Chronic diarrhea, defined as diarrhea lasting for more than four weeks, is a prevalent condition affecting approximately 5% of the global population, irrespective of age, gender, ethnicity, or socioeconomic background. This persistent condition significantly impacts patient well-being and quality of life, leading to considerable healthcare costs for diagnosis and management. The Chronic Diarrhea Differential Diagnosis is extensive, encompassing a wide array of etiologies, including infections, endocrine disorders, malabsorption syndromes, and gut-brain interaction disorders. The overlapping nature of symptoms across these conditions complicates accurate diagnosis, potentially causing diagnostic delays or misdiagnosis. This review aims to provide a detailed overview of the chronic diarrhea differential diagnosis, with a particular focus on irritable bowel syndrome with diarrhea (IBS-D) and exocrine pancreatic insufficiency (EPI), two conditions that may present with similar symptoms yet necessitate distinct management approaches due to their differing underlying causes. We will outline a structured four-step diagnostic strategy and propose a practical algorithm to aid in the efficient differentiation of IBS-D, EPI, and other causes of chronic diarrhea. Our goal is to enhance diagnostic precision, ultimately improving patient outcomes, health-related quality of life, and reducing the economic burden on healthcare systems.
The human and economic burden of chronic diarrhea is substantial. It diminishes health-related quality of life, disrupts daily routines, and significantly increases healthcare resource utilization. Recent data from the United States in 2016 revealed over 36.8 million ambulatory visits for gastrointestinal symptoms, with diarrhea being the fourth most common symptom prompting these visits and the sixth most common gastrointestinal diagnosis.
The differential diagnosis of chronic diarrhea is broad and encompasses a diverse range of conditions. These include infectious etiologies (bacterial, parasitic, viral), endocrinopathies (hyperthyroidism, diabetes), maldigestive and malabsorptive disorders (celiac disease, lactose intolerance, exocrine pancreatic insufficiency [EPI]), disorders of gut-brain interaction (irritable bowel syndrome [IBS]), inflammatory conditions (Crohn’s disease, ulcerative colitis), medication side effects (laxatives), and toxic substance ingestion (alcohol abuse). The symptomatic overlap among these conditions often poses diagnostic challenges, leading to potential delays or misdiagnoses. Therefore, a systematic and efficient diagnostic approach is crucial for timely and accurate patient management.
This review offers a comprehensive strategy for differentiating and accurately diagnosing the various diarrhea-related conditions encountered in clinical practice. We specifically focus on distinguishing IBS-D and EPI from each other and from other conditions with similar presentations. This approach aims to facilitate earlier diagnosis, more targeted treatment, improved patient quality of life, and more efficient healthcare resource utilization.
IRRITABLE BOWEL SYNDROME
Irritable bowel syndrome (IBS) stands as the most prevalent cause of diarrhea in developed nations, with an estimated prevalence ranging from 4% to 9% in the United States, based on Rome IV criteria. While IBS can manifest at any age, it is most commonly diagnosed in women between 20 and 40 years old, with women being diagnosed approximately twice as frequently as men (14% vs. 8.9%).
