Introduction
The clivus, a crucial midline bony structure at the base of the skull, is a frequent site for a diverse array of pathologies. As auto repair experts at xentrydiagnosis.store, while our primary focus is vehicle diagnostics and repair, understanding complex diagnostic challenges in other fields, like medical imaging, can broaden our problem-solving skills and analytical thinking. Just as we diagnose intricate car issues, medical professionals diagnose complex conditions in the human body. This article, tailored for an English-speaking audience, delves into the differential diagnosis of clival lesions, emphasizing the pivotal role of imaging techniques.
Clival lesions, often arising from the clivus itself or extending from adjacent areas, can be asymptomatic or manifest with subtle symptoms like headaches or cranial nerve dysfunction, notably affecting the abducens nerve due to its proximity. Advanced imaging modalities such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are indispensable for accurate diagnosis, determining the extent of the disease, and guiding therapeutic strategies. This enhanced guide aims to provide a comprehensive overview of clival and paraclival pathologies, improving upon existing resources by focusing on differential diagnosis from an imaging perspective, crucial for effective clinical decision-making.
Embryology and Anatomy of the Clivus
The term “clivus,” derived from Latin meaning “slope,” aptly describes this sloping bony structure at the central skull base, also known as the clivus of Blumenbach. Understanding its anatomy is crucial for interpreting imaging findings and narrowing down the differential diagnosis.
Anatomical Boundaries and Relations
The clivus is strategically positioned and related to several critical neurovascular structures (Fig. 1).
Fig. 1.
Alt Text: Anatomical illustration and CT scans showcasing the clivus. Part A illustrates the adult clivus with key structures labeled: 1-sphenoid sinus, 2-optic chiasm, 3-pituitary gland, 4-dorsum sellae, 5,6-VI cranial nerve and basilar artery, 7-pons. Fatty marrow within the clivus is highlighted. Part B is a sagittal CT image (bone window) showing these features. Part C is an axial CT image (bone window) displaying the petroclival fissure (PCF), internal carotid artery in the carotid canal (CC), foramen ovale (FO), and Vidian canal (VC).
- Superiorly: Dorsum sellae, sella turcica, and pituitary gland.
- Inferiorly: Foramen magnum and jugular tubercle.
- Laterally: Petroclival fissure (petro-occipital synchondrosis), petrous temporal bone, and petrous internal carotid artery (ICA).
- Anteriorly: Sphenoid sinus and nasopharynx.
- Posteriorly: Prepontine and premedullary cisterns, brainstem, and their contents.
The petro-occipital fissure, located laterally, is a key anatomical landmark and a common origin site for chondrosarcomas.
Neurovascular Relations and Embryological Origins
The sixth cranial nerve (abducens nerve) has a close relationship with the clivus, traversing the Dorello canal along the clival slope. This proximity explains why clival lesions frequently manifest with abducens nerve palsy and diplopia. The petrous ICA is lateral to the clivus, while the basilar artery is posterior. The basilar venous plexus is also present on the clival dura.
Embryologically, the clivus derives from the first and second occipital sclerotomes and the proatlas. Ossification occurs from basisphenoid and basiocciput centers, connected by the spheno-occipital synchondrosis, which fuses around age 25. The notochord’s embryologic path is closely related to the clivus, and remnants can lead to congenital variants (Fig. 2).
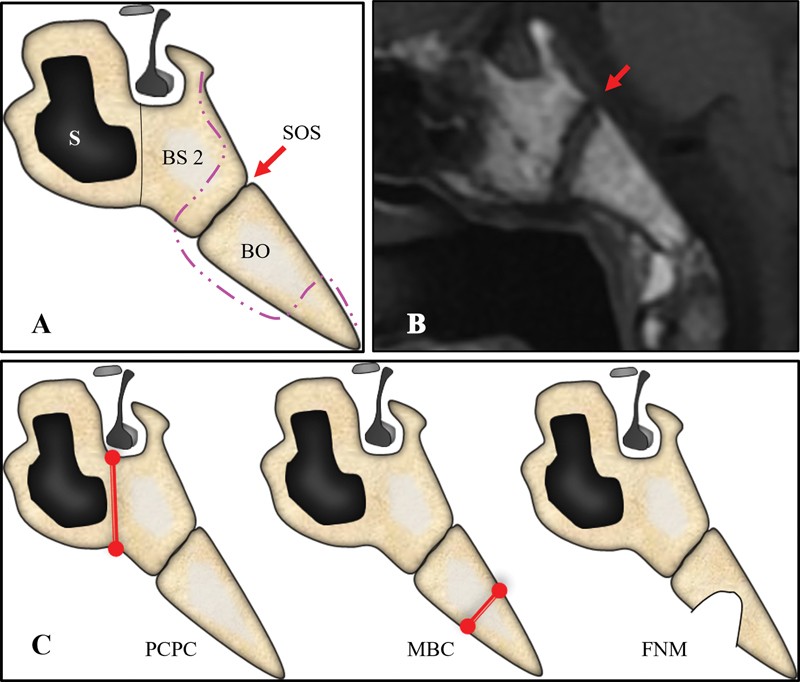
Fig. 2.
Alt Text: Diagrams and MRI of the clivus and congenital variants. Part A shows a normal clivus with the spheno-occipital synchondrosis (SOS) between basi post-sphenoid (BS2) and basiocciput (BO), with the notochord remnant path. Part B is a sagittal T1-weighted MRI of a 6-year-old, showing the SOS (red arrow). Part C illustrates locations of congenital variants: Persistent craniopharyngeal canal (PCPC), Median basal canal/canalis medianus basalis (MBC), and Fossa navicularis magna (FNM).
Age-Related MR Signal Changes in Clival Marrow
Understanding the normal age-related changes in clival bone marrow signal on MRI is crucial to avoid misinterpreting normal variations as pathology. Signal intensity is best evaluated on sagittal T1-weighted non-fat-saturated, non-contrast images. With increasing age, fatty marrow (yellow marrow) replaces red marrow, leading to higher T1 signal intensity. Heterogeneity with T1 hypointense foci can be normal. Normal clival signal is typically isointense or hyperintense relative to the pons. Hypointensity compared to the pons or intervertebral discs warrants further investigation. The maturation of marrow signal with age is illustrated in Fig. 3.
Fig. 3.
Alt Text: MRIs illustrating clival marrow signal changes with age. Part A: 6-year-old with unfused synchondrosis and T1 isointensity (red marrow). Part B: 14-year-old with unfused synchondrosis and homogeneous T1 hyperintensity (fatty marrow). Part C: Adult clivus with fused synchondrosis and homogeneous fatty marrow. In all cases, clival marrow is not darker than the pons on T1-weighted MRI.
Differential Diagnosis of Clival and Paraclival Pathologies
Clival and paraclival pathologies are diverse, encompassing congenital, inflammatory, infectious, benign, and malignant conditions (Tables 1 2 3). A systematic approach, integrating clinical presentation and imaging features, is essential for accurate differential diagnosis.
Table 1. Classification of Clival and Paraclival Abnormalities

Alt Text: Table classifying clival and paraclival abnormalities into congenital, inflammatory, infective, benign tumors, primary malignant tumors, metastatic lesions, and miscellaneous categories.
Table 2. Categorization of Clival and Paraclival Pathologies
| Pathologies involving the clivus directly | Paraclival pathologies |
|---|---|
| Basal encephalocele | Skull base osteomyelitis |
| Benign: Enchondroma, Fibrous dysplasia, Aneurysmal bone cyst, Giant cell tumor, Cholesteatoma, Ecchordosis physaliphora, Paget disease | Petrous apicitis |
| Malignant: Chordoma, Chondrosarcoma, Plasmacytoma, Langerhans cell histiocytosis, Multiple myeloma, Lymphoma, Metastases | Head and neck pathologies extending to clivus: Nasopharyngeal carcinoma, Sphenoid sinusitis, Mucocele, IgG4 disease |
| Miscellaneous: Radionecrosis | Intracranial pathologies invading the clivus: Pituitary adenoma, Meningioma, Craniopharyngioma, Neuroendocrine tumors including paragangliomas |
Alt Text: Table categorizing pathologies as directly involving the clivus or being paraclival. Direct clival pathologies include basal encephalocele, benign and malignant tumors, and miscellaneous conditions. Paraclival pathologies include osteomyelitis, petrous apicitis, head and neck extensions, and intracranial invasions.
