilitis: These forms are chronic and often require more intensive diagnostic and therapeutic strategies.
- Cheilitis Associated with Dermatoses and Systemic Diseases: This category includes lip inflammation that is secondary to other skin or systemic conditions.
This classification provides a structured approach to cheilitis diagnosis, guiding clinicians through the differential diagnosis process.
Table 1: Proposed Classification of Cheilitis
| Mostly Reversible Cheilitis | Mostly Persistent Cheilitis | Cheilitis Associated with Dermatoses and Systemic Diseases |
|---|---|---|
| Cheilitis Simplex | Actinic Cheilitis | Lupus Erythematosus |
| Angular/Infective Cheilitis | Granulomatous Cheilitis | Lichen Planus |
| Contact/Eczematous Cheilitis | Glandular Cheilitis | Angioedema |
| Exfoliative Cheilitis | Plasma Cell Cheilitis | Pemphigoid/Pemphigus Group |
| Drug Related Cheilitis | Xerostomia | |
| Erythema Multiforme | ||
| Crohn’s Disease | ||
| Sarcoidosis, etc. |





Reversible Cheilitis: Types and Diagnosis
Reversible cheilitis encompasses conditions that are generally temporary and respond well to treatment. Accurate cheilitis diagnosis in this category involves identifying the specific subtype and its triggers.
Table 2: Prominent Features of Mostly Reversible Cheilitis
| Mostly Reversible Cheilitis | Occurrence | Related Factors | Therapy |
|---|---|---|---|
| Cheilitis Simplex | Common | Lip licking, cold, windy, dry weather | Advice on environmental conditions, lip balms, petroleum jelly, emollients, topical corticosteroids |
| Angular/Infective Cheilitis | Common | Infective agents, immune deficiency, mechanical factors, nutritional deficiencies | Elimination of local factors, topical antimycotics, antiseptics, antibiotics, topical corticosteroids |
| Contact/Eczematous Cheilitis | Very Common | Atopy, contact allergens/irritants | Topical corticosteroids (low to medium potency), emollients |
| Exfoliative Cheilitis | Rare | Lip licking/picking, psychological distress, nutritional deficiencies | Corticosteroids, psychotherapy (spontaneous resolution possible) |
| Drug Related Cheilitis | Rare | Drugs | Emollients, drug elimination if possible |
Cheilitis Simplex
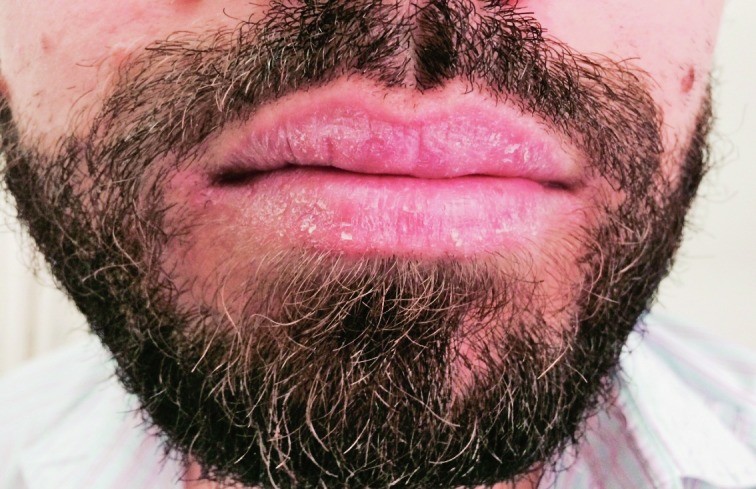
Cheilitis simplex, commonly known as chapped lips, is a frequent condition characterized by cracked lips, fissures, and desquamation, particularly of the lower lip. Cheilitis diagnosis for simplex cases often relies on clinical observation and patient history. Lip licking, a common habit, exacerbates dryness and irritation, leading to mucosal separation and cracking. Saliva’s digestive enzymes further irritate the lips by extracting moisture. In children, lip sucking and biting can result in perioral erythema.
Cheilitis simplex. Alt text: Clinical presentation of Cheilitis Simplex showing dryness and cracking of the lower lip.
Differential cheilitis diagnosis includes contact cheilitis, atopic cheilitis, and actinic cheilitis. Therapy primarily involves environmental advice and the use of lip balms, petroleum jelly, emollients, and sometimes low-potency topical corticosteroids.
Angular Cheilitis
Angular cheilitis, also known as perleche, manifests at the corners of the mouth. Cheilitis diagnosis often considers predisposing factors like deep lip angle wrinkles and lip-licking habits. Nutritional deficiencies (B vitamins, iron, zinc), poorly fitting dentures, drooling, and conditions like celiac disease are common contributing factors. Saliva plays a key role; increased production and drooling promote the condition, while decreased secretion (hyposalivation) leads to dryness, cracking, and Candida albicans invasion.