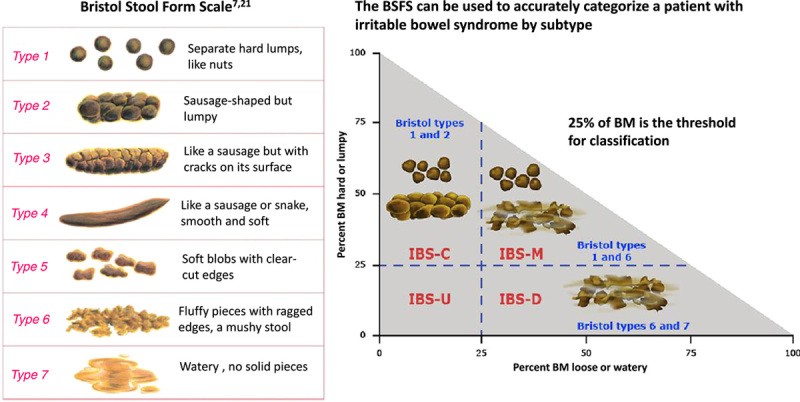
According to the Rome IV clinical criteria, IBS diagnosis requires recurrent abdominal pain, on average, at least one day per week, associated with changes in visceral sensation related to defecation and/or alterations in stool form or frequency. These symptoms should impact the patient’s quality of life or ability to perform daily activities. While the Rome IV criteria do not specify a symptom duration for clinical diagnosis, practitioners must confidently exclude other potential diagnoses. The Rome IV research criteria are more stringent, requiring symptoms to be present for the preceding three months with onset at least six months before diagnosis (Table 1). Common symptoms associated with IBS-D, though not part of the core definition, include abdominal bloating and distension, fecal urgency, feelings of incomplete evacuation, and mucus passage in stools. Stools are typically watery, classified as Bristol Stool Form Scale 6-7 (Figure 1), and occur during waking hours. Stress is a recognized exacerbating factor. Alarm features or ‘red flags’ that necessitate further evaluation for organic causes beyond IBS include symptom onset after age 50, unintentional weight loss, acute unexplained changes in symptoms, recurrent bleeding or anemia, and a family history of inflammatory bowel disease, celiac disease, or colorectal cancer (Figures 2 and 3).
TABLE 1. Rome IV Diagnostic Criteria for Irritable Bowel Syndrome
| Clinical diagnostic criteria | Criteria for patient inclusion in clinical trials, epidemiological studies, or pathophysiological studies |
|---|---|
| Recurrent abdominal pain on average at least 1 day/week, associated with two or more of the following criteria[*]: • Related to defecation • Associated with a change in frequency of stool • Associated with a change in form (appearance) of stoolBothersome symptoms: • Interfere with daily activities • Require attention • Cause worry or interfere with the quality of life | Recurrent abdominal pain on average at least 1 day/week in the last 3 mo, associated with two or more of the following criteria[†]: • Related to defecation • Associated with a change in frequency of stool • Associated with a change in the form (appearance) of stool |
[*For the last 8 weeks.]
[†For the last 3 months with symptom onset at least 6 months before diagnosis.]
FIGURE 1. Bristol Stool Form Scale and IBS Subtypes
Image alt text: Bristol Stool Form Scale illustrating types 1 through 7, correlating stool consistency with IBS subtypes IBS-C, IBS-D, IBS-M, and IBS-U.
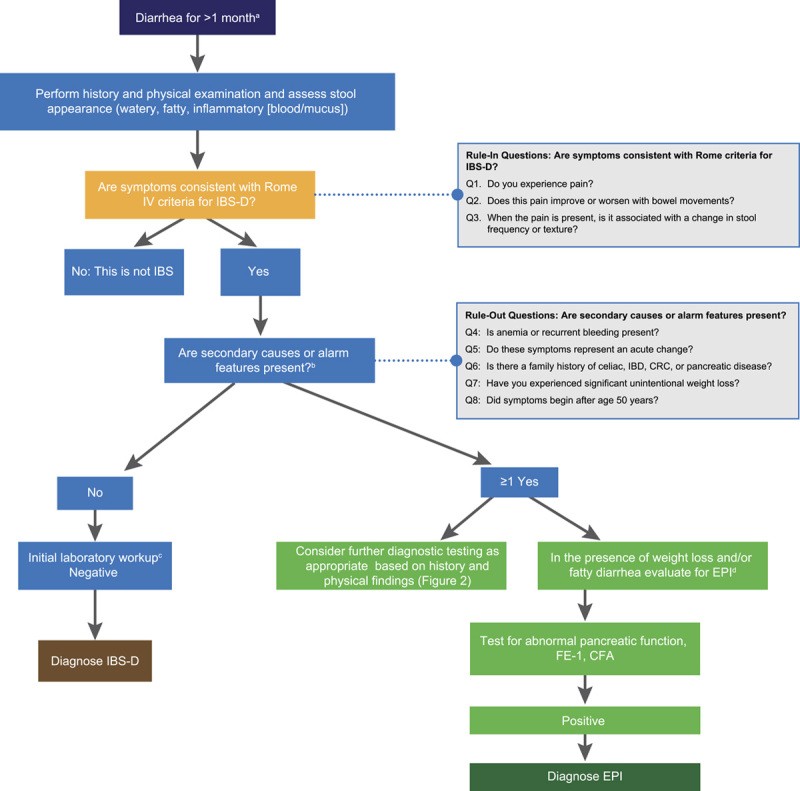
FIGURE 2. General Sequence for Differential Diagnosis of Chronic Diarrhea
Image alt text: Flowchart illustrating a general diagnostic sequence for chronic diarrhea, including steps for initial assessment, alarm feature evaluation, and targeted testing for conditions like celiac disease, IBD, and EPI.