Table 3. Age-Wise Categorization of Clival and Paraclival Pathologies
| Pediatric | Adult | No specific predilection |
|---|---|---|
| Basal encephalocele | Paget’s disease | Infective and inflammatory processes |
| Adamantinomatous craniopharyngioma | Chondrosarcoma | Fibrous dysplasia |
| Langerhans cell histiocytosis | Giant cell tumor | Neuroendocrine tumors |
| Primary skull base lymphoma | Chordoma | Enchondroma |
| Aneurysmal bone cyst | Plasmacytoma, multiple myeloma, metastases | Radionecrosis |
| Meningioma, pituitary adenoma, papillary craniopharyngioma, nasopharyngeal carcinoma |
Alt Text: Table categorizing clival and paraclival pathologies by age predilection: pediatric, adult, and no specific age preference. Pediatric conditions include encephalocele and certain tumors. Adult conditions include Paget’s disease and chordoma. Non-age-specific conditions include infections and fibrous dysplasia.
Congenital Lesions
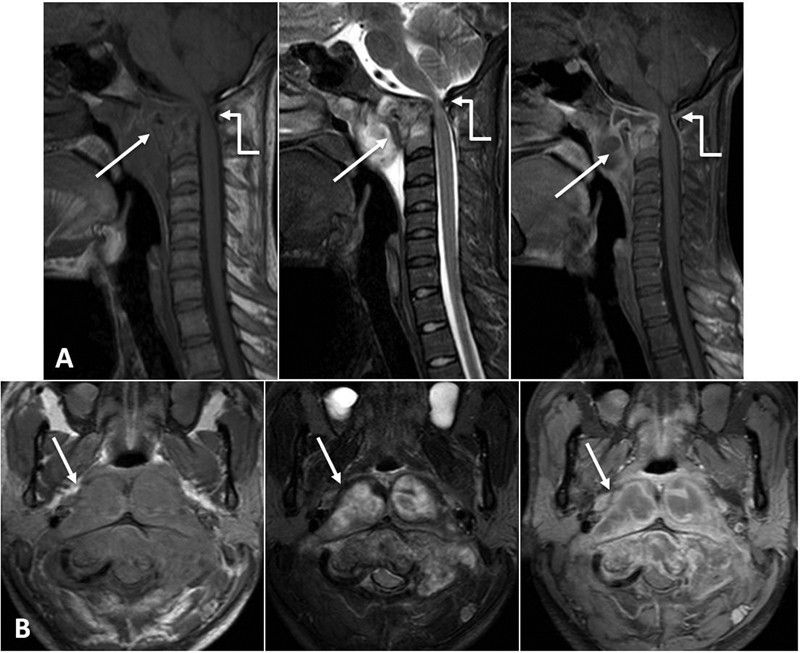
Basal Encephaloceles
Basal encephaloceles are rare congenital midline skull base defects causing herniation of brain parenchyma and meninges. They can be transsphenoidal or transethmoidal, or classified as sphenopharyngeal or spheno-orbital. Imaging, especially MRI, is critical for diagnosis, revealing the defect and herniated contents (Fig. 4).
Differential Diagnosis
- Craniopharyngioma: While also suprasellar, encephaloceles are congenital defects with herniation, unlike tumors.
- Nasal polyps: Encephaloceles contain brain tissue and meninges, unlike mucosal nasal polyps.
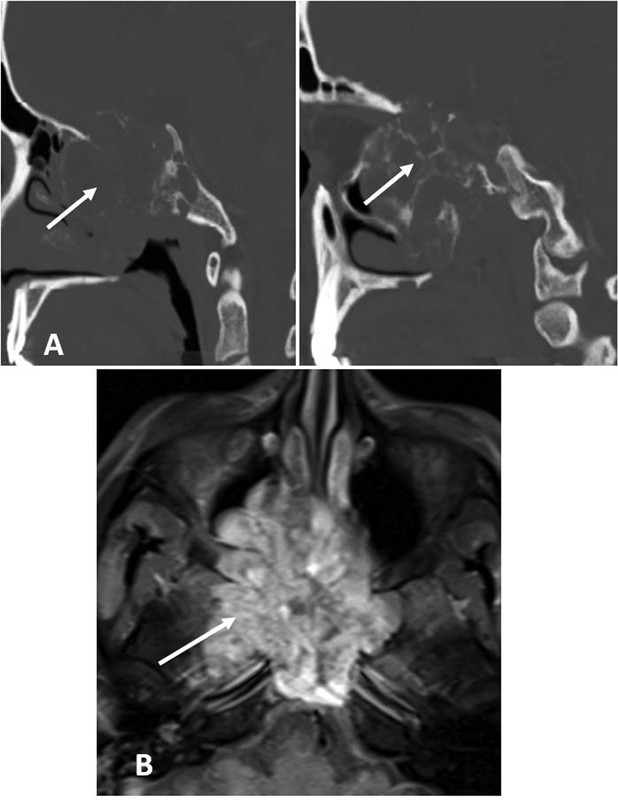
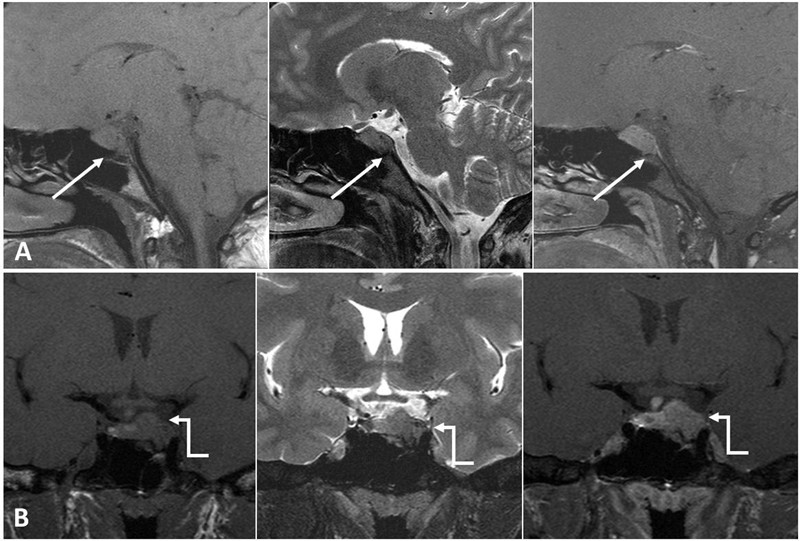
Fig. 4.
Alt Text: MRI scans of basal encephalocele in an 18-year-old girl. Sagittal T1W, T2W, and axial T2W images show a midline clival defect (arrow) with midbrain herniation into the nasopharynx (arrow). Small posterior fossa, peg-like tonsils, and hydrocephalus are also noted.
Inflammatory Conditions
Sphenoid Sinus Mucocele
Mucoceles, particularly of the sphenoid sinus, can erode into the clivus, causing neurological symptoms. Primary clival mucoceles are rare. MRI signal characteristics vary with content, typically hyperintense on T1W and T2W sequences, without enhancement.
Differential Diagnosis
- Sinonasal neoplasms: Mucoceles are expansile and cystic, while neoplasms are solid and often enhance.
- Inflammatory sinusitis: Mucoceles are well-defined, expansile lesions, unlike diffuse sinusitis.