Angular cheilitis is more prevalent in diabetics, psychiatric patients (due to lip trauma), individuals on certain medications (isotretinoin), and the elderly. It is also associated with inflammatory bowel diseases like Crohn’s disease. In some cases, it occurs as part of Plummer-Vinson syndrome, alongside atrophic glossitis, esophageal webs, and anemia. Secondary bacterial or candidal infections are common.
Differential cheilitis diagnosis includes recurrent herpes labialis and secondary syphilis. Treatment focuses on eliminating predisposing factors and using topical antimycotics, antiseptics, antibiotics, and sometimes corticosteroids.
Contact/Eczematous Cheilitis
Contact/eczematous cheilitis is an inflammatory reaction to irritants or allergens in products like lipsticks, oral hygiene items, foods, fragrances, preservatives, and dental materials. Cheilitis diagnosis involves identifying potential contactants through patient history and patch testing. Symptoms include dryness, scaling, erythema, and fissuring, more common on the skin than mucosa. Atopic dermatitis is a predisposing factor. Cheilitis venenata is a term specifically for allergic contact reactions.
Contact/eczematous cheilitis. Alt text: Clinical appearance of Contact Cheilitis showing erythema and scaling affecting the lip skin.
Common allergens include lipstick components, rubber, leather, nail polish substances, metals, and topical antibiotics. Reactions to topical medications, virostatic agents, and sunscreens are also possible. Factitial cheilitis, a self-induced form, is often triggered by stress. Patch testing, particularly with the European baseline series, is crucial for cheilitis diagnosis to identify causative allergens.
Differential cheilitis diagnosis includes cheilitis simplex and exfoliative cheilitis. Treatment involves eliminating the causative agents and using topical corticosteroids and emollients.
Exfoliative Cheilitis
Exfoliative cheilitis is characterized by constant desquamation, often on the lower lip. Cheilitis diagnosis considers factors such as frequent lip moisturization, nutritional deficiencies, oral candidiasis, allergies, and HIV. It presents with continuous peeling of the vermilion. Lips may initially appear normal or red, followed by thickening and peeling in cycles. Bleeding and hemorrhagic crusts may occur. Exacerbating factors include mouth breathing, lip manipulation, and infections.
Differential cheilitis diagnosis includes contact cheilitis and cheilitis simplex. Treatment options include topical corticosteroids, calcineurin inhibitors, Calendula officinalis L., and psychotherapy in some cases. Spontaneous resolution is possible.
Drug-Induced Cheilitis
Drug-induced cheilitis results from medication intake, primarily retinoids but also topical antibiotics, virostatic agents, and lip care products. Cheilitis diagnosis here relies on medication history. Reactions can manifest as lichenoid reactions, fixed drug eruptions, or erythema multiforme-like changes. Emollients are essential for treatment, and discontinuing the offending drug is crucial when possible.
Irreversible Cheilitis: Chronic Conditions
Irreversible cheilitis includes chronic conditions requiring biopsy and histological examination for definitive cheilitis diagnosis.
Table 3: Common Features of Mostly Persistent Cheilitis
| Mostly Persistent Cheilitis | Occurrence | Related Factors | Therapy |
|---|---|---|---|
| Actinic Cheilitis | Rare | Sun damage (outdoor workers, fair-skinned men) | Topical corticosteroids or 5-fluorouracil, chemical peel, cryotherapy, electrosurgery, vermilionectomy, immunosuppressants, surgery |
| Granulomatous Cheilitis | Rare | Other granulomatous diseases | Topical, intralesional, and systemic corticosteroids and/or antibiotics |
| Glandular Cheilitis | Very Rare | Smoking, poor oral hygiene, sunlight | Systemic antibiotics and topical, intralesional or systemic corticosteroids, or surgical excision |
| Plasma Cell Cheilitis | Very Rare | Unknown | Topical and intralesional corticosteroids, destructive measures, immunosuppressants |
Actinic (Solar) Cheilitis
Actinic cheilitis, or sailor’s lip, is lower lip damage from UV radiation, considered premalignant. Cheilitis diagnosis is critical due to its malignant potential. It is common in outdoor workers. Cheilitis abrasiva praecancerosa is used when erosions are prominent.
Actinic cheilitis (a photo from ref. 23; with the author’s permission and by the courtesy of Professor Mravak-Stipetić). Alt text: Actinic Cheilitis showing whitish discoloration and thickening of the lower lip vermilion border due to sun damage.
It mainly affects middle-aged, fair-skinned men and requires biopsies to rule out dysplasia or cancer. Clinical signs include painless thickening and whitish discoloration. The vermilion border becomes indistinct, and lips may become scaly and indurated. Histopathology ranges from epithelial atrophy to squamous cell carcinoma in situ.
Differential cheilitis diagnosis includes epithelial dysplasia, squamous cell carcinoma, and other conditions. Treatment aims to relieve symptoms and prevent squamous carcinoma, using various modalities including topical agents, cryotherapy, and surgery. Sun protection is crucial.