FIGURE 3. A General Strategy for the Differential Diagnosis of Patients with Chronic Diarrhea: EPI or IBS-D?
Image alt text: Algorithm outlining a diagnostic strategy for differentiating between EPI and IBS-D in patients with chronic diarrhea, incorporating alarm features, initial blood and stool tests, and pancreatic function testing.
While chronic abdominal pain is a defining symptom of IBS, distinguishing it from functional diarrhea can be challenging due to significant symptom overlap; patients may even fluctuate between these diagnoses. Patients with IBS, particularly those with frequent pain, often exhibit increased psychological distress and somatic comorbidities compared to those with functional diarrhea, necessitating appropriate evaluation and early management.
Currently, there is no universally accepted biomarker for IBS diagnosis. Extensive testing to exclude organic causes is generally discouraged due to its high cost, inefficiency, and low diagnostic yield. Accurate IBS diagnosis can often be achieved through subjective patient history alone. Studies have shown that Rome criteria, in the absence of alarm symptoms, exhibit high specificity and positive predictive values for IBS diagnosis. Consequently, clinical guidelines recommend minimizing diagnostic investigations and adopting a positive diagnostic strategy. Major gastroenterology organizations advise against routine colonoscopy for IBS diagnosis, except in patients over 45 (for age-appropriate screening) or those presenting with warning signs of more serious conditions.
Recommended diagnostic tests are limited and primarily aim to exclude other conditions. These include serologic testing for celiac disease (serum IgA and tissue transglutaminase IgA), fecal calprotectin (or lactoferrin) and C-reactive protein to exclude inflammatory bowel disease in patients without alarm features, and stool antigen testing for Giardia in individuals with relevant risk factors (travel to endemic areas, exposure to untreated water, daycare attendance).
Irritable Bowel Syndrome Subtypes
IBS is categorized into four subtypes based on predominant stool patterns: IBS-D, IBS with constipation (IBS-C), IBS with mixed bowel habits (IBS-M), and IBS unclassified (IBS-U). IBS-D is the most common subtype, affecting up to 40% of adults diagnosed with IBS. Globally, IBS-D affects approximately 1.2% of individuals, with a slight female predominance (1.3% vs. 1.0% in males).
Patients with IBS-D typically present with Bristol Stool Form Scale type 6 or 7 stools (loose, mushy, watery) in more than 25% of bowel movements and type 1 and 2 stools (hard, lumpy, pellet-like) in less than 25% of bowel movements (Figure 1). Rome IV criteria emphasize assessing stool texture on days with abdominal pain for improved precision in IBS subtype differentiation.
The overlapping symptoms of IBS-D with conditions like EPI, celiac disease, small intestinal bacterial overgrowth, disaccharidase deficiencies, Crohn’s disease, ulcerative colitis, and infections complicate diagnosis. However, initial stool characterization as watery (suggestive of IBS), fatty or greasy (suggestive of EPI), or inflammatory (suggestive of inflammatory bowel disease) can help narrow the chronic diarrhea differential diagnosis (Table 2).