Sphenoid Sinusitis
Sphenoid sinusitis, especially fungal, can mimic other clival pathologies. CT and MRI help delineate the extent and nature of the inflammatory process (Fig. 5).
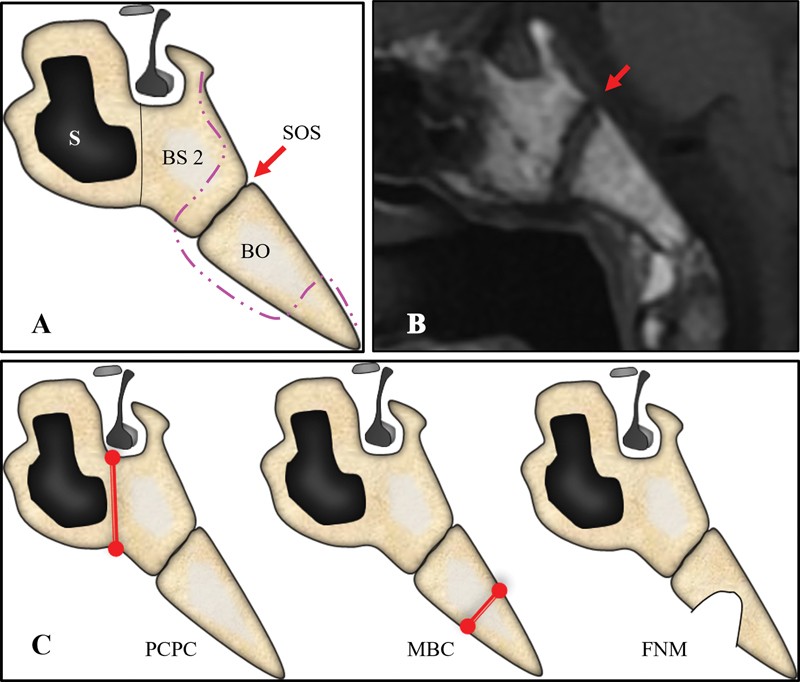
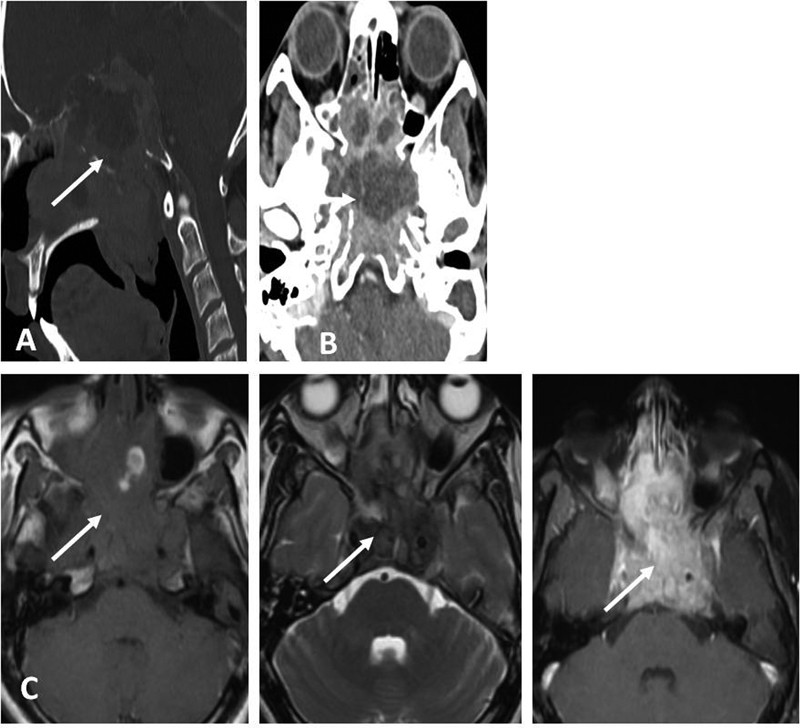
Fig. 5.
Alt Text: Coronal CT images of paranasal sinuses in allergic fungal sinusitis. Polypoidal mucosal thickening and hyperdense contents opacify sphenoid and ethmoid sinuses (arrow). Sinus wall erosion is visible (elbow arrow).
Infective Conditions
Skull Base Osteomyelitis (SBO)
SBO is a severe infection, often in elderly diabetics or immunocompromised individuals. CT shows bony erosion, and MRI reveals altered marrow signal (T1 hypointense, T2 hyperintense with enhancement). Fungal SBO may be T2 hypointense.
Differential Diagnosis
- Malignancy: SBO is typically T2 hyperintense and shows diffuse enhancement, while malignancy tends to be T2 intermediate and enhances more solidly. ESR elevation favors SBO.
- Inflammatory conditions: Infections show more aggressive bone destruction and edema than some inflammatory processes.
Tuberculous Osteomyelitis
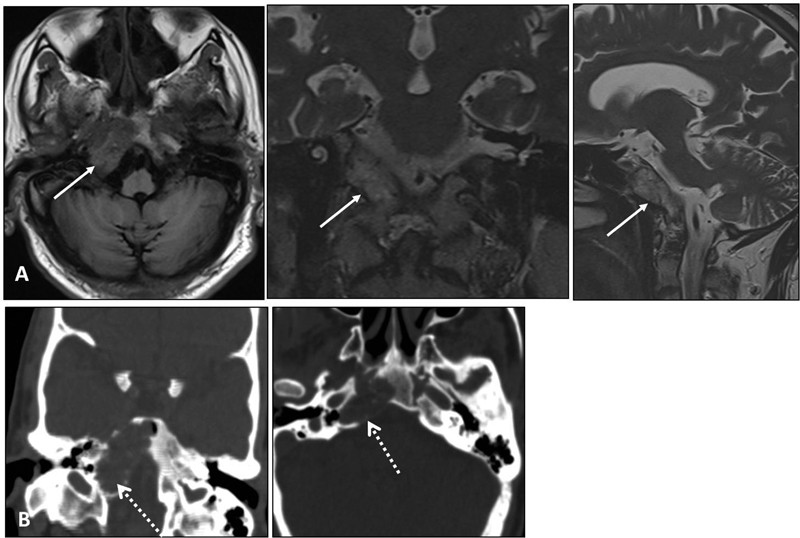
Tuberculosis of the clivus is rare but should be considered, especially with a history of TB. Imaging reveals clival destruction and soft tissue involvement (Fig. 7).