Granulomatous Cheilitis
Granulomatous cheilitis, or orofacial granulomatosis, is chronic lip swelling of unknown cause, starting in young adults. Cheilitis diagnosis is based on clinical presentation and histology. It presents with intermittent or permanent lip swelling. Etiology is unclear, but inflammatory cell influx and dietary allergens like cinnamon are suspected.
Granulomatous cheilitis. Alt text: Granulomatous Cheilitis demonstrating significant swelling and enlargement of the upper lip.
It can occur as isolated Miescher’s cheilitis or with systemic granulomatous diseases like Crohn’s, sarcoidosis, and Melkersson-Rosenthal syndrome. Melkersson-Rosenthal syndrome includes granulomatous cheilitis, facial palsy, and plicated tongue. Histology shows granulomatous inflammation.
Differential cheilitis diagnosis includes angioedema, tuberculosis, and other conditions causing lip swelling. Treatment includes corticosteroids, antibiotics, dietary changes, and surgery, though not always necessary.
Glandular Cheilitis
Glandular cheilitis is a rare chronic inflammation of minor salivary glands, mainly of the lower lip. Cheilitis diagnosis involves clinical and histological assessment. Risk factors include smoking, poor hygiene, sunlight, and infection. Variants include simplex and apostematosa forms. The simplex form presents with red papules and edema. The apostematosa form involves secondary staphylococcal infection with pus drainage.
Histopathology is nonspecific. Differential cheilitis diagnosis includes other cheilitis forms and squamous cell carcinoma. Management involves identifying and addressing etiologic factors. Treatment includes antibiotics, corticosteroids, or surgical excision.
Plasma Cell Cheilitis
Plasma cell cheilitis is a very rare inflammation with plasma cell infiltration in the dermis. Cheilitis diagnosis relies on histology. Clinically, it presents as eroded or erythematous-violaceous plaques. Histology shows plasma cell infiltrate.
Differential cheilitis diagnosis includes actinic and allergic contact cheilitis. Treatment includes corticosteroids, calcineurin inhibitors, destructive methods, or immunosuppressants.
Cheilitis Associated with Skin and Systemic Diseases
Cheilitis can manifest as part of various dermatoses and systemic diseases. Cheilitis diagnosis in these cases is secondary to identifying the primary condition.
Lupus Erythematosus
Discoid lupus erythematosus can involve the lips, presenting as diffuse cheilitis. Systemic lupus erythematosus lip changes include erythema, purpura, erosions, or ulcerations. Oral ulcerations are a diagnostic criterion for systemic lupus.
Differential cheilitis diagnosis includes allergic contact dermatitis, actinic cheilitis, and lichen planus.
Lichen Planus
Lichen planus affects the lips in 6% of cases, with reticular Wickham’s striae, erythema, and erosions, especially on the lower lip.
Differential cheilitis diagnosis includes lichenoid drug reactions and discoid lupus erythematosus.
Angioedema
Angioedema often affects the lips, usually due to allergies, causing transient swelling. Macrocheilia refers to permanent lip swelling. Cheilitis diagnosis focuses on identifying triggers for angioedema.
Bullous Diseases
Bullous diseases like pemphigus vulgaris can manifest on the lips, often as initial oral lesions with erosions. Pemphigoid group diseases can also present similarly. Cheilitis diagnosis requires complex pemphigus and pemphigoid workups.
Lip lesions/cheilitis in association with pemphigus vulgaris. Alt text: Pemphigus Vulgaris related Cheilitis showing blistering and erosions on the lip mucosa.
Other Dermatoses
Lips can be affected in erythema multiforme, atopic dermatitis, herpes simplex, Stevens-Johnson syndrome, and toxic epidermal necrolysis, often with erosions and crusts.
Lip lesions/cheilitis in association with erythema multiforme. Alt text: Erythema Multiforme associated Cheilitis displaying characteristic target lesions and crusting on the lips.
Discussion: Enhancing Cheilitis Diagnosis
Cheilitis is a common inflammatory condition of the lips with diverse etiologies. Accurate cheilitis diagnosis is essential for effective management. It can be isolated or part of systemic conditions, including anemia, candidiasis, and allergic reactions. Common forms include angular, contact, actinic, and exfoliative cheilitis. Contact cheilitis requires detailed history taking to identify irritants or allergens. Chronic conditions like actinic and granulomatous cheilitis often necessitate biopsies for definitive cheilitis diagnosis.
Effective cheilitis diagnosis requires a comprehensive approach, including oral cavity, skin, and mucosae examination. Patient history is crucial, considering medical history, environmental exposures, habits, and potential deficiencies. Distinguishing between reversible and irreversible forms is vital for treatment planning.
Table 4: Common Diagnostic Parameters/Procedures Related to Specific Cheilitis Group
| Mostly Reversible