TABLE 2. Narrowing the Diagnosis According to Stool Characteristics
| Watery | Fatty/Greasy | Inflammatory |
|---|---|---|
| Osmotic • Carbohydrate malabsorption • Celiac disease • Osmotic laxativesSecretory • Bile acid malabsorption • Microscopic colitis • Endocrinopathies (eg, diabetes, hyperthyroidism) • Medications (eg, metformin)Functional • Functional diarrhea • Irritable bowel syndrome | Malabsorption or maldigestion • Celiac disease • Small intestinal bacterial overgrowth • Giardiasis • Whipple disease • Inadequate luminal bile acid concentration • Exocrine pancreatic insufficiency | Inflammatory bowel disease • Segmental colitis associated with diverticulosis (SCAD) • Infectious disease • Clostridium difficile • Invasive bacterial infections • Invasive parasitic infections • Ischemic colitis • Radiation colitis • Lymphoma |
EXOCRINE PANCREATIC INSUFFICIENCY
Exocrine pancreatic insufficiency (EPI) is most commonly associated with pancreatic diseases but can also result from various extrapancreatic conditions. Approximately 80% of children with cystic fibrosis develop EPI within the first two years of life. EPI prevalence ranges from 10% to 30% in mild chronic pancreatitis and up to 85% in severe chronic pancreatitis. Around 72% of patients with pancreatic cancer develop EPI, with a higher frequency (3.36 times) when the tumor is located in the pancreatic head compared to the body or tail. In pancreatic diseases, EPI results from reduced secretion of pancreatic enzymes and bicarbonate due to parenchymal function loss or obstruction of the main pancreatic duct.
EPI is characterized by a deficiency in the quantity or activity of pancreatic enzymes in the intestinal lumen, leading to impaired food digestion. The most clinically significant consequence of EPI is inadequate fat digestion. Diarrhea develops when the digestive capacity of the exocrine pancreas is overwhelmed by the quantity and quality of ingested food. Symptom prevalence in EPI varies considerably due to differing dietary habits and restrictions. Clinical studies in patients with confirmed EPI have reported steatorrhea (fatty/oily loose stools) frequencies ranging from 23% to 70% in chronic pancreatitis, 46% in pancreatic cancer (pre-surgery), and 15% in cystic fibrosis. A detailed patient history, including dietary habits, is crucial as low-fat diets adopted to manage symptoms can mask EPI diagnosis by reducing or eliminating steatorrhea.
Patients with EPI typically present with malabsorption syndrome symptoms, including diarrhea, abdominal distension and cramps, flatulence, and weight loss, along with nutritional deficiencies (fat-soluble vitamins, micronutrients, proteins). Symptom severity varies depending on the underlying cause, enzyme deficit, and dietary fat intake. Common symptoms include foul-smelling, fatty, loose stools; flatulence; and weight loss. Long-term consequences of EPI can include sarcopenia, osteoporosis, low-trauma fractures, metabolic bone disease (especially in chronic pancreatitis), increased infection risk, and cardiovascular disease.
EPI should be considered in the chronic diarrhea differential diagnosis in patients with a history of pancreatic disease (acute, relapsing, or chronic pancreatitis; cystic fibrosis; pancreatic cancer; acute necrotizing pancreatitis; type 1, 2, or 3c diabetes mellitus), risk factors for pancreatic disease (alcohol abuse, smoking), family history of pancreatic diseases, or pancreatic or gastric surgery. In patients without a history of pancreatic disease, EPI testing is warranted only when clinical suspicion is high.
Definitive EPI diagnosis, often challenging due to the lack of highly accurate tests, is essential to prevent complications. Diagnosis typically involves a combination of symptoms, nutritional markers, and noninvasive pancreatic function tests like the coefficient of fat absorption (CFA) and fecal elastase (FE-1). While other pancreatic function tests exist, they are either invasive (endoscopic pancreatic function test [ePFT]) or not readily available (¹³C-labeled breath tests). The direct secretin-cholecystokinin (CCK) test, the most sensitive for detecting reduced stimulated pancreatic secretion, is invasive, expensive, and cumbersome, limiting its clinical use. The ePFT after intravenous secretin administration was developed as an alternative but still has limitations. Both secretin-CCK and ePFT are mainly used for functional diagnosis of chronic pancreatitis in cases with inconclusive imaging, not for routine EPI diagnosis.
The CFA test is considered the gold standard for EPI diagnosis. However, it requires a 5-day diet containing 100g of fat daily and total fecal collection from days 3 to 5 for lab analysis. This cumbersome and unpleasant procedure is rarely used clinically. ¹³C-labeled breath tests offer an accurate and standardized alternative to CFA but are not yet widely available. Fecal elastase-1 (FE-1) test, measuring pancreatic-specific enzyme concentration in stool, is a simple, widely available, and frequently used pancreatic function test. FE-1 test involves enzyme-linked immunosorbent assay on a small stool sample. Optimal cutoff and accuracy of FE-1 for EPI diagnosis, using CFA as the gold standard, vary across studies. Sensitivity ranges from 68% to 94% and specificity from 48% to 82%, depending on the cutoff value (84 to 200 µg/g) used in different studies.