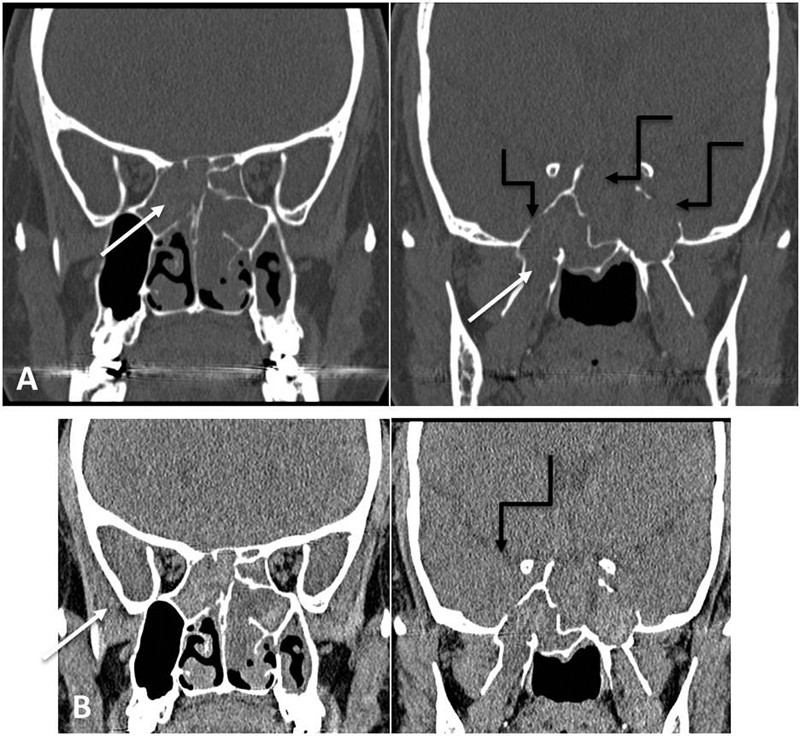
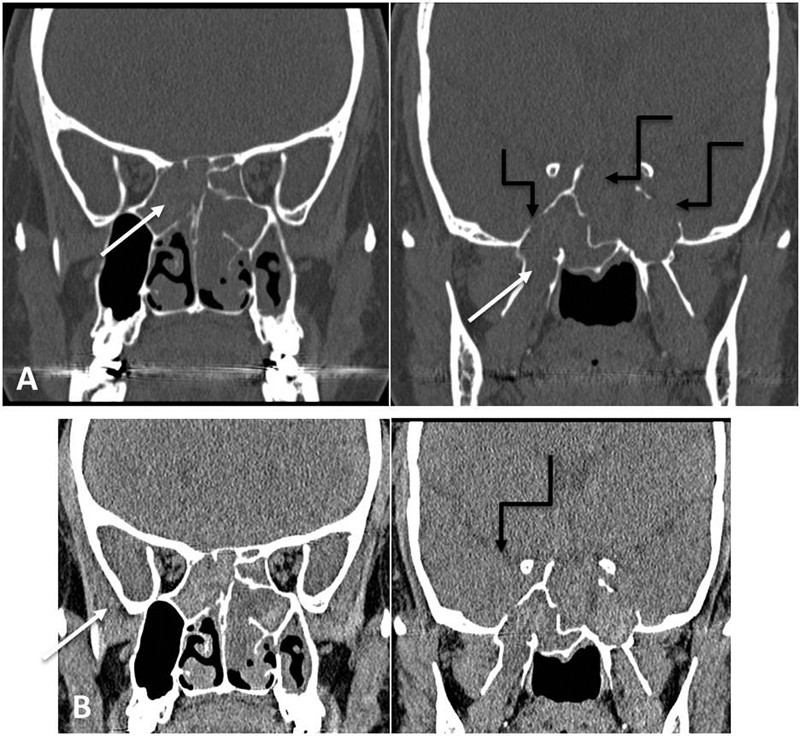
Fig. 6.
Alt Text: (I) MRI of skull base osteomyelitis. Axial T1W, T2W, and T1+C images show abnormal clival signal (arrow), enhancing soft tissue in petroclival and prevertebral regions (arrowhead), dural enhancement (elbow arrow), and otomastoiditis. (II) CT of the same patient showing clival erosion (arrow), petroclival joint widening, hypoglossal canal erosion (arrowhead), and otomastoiditis (elbow arrow).
Petrous Apicitis
Petrous apicitis, an extension of otitis media, can involve the paraclival region. MRI shows T2 hyperintensity, T1 hypointensity, and enhancement. CT shows petrous air cell opacification and bone destruction.
Differential Diagnosis
- Cholesterol granuloma: Similar location but cholesterol granulomas are often T1 hyperintense due to blood products.
- Petrous bone tumors: Apicitis is infectious/inflammatory, while tumors are neoplastic masses.
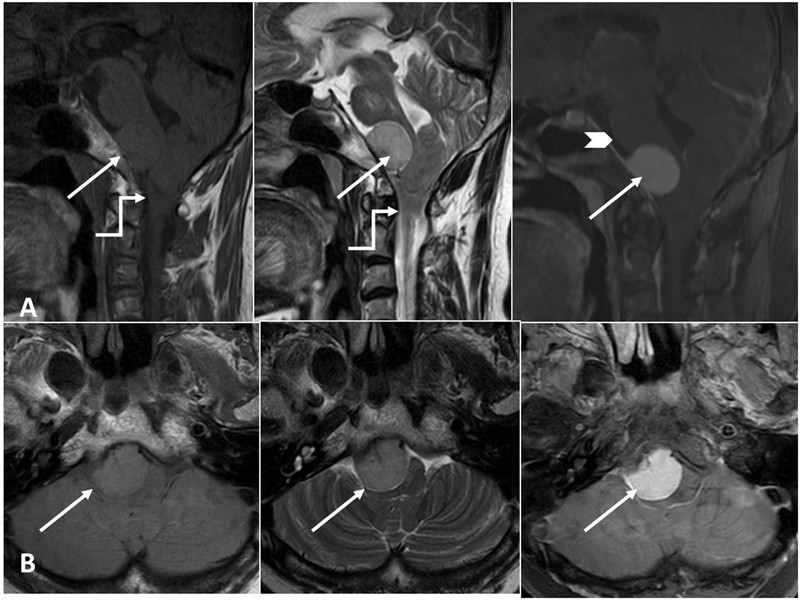
Fig. 7.
Alt Text: MRI of tuberculous osteomyelitis. Sagittal and axial T1W, T2W, and post-contrast T1 fat-saturated images show abnormal signal in clivus, atlas, and odontoid process with a peripherally enhancing prevertebral abscess (arrow) and cord compression (elbow arrow).
Benign Tumors
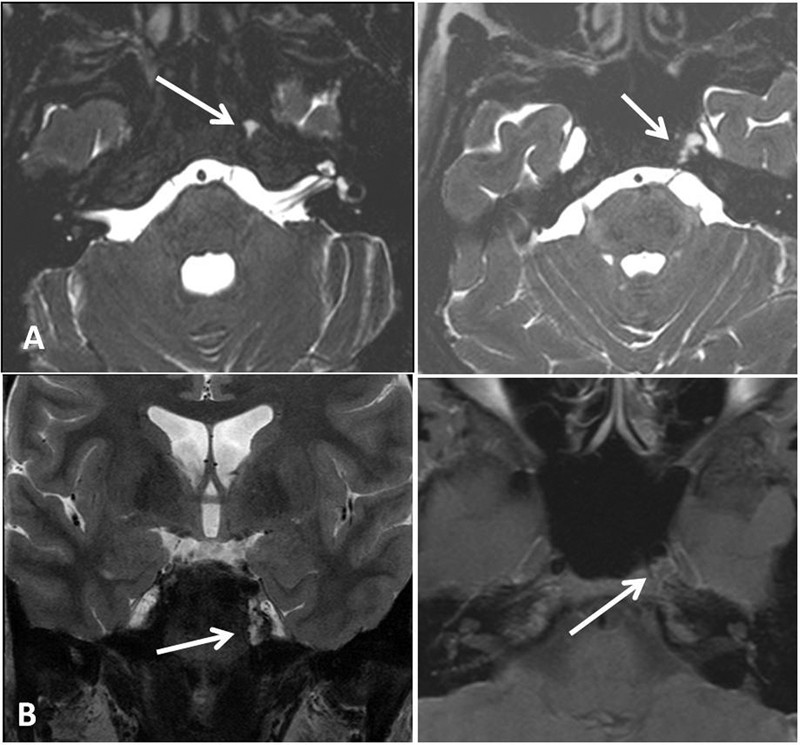
Enchondroma
Enchondromas are rare benign cartilaginous tumors of the skull base. CT shows hyperdense lesions with calcifications. MRI shows well-circumscribed lesions, heterogeneous T1 and mixed T2 signal (Fig. 8).
Differential Diagnosis
- Chondrosarcoma: Enchondromas are benign and well-defined, while chondrosarcomas show more aggressive features like bone destruction and soft tissue extension.
- Chordoma: Chordomas are midline and typically more aggressive with extensive bone destruction.
Fibrous Dysplasia (FD)
Clival FD is rare. CT shows sclerotic bone expansion with ground-glass density. MRI shows T1 hypointense and variable T2 signal with heterogeneous enhancement (Fig. 9).
Differential Diagnosis
- Paget’s disease: Paget’s is usually polyostotic and shows different phases, while FD is a developmental disorder.
- Osteoma: Osteomas are densely sclerotic lesions without the ground-glass matrix of FD.
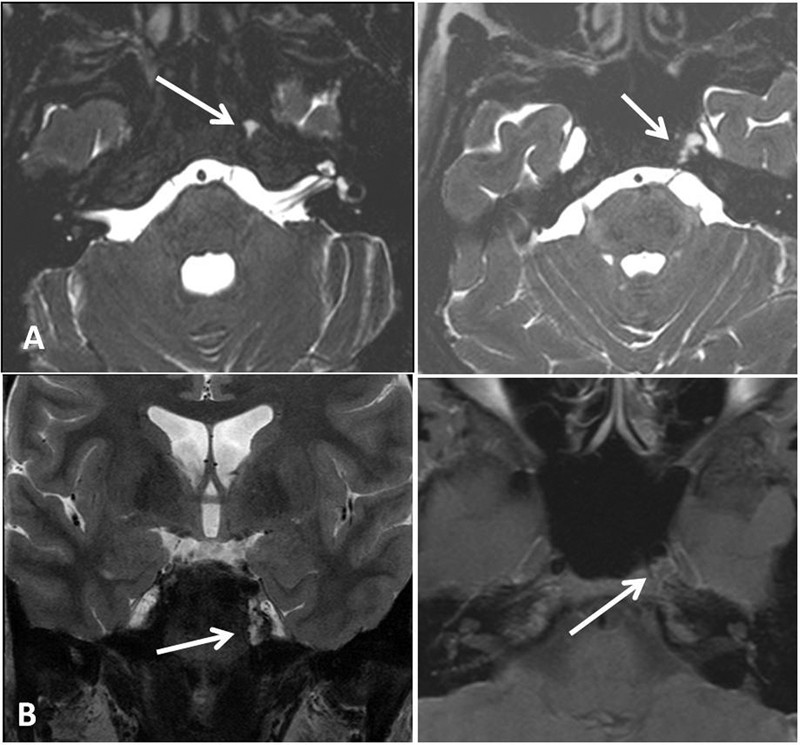
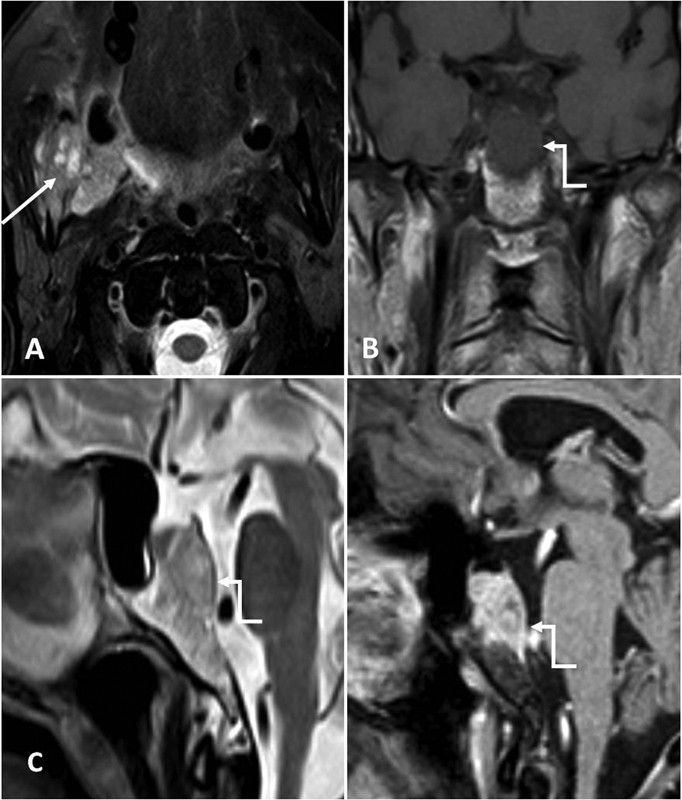
Aneurysmal Bone Cyst (ABC)
ABCs are benign osteolytic tumors, rare in the clivus. MRI shows characteristic fluid-fluid levels and septations (Fig. 10).
Differential Diagnosis
- Giant cell tumor (GCT): ABCs are cystic with fluid levels, while GCTs are solid and T2 hypointense.
- Telangiectatic osteosarcoma: Rare in the clivus, but also cystic. ABCs are benign and lack aggressive features.
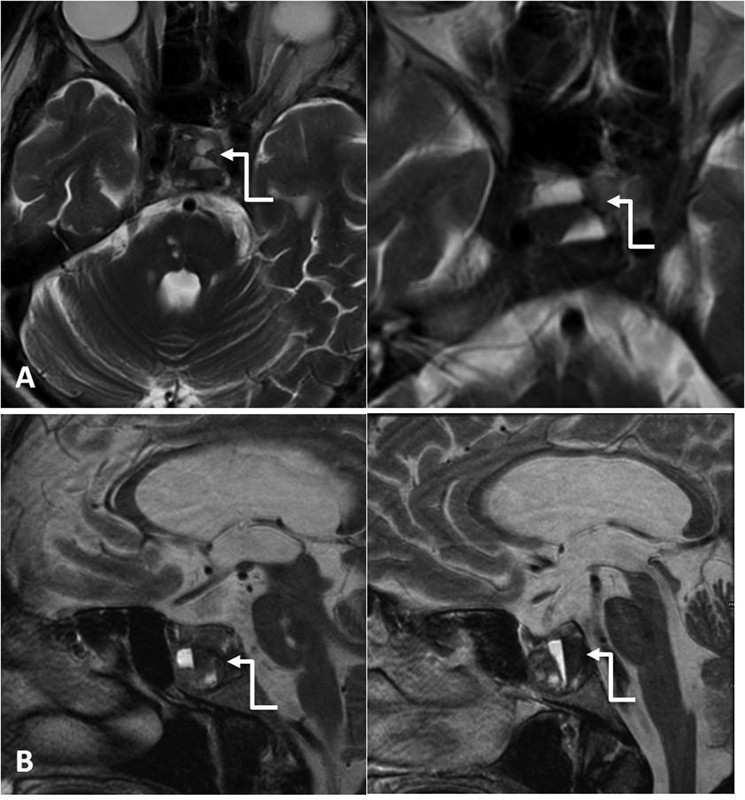
Giant Cell Tumor (GCT)
Clival GCTs are rare but aggressive benign tumors. CT shows expansile lytic lesions. MRI shows T2 hypointense solid lesions with homogeneous enhancement (Fig. 11).
Differential Diagnosis
- Plasmacytoma: Plasmacytomas can be T2 isointense but are often associated with multiple myeloma and lack the T2 hypointensity of GCT.
- Chondrosarcoma: Chondrosarcomas have chondroid matrix and calcifications, unlike GCTs.
Ecchordosis Physaliphora (EP)
EP is a benign notochordal remnant. CT shows well-defined hypodense lesions with sclerotic margins. MRI shows T1 hypointense, T2 hyperintense lesions without enhancement (Fig. 12).
Differential Diagnosis
- Chordoma: EPs are benign, intradural, and non-enhancing, while chordomas are malignant, extradural, expansile, and enhance.
- Mucocele: Mucoceles enhance peripherally if inflamed, while EPs do not enhance.
Paget Disease
Paget’s disease, a chronic bone disorder, can affect the clivus. Imaging findings vary with the disease phase. CT shows bone thickening and sclerosis in the blastic phase.
Differential Diagnosis
- Fibrous dysplasia: Paget’s is a remodeling disorder, while FD is a developmental abnormality.
- Metastatic disease: Metastases are usually destructive, while Paget’s involves bone remodeling and expansion.