In patients with chronic diarrhea and high EPI probability (e.g., pancreatic head cancer, advanced chronic calcifying pancreatitis, pancreaticoduodenectomy, gastrectomy), pancreatic function tests may have limited diagnostic value and are not always necessary for diagnosis. Conversely, in patients with chronic diarrhea but low EPI probability (no prior pancreatic disease, no risk factors, no weight loss or nutritional deficiencies), normal FE-1 levels can effectively rule out EPI. Low FE-1 levels may indicate EPI, warranting further pancreatic investigation, but false-positive FE-1 results are not uncommon.
EPI is among several organic gastrointestinal diseases that can mimic IBS. EPI, defined by low FE-1 concentration, is observed in 5%–6% of patients meeting Rome criteria for IBS-D and 4.6% of patients with unexplained abdominal pain, diarrhea, or IBS-D. However, due to the possibility of false-positive FE-1 results in watery diarrhea, low FE-1 levels do not definitively exclude IBS-D.
DIFFERENTIAL DIAGNOSIS OF CHRONIC DIARRHEA
Early and accurate diagnosis is crucial in managing chronic diarrhea. Patients may present with a spectrum of symptoms indicative of various disorders, including IBS-D, EPI, celiac disease, small intestinal bacterial overgrowth, inflammatory bowel disease, and infections (e.g., giardiasis). Common overlapping symptoms include diarrhea, abdominal pain, bloating, and flatulence. To aid in accurate diagnosis, we propose a four-step diagnostic process (Figure 2).
Step 1: Thorough History and Physical Examination
The initial step in chronic diarrhea differential diagnosis is a comprehensive history and physical examination. Patients with diarrhea persisting for ≥4 weeks should be questioned in detail about their symptoms and diarrhea history. While clinical diarrhea is defined as loose or watery stools ≥3 times in 24 hours, patients use various definitions (loose stools, increased frequency, fecal urgency), emphasizing the need for a detailed patient history. Abnormal stool form is often more critical than frequency, as patients with functional constipation may also report diarrhea due to increased defecation frequency but further questioning may reveal straining, incomplete evacuation, and hard stools.
Initially, categorize diarrhea as watery (IBS, celiac disease, endocrinopathy, laxative misuse), fatty/greasy (malabsorptive/maldigestive diseases like celiac disease or EPI), or inflammatory (infectious or inflammatory bowel disease). However, definitive categorization can be challenging due to symptom overlap (Table 2). Further history should include: diarrhea pattern (continuous, intermittent, meal-related – differentiating secretory from osmotic diarrhea), onset, precipitating events, stool volume, presence of blood, mucus, or fat, nocturnal diarrhea, fecal urgency or incontinence. Also, explore other gastrointestinal and extraintestinal symptoms, aggravating factors (diet, stress, medications), and alleviating factors.
Step 2: Identify Risk Factors, Iatrogenic Factors, and Previous Diagnoses
To exclude extrinsic causes of chronic diarrhea, assess for recent travel (to regions with diarrhea-related pathogens like Giardia), gastrointestinal surgery (gallbladder removal, ileocecal resection, Roux-en-Y gastric bypass), radiation therapy, or diarrhea-inducing medications. Additionally, consider mucosal (celiac disease), hepatic, pancreaticobiliary, neoplastic, or systemic (endocrine, vascular, immunologic) diseases as potential risk factors for diarrhea.
Step 3: Rule Out Alarm Features
Identify alarm features suggesting more serious underlying conditions. These include recent onset, especially in older patients; nocturnal diarrhea; severe or worsening symptoms; unexplained weight loss; family history of gastroenterological or systemic diseases (celiac disease, inflammatory bowel disease, colorectal cancer); blood in stool; and unexplained iron deficiency.