Cholesteatoma
Cholesteatomas are epithelium-lined cysts. Clival cholesteatomas are rare. CT shows clival erosion. MRI shows T1 hypo to isointense, T2 hyperintense lesions, no enhancement, and high DWI signal (Fig. 13).
Differential Diagnosis
- Epidermoid cyst: Similar imaging but location and clinical context differ.
- Arachnoid cyst: CSF signal intensity on all sequences, unlike cholesteatomas.
Langerhans Cell Histiocytosis (LCH)
LCH is a rare cause of clival mass in children. It shows destructive lytic lesions, T2 hyperintense, T1 hypointense with enhancement.
Differential Diagnosis
- Eosinophilic granuloma: Solitary LCH lesion, part of the LCH spectrum.
- Metastasis: Considered in children with destructive bone lesions, but LCH has characteristic imaging and clinical features.
Fig. 8.
Alt Text: MRI of enchondroma. Axial CISS and coronal T2W and axial T1-post-contrast images show a lobulated extra-axial lesion at the petrosphenoid synchondrosis, compressing the 6th cranial nerve. T2 hyperintense lesion with heterogeneous post-contrast enhancement, classic for chondroid lesion.
Fig. 9.
Alt Text: Imaging of fibrous dysplasia. Axial CT (bone window) shows bony expansion with ground-glass matrix and sclerotic change in the left clivus. Axial T1-weighted MRI shows low T1 signal in the expanded bone, consistent with fibrous dysplasia.
Fig. 10.
Alt Text: MRI of aneurysmal bone cyst. Axial and sagittal T2-weighted images showing a cystic lesion with fluid-fluid levels (elbow arrows) involving the clivus.
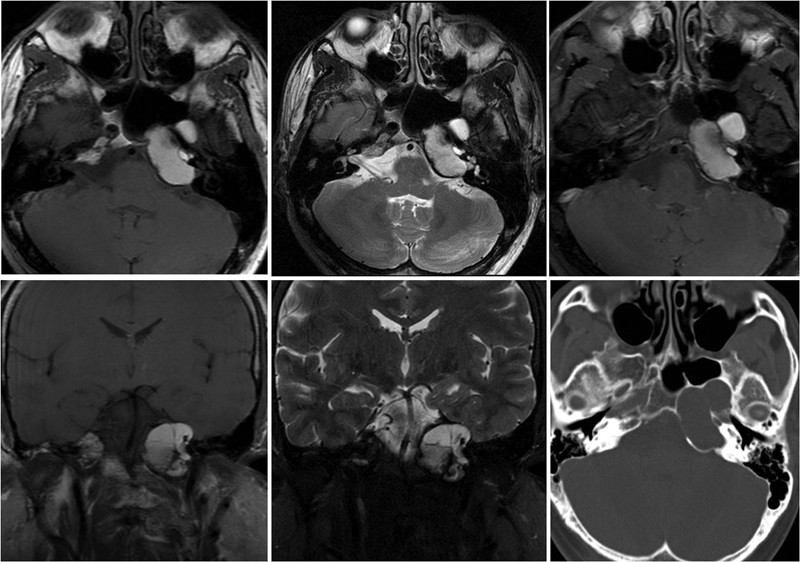
Fig. 11.
Alt Text: Imaging of giant cell tumor. Sagittal CT reformatted and axial post-contrast CT images show an expansile lytic lesion (arrows) in the clivus. Axial T1W, T2W, and post-contrast T1W images show a large T2 intermediate to hypointense mass (classic GCT signal) with enhancement and bony expansion.
Fig. 12.
Alt Text: Imaging of ecchordosis physaliphora. Sagittal CT (bone window), sagittal T1 noncontrast, sagittal T2WI, and sagittal T1+C images show a well-defined non-enhancing lesion (arrows) in the clivus, hypointense on T1W and hyperintense on T2W images.
Fig. 13.
Alt Text: MRI of congenital cholesteatoma. Axial T1W, T2W, and post-contrast and coronal T1W, T2W images show a well-defined expansile cystic lesion in the left petrous apex extending into the clivus, causing bone thinning, T1 and T2 hyperintense with no enhancement.
Primary Malignant Tumors
Chordoma
Chordomas are malignant tumors from notochordal remnants, typically midline clival lesions. CT shows expansile masses with bone destruction. MRI shows T1 hypointense and very T2 hyperintense lesions with heterogeneous “honeycomb” enhancement (Figs. 14 and 15).
Differential Diagnosis
- Chondrosarcoma: Chordomas are midline and very T2 bright, while chondrosarcomas are off-midline and less T2 bright with ring and arc calcifications.
- Ecchordosis physaliphora: Chordomas are expansile, destructive, and enhancing, unlike EPs.
Chondrosarcoma
Skull base chondrosarcomas arise from cartilage or bone. CT shows osteolytic lesions with ring and arc calcifications. MRI shows T1 iso to hypointense and T2 hyperintense lesions with heterogeneous enhancement (Fig. 16). They are typically off-midline.
Differential Diagnosis
- Chordoma: Chondrosarcomas are off-midline with ring and arc calcifications, unlike midline chordomas with “honeycomb” enhancement.
- Meningioma: Meningiomas are extra-axial, dural-based, and homogeneously enhancing, while chondrosarcomas are intraosseous.
Plasmacytoma and Multiple Myeloma (MM)
Plasmacytomas and MM involve plasma cell proliferation. Solitary clival plasmacytomas are rare. MRI shows T1 iso to hyperintense and T2 iso to hypointense lesions with enhancement (Fig. 17). CT shows osseodestructive lesions.
Differential Diagnosis
- Metastasis: Plasmacytomas can mimic metastases, but solitary plasmacytoma and MM have distinct clinical and hematologic features.
- Lymphoma: Lymphomas are typically T1 and T2 isointense/hypointense with restricted diffusion, unlike plasmacytomas.
Lymphoma
Primary skull base lymphoma is rare. MRI shows isointense or hypointense masses on T1W and T2W images with homogeneous enhancement and restricted diffusion.
Differential Diagnosis
- Plasmacytoma: Lymphomas show restricted diffusion and are more T2 hypointense, while plasmacytomas are more T1 hyperintense.
- Metastasis: Lymphomas are typically homogeneous, while metastases can be more heterogeneous and associated with systemic malignancy.
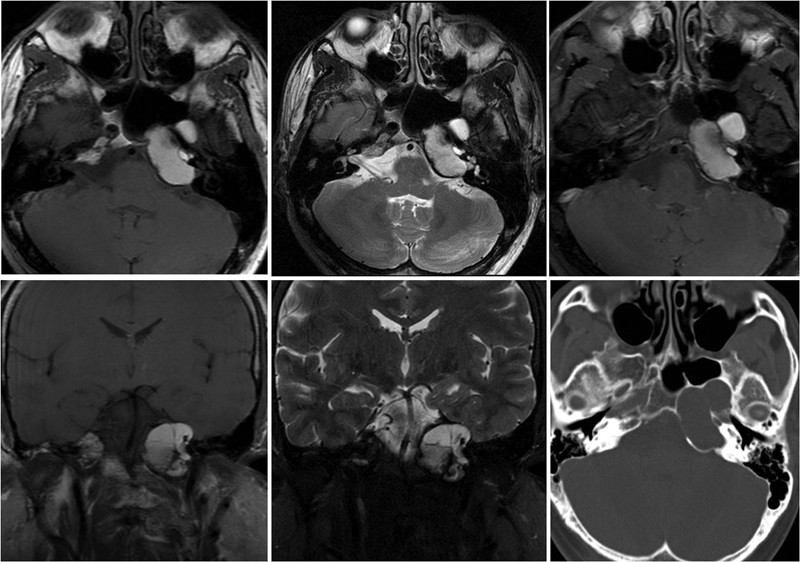
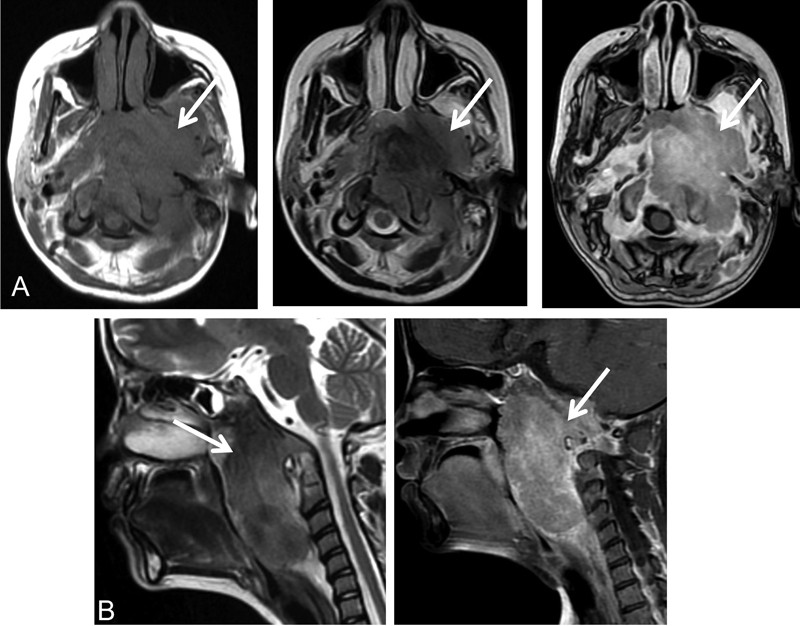
Fig. 14.
Alt Text: MRI of clival chordoma. Axial and coronal T1W and axial, coronal, and sagittal T2W images show a large midline intensely T2 hyperintense clival lesion (arrow), with posterior projection indenting the pons (“thumb sign,” elbow arrow).
Fig. 15.
Alt Text: MRI of clival chordoma. Axial T2W and sagittal T2W and post-contrast T1W images show an enhancing T2 heterogeneously hyperintense expansile lesion (arrow) with a hypointense thin peripheral sclerotic rim (arrowhead).
Fig. 16.
Alt Text: Imaging of clival chondrosarcoma. Sagittal CT reformatted (bone window) and axial post-contrast MRI T1-weighted images show a large expansile lobulated mass (arrows) in the basisphenoid region with peripheral lobular enhancement and ring and arc calcifications on CT.
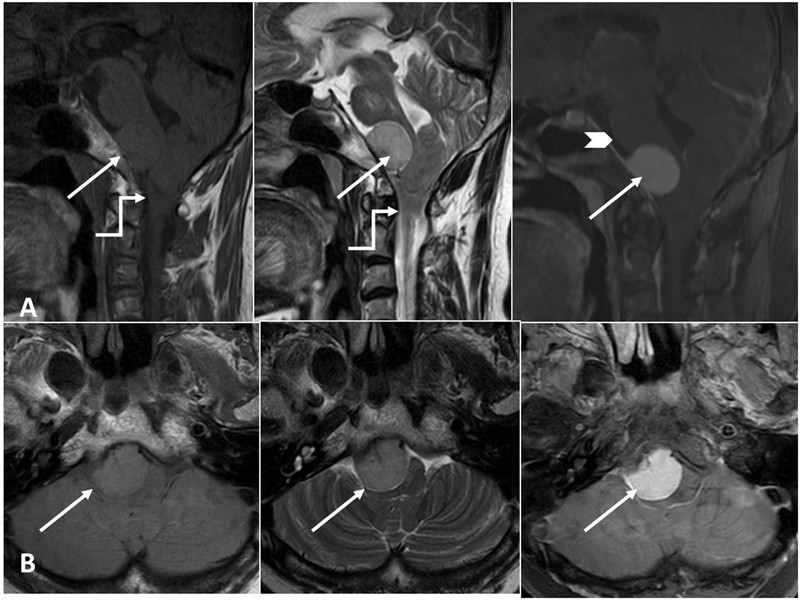
Fig. 17.
Alt Text: Imaging of clival plasmacytoma. Axial T1W, coronal and sagittal T2W MRI and CT images show abnormal marrow signal in the right clivus and petrous apex (arrows) and an expansile lytic lesion on CT (dotted arrows).
Metastatic Lesions
Clival Metastases
Clival metastases are rare, usually destructive bone lesions. MRI shows T1 isointense or hypointense, T2 hyperintense lesions with enhancement (Fig. 18).
Differential Diagnosis
- Plasmacytoma/MM: Metastases can mimic plasmacytoma, but clinical history of primary malignancy is crucial.
- Chordoma: Metastases are often more heterogeneous and less T2 bright than chordomas.
Fig. 18.
Alt Text: Imaging of clival metastasis. Axial STIR MRI shows a primary mass in the right buccal mucosa (arrow). Coronal T1W, sagittal T2W, and T1 post-contrast MRI images show an expansile lesion in the basisphenoid, T1 hypointense, T2 heterogeneously hyperintense with intense enhancement (elbow arrows).
Intracranial Tumors Invading Clivus
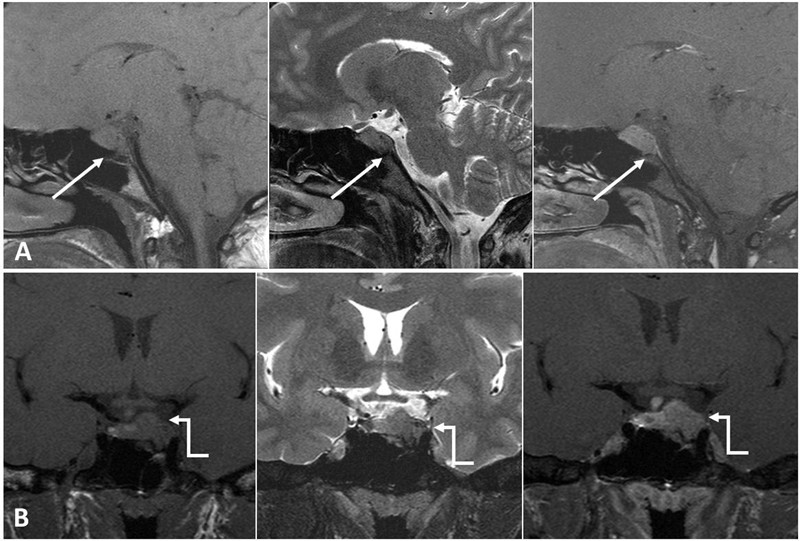
Invasive Pituitary Adenoma
Pituitary adenomas can invade the clivus. MRI shows pituitary mass extending into the clivus (Figs. 19 and 20).
Differential Diagnosis
- Craniopharyngioma: Also suprasellar, but craniopharyngiomas often have calcifications and cystic components.
- Meningioma: Meningiomas are extra-axial and dural-based, while pituitary adenomas arise from the pituitary gland.
Nasopharyngeal Carcinoma (NPC)
NPC can invade the clivus. Imaging shows nasopharyngeal mass extending to the clivus (Fig. 21).
Differential Diagnosis
- Lymphoma: NPC arises from nasopharyngeal epithelium, while lymphoma is a hematopoietic malignancy.
- Sarcoma: Rare nasopharyngeal sarcomas can also invade the clivus.
Meningioma
Meningiomas are common benign intracranial tumors that can invade the clivus. CT shows hyperdense lesions with homogeneous enhancement. MRI shows hypo to isointense T1 and T2 lesions with intense homogeneous enhancement and dural tail (Fig. 22).
Differential Diagnosis
- Schwannoma: Can occur in the cerebellopontine angle and extend to the clivus, but meningiomas are dural-based with dural tail.
- Chordoma/Chondrosarcoma: Meningiomas are extra-axial and homogeneously enhancing, while chordomas and chondrosarcomas are intraosseous and have different enhancement patterns.