Step 4: Initial Laboratory Workup
History and physical examination findings should guide laboratory investigations. If alarm features are present, testing should target the most likely etiologies. For example, in patients with meal-related fatty-greasy diarrhea, weight loss, and fat-soluble vitamin deficiencies, EPI workup is warranted. FE-1 measurement is the most common indirect test for exocrine pancreatic function; FE-1 <200 µg/g suggests EPI, and <100 µg/g indicates severe EPI. However, in patients without alarm features, presenting with symptoms consistent with functional diarrhea or IBS-D, guidelines recommend screening for celiac disease (anti-tissue transglutaminase IgA and total IgA), inflammatory bowel disease (fecal calprotectin or lactoferrin and C-reactive protein [ACG only]), and Giardia (in specific populations). Bile acid diarrhea testing (48-hour fecal bile acid assay or serum fibroblast growth factor 19 level) is also suggested.
AN ALGORITHM FOR THE DIFFERENTIAL DIAGNOSIS OF CHRONIC DIARRHEA: FOCUS ON IBS-D AND EPI
Building upon the four-step diagnostic process, we have developed a streamlined algorithm to assist clinicians in differentiating IBS-D and EPI from other diarrhea syndromes (Figure 3). This algorithm aims to minimize unnecessary diagnostic testing and healthcare costs by promoting timely and appropriate diagnosis and management. The algorithm provides a framework for rapid and accurate IBS-D diagnosis. It starts with three “rule-in” questions aligned with Rome IV criteria for IBS: (1) Do you experience abdominal pain? (2) Does pain improve or worsen with defecation? and/or (3) Is pain associated with changes in stool frequency or form? Positive answers and absence of alarm symptoms/signs (Figure 3) can lead to an IBS-D diagnosis with approximately 97% accuracy. In such cases, minimal diagnostic testing is needed. However, if alarm symptoms are present (e.g., weight loss) and EPI is suspected, nutritional markers and FE-1 testing are indicated. Abnormal results necessitate pancreatic investigation. If the pancreas appears normal, a false-positive FE-1 result is likely, EPI can be excluded, and other causes of chronic diarrhea should be explored.
DISCUSSION
Diarrhea is a common and complex condition with diverse etiologies and pathogenic mechanisms. Differentiating these conditions, especially when symptoms overlap, can be challenging. In the United States, up to 75% of patients meeting IBS criteria remain undiagnosed, highlighting this diagnostic challenge. This is concerning as IBS is the most frequent cause of diarrhea and can be diagnosed accurately with simple questions and limited testing.
EPI is a frequently reported mimic of IBS-D, often leading to misdiagnosis of EPI as IBS-D. Our proposed algorithm (Figure 3) is specifically designed to aid in distinguishing between these two disorders and differentiating them from other causes of chronic diarrhea. Importantly, this algorithm integrates recommendations from recent IBS guidelines, emphasizing a positive diagnostic strategy. This simplified algorithm should assist clinicians in achieving timely diagnoses, reducing unnecessary testing, and thus minimizing treatment delays and improving patient health and quality of life.
ACKNOWLEDGMENTS
The authors acknowledge Moira A. Hudson, PhD, and Janet E. Matsuura, PhD, of ICON plc for medical writing and editing support, funded by AbbVie. AbbVie provided medical review, but content decisions remained with the authors. No honoraria or payments were made for authorship.
Footnotes
Funding for manuscript development was provided by AbbVie. AbbVie provided courtesy medical review; author decisions on content were final. No honoraria or payments were provided for authorship.
D.M.B. consults, advises, or speaks for Alnylam, Alfasigma, Anji, Ardelyx, Arena, Bayer, AbbVie, Mahana, Owlstone, Ironwood, Salix, Takeda, Redhill, QoL Medical, Gemelli Biotech, and Vibrant. He is a Board member for the International Foundation for Gastrointestinal Disorders (IFFGD) and has received unrestricted grants from the IDP Foundation. J.E.D.-M. has received honoraria for lectures and advisory roles from AbbVie, Viatris, and Abbott Pharmaceuticals, and unrestricted research grants from AbbVie.
Contributor Information
Darren M. Brenner, Email: [email protected].
J. Enrique Domínguez-Muñoz, Email: [email protected].