Craniopharyngioma
Craniopharyngiomas, suprasellar masses from Rathke’s pouch, can involve the clivus.
Neuroendocrine Tumors and Paragangliomas
Neuroendocrine tumors and paragangliomas can also affect the clivus (Figs. 23 and 24). Paragangliomas show “salt and pepper” appearance on MRI and “moth-eaten” bone destruction on CT.
Differential Diagnosis
- Meningioma: Paragangliomas have characteristic “salt and pepper” appearance and are highly vascular, unlike meningiomas.
- Schwannoma: Paragangliomas are highly vascular and enhance intensely, while schwannomas may show cystic changes.
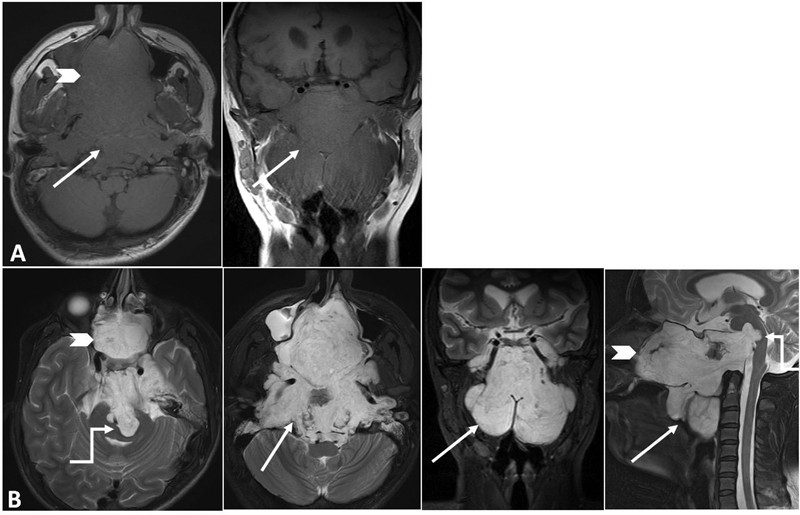
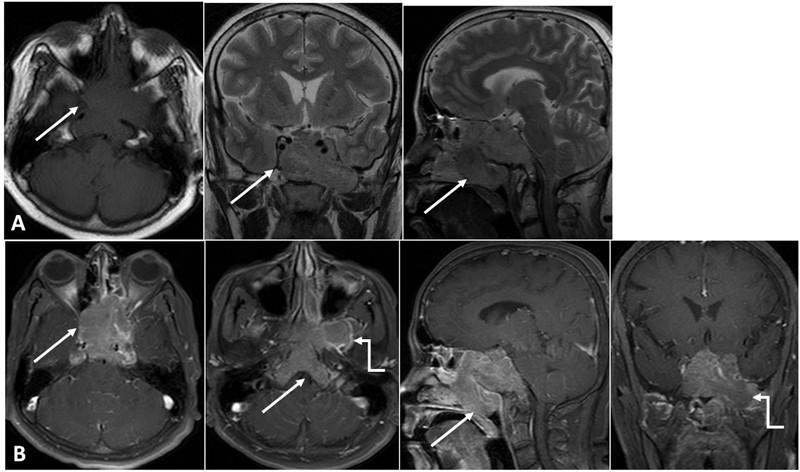
Fig. 19.
Alt Text: MRI of pituitary adenoma. Sagittal and coronal images show a pituitary mass (arrow) extending into the left cavernous sinus and eroding the sella turcica, extending up to the clivus.
Fig. 20.
Alt Text: MRI of invasive pituitary adenoma. T1 and post-contrast images of a partially resected pituitary macroadenoma, now presenting as a mass in the dorsum sellae and invading the entire clivus (arrow), showing homogeneous post-contrast enhancement.
Fig. 21.
Alt Text: MRI of nasopharyngeal carcinoma invading the clivus. Axial T1W, T2W, and post-contrast T1W and sagittal T2W and post-contrast T1W images show a large lobulated heterogeneously enhancing mass (arrows) in the nasopharynx extending to the clivus, eroding the sphenoid and atlas.
Fig. 22.
Alt Text: MRI of clival meningioma. Sagittal and axial T1W, T2W, and post-contrast T1 fat-saturated images show a well-defined homogenously enhancing extra-axial lesion (arrow) at the clivus, compressing the medulla, with a dural tail (arrowhead).
Fig. 23.
Alt Text: MRI of neuroendocrine tumor infiltrating the clivus. Axial T1W, coronal, and sagittal T2W and post-contrast fat-saturated images show a heterogeneous mass (arrow) involving the nasopharynx, clivus, sella, encasing carotid arteries, and extending into the pterygopalatine fossa (elbow arrow).
Fig. 24.
Alt Text: MRI of paraganglioma invading the clivus. Axial T2, axial post-contrast, and coronal T2-weighted fat sat MRI images show a large heterogeneously enhancing mass (arrow) involving the skull base and petrous apex, extending into the neck (dotted arrow), with a “salt and pepper” appearance (T2 bright foci and T2 hypointense flow voids).
Miscellaneous Conditions
Osteoradionecrosis (ORN)
ORN is a complication of radiation therapy, involving bone destruction. It can be difficult to differentiate from tumor recurrence.
Differential Diagnosis
- Tumor recurrence: Histological correlation is often needed to differentiate ORN from recurrent malignancy.
- Infection: ORN is non-infectious, but secondary infection can complicate diagnosis.
Table 4. Summary of Key Imaging Features for Differential Diagnosis
| Lesion | Key Imaging Features |
|---|---|
| 1. Chordoma | T2 very hyperintense, T1 iso to hypointense; Heterogeneous “Honeycomb” enhancement; Midline; Thumb sign; Chondroid variant: calcifications |
| 2. Chondrosarcoma | T2 hyperintense, T1 hypointense; Intense heterogenous enhancement; Off midline; Rings and arcs calcifications |
| 3. Ecchordosis physaliphora | T2 hyperintense, T1 hypointense; No post-contrast enhancement; Stalk like clival connection on high-resolution T2WI |
| 4. Fibrous dysplasia | Ground-glass density, ballooning, bone expansion, cortical thinning on CT |
| 5. Plasmacytoma | T1 iso to hyperintense; T2 iso to hypointense, post-contrast enhancement; Osseodestructive on CT; Solitary |
| 6. Lymphoma | Isointense or hypointense on T1W and T2W; Homogeneous enhancement; Restricted diffusion |
| 7. Giant cell tumor | T2 hypointense soft tissue lesion; Homogenous post-contrast enhancement |
| 8. Fungal infection | T2 hypointense (classically) |
| 9. Aneurysmal bone cyst | Multiple fluid levels and internal septations on MRI |
| 10. Cholesteatoma | High signal on DWI |
| 11. Meningioma | Hyperdense on noncontrast CT; Homogeneous enhancement; Hypo to isointense on T1W and T2W; Dural tail |
| 12. Paraganglioma | “Moth-eaten” bone destruction on CT; Intense enhancement; “Salt and pepper” pattern on T1W and T2W |
Alt Text: Table summarizing key imaging features of clival and paraclival lesions to aid in differential diagnosis, including signal intensities on MRI, enhancement patterns, CT findings, and specific characteristics like fluid levels or diffusion restriction.
Conclusion
The clivus is a complex anatomical region susceptible to a wide range of pathologies. Accurate diagnosis relies heavily on imaging, particularly CT and MRI. Understanding the specific imaging features of each entity is crucial for formulating a comprehensive differential diagnosis of clival lesions. This knowledge, while primarily for medical professionals, highlights the importance of systematic diagnostic approaches, a principle that resonates across various fields, including auto repair diagnostics at xentrydiagnosis.store. By appreciating the complexities of medical differential diagnosis, we can further sharpen our own diagnostic skills in the automotive domain.