Introduction
Congenital cloudy cornea, or corneal opacity present at birth or shortly thereafter, represents a significant diagnostic and therapeutic challenge in pediatric ophthalmology. The etiology of a cloudy cornea in newborns and infants is broad, encompassing a spectrum of conditions from relatively benign to vision-threatening. Accurate and timely differential diagnosis is paramount, as it dictates appropriate management strategies and significantly impacts visual prognosis. This article delves into the complexities of Cloudy Cornea Differential Diagnosis, drawing upon a compelling case study to illustrate key diagnostic considerations and therapeutic approaches. We aim to provide a comprehensive overview that enhances understanding for ophthalmologists and eye care professionals encountering this challenging clinical scenario.
Unraveling the Etiology: A Wide Spectrum of Causes
The differential diagnosis of cloudy cornea in infants is extensive, necessitating a systematic approach to identify the underlying cause. Several categories of conditions can manifest as congenital corneal opacities, including:
- Birth Trauma: Forceps delivery or vacuum extraction can result in Descemet’s membrane rupture and corneal edema, leading to transient clouding.
- Sclerocornea: A non-progressive developmental anomaly where the cornea is opaque and resembles sclera, often bilateral and associated with other ocular and systemic anomalies.
- Peter’s Anomaly: A spectrum of anterior segment dysgenesis characterized by central corneal opacity, iridocorneal adhesions, and sometimes lens abnormalities.
- Infections: Intrauterine infections such as TORCH (Toxoplasmosis, Other agents, Rubella, Cytomegalovirus, Herpes simplex) can cause keratitis and corneal clouding.
- Inflammation: Congenital corneal dystrophies can present with early-onset corneal edema and clouding.
- Congenital Glaucoma: Elevated intraocular pressure at birth can lead to corneal edema and enlargement (buphthalmos), causing corneal cloudiness.
- Metabolic Disorders: Mucopolysaccharidoses and other storage diseases can result in corneal clouding due to stromal deposition.
- Corneal Dystrophies: Congenital Hereditary Endothelial Dystrophy (CHED), Congenital Hereditary Stromal Dystrophy (CHSD), and Posterior Polymorphous Dystrophy are primary corneal disorders that can manifest with congenital cloudiness.
- Dermoids: Congenital corneal masses that can cause localized or diffuse corneal opacity.
- Cornea Plana: A rare condition characterized by a flattened cornea, which can sometimes appear cloudy.
- Oculo-Auriculo-Vertebral Dysplasia (Goldenhar-Gorlin Syndrome): A syndrome involving craniofacial and ocular abnormalities, including corneal opacities.
- Congenital Corneal Ectasia: Rare conditions where the cornea protrudes abnormally, potentially leading to clouding.
Differentiating between these conditions requires a meticulous clinical evaluation, often supplemented by ancillary investigations.
Case Presentation: Navigating the Diagnostic Pathway
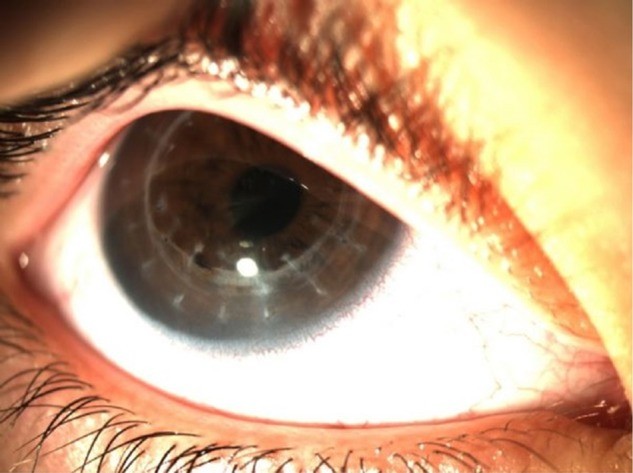
We present the case of a 4-year-old girl who presented to our cornea clinic with a history of bilateral cloudy cornea noted since birth. Her parents reported blurry vision since infancy. Upon examination, her visual acuity was counting fingers at 1 meter in both eyes. Slit-lamp biomicroscopy revealed diffuse corneal cloudiness bilaterally (Figure 1A, B). Intraocular pressure was within normal limits (14 mmHg OD, 13 mmHg OS), and central corneal thickness was measured at 692 µm OD and 684 µm OS using ultrasound pachymetry. Corneal diameter was 11 mm in both eyes. Neurological examination was unremarkable, and there was no evidence of strabismus or nystagmus at the time of initial presentation. Specular and confocal microscopy were not feasible due to the corneal opacity. Systemic examination was normal, with no other reported health issues.
Alt text: Preoperative slit-lamp images of the right and left eyes of a 4-year-old girl with congenital cloudy cornea, showing diffuse bilateral corneal opacity.
A significant finding in the patient’s history was a strong family history of bilateral poor vision. Further examination revealed that the patient’s mother, an 8-year-old sister, and a newborn sister also exhibited bilateral corneal clouding. This positive family history strongly suggested a hereditary component to the corneal disease, narrowing the differential diagnosis towards congenital corneal dystrophies.
Initial Diagnostic Hypothesis and Intervention
Based on the clinical presentation, particularly the bilateral congenital corneal cloudiness and positive family history, a preliminary diagnosis of Congenital Hereditary Endothelial Dystrophy (CHED) was considered. CHED is a known cause of congenital corneal opacity, and its hereditary nature aligned with the family history in this case.
To address the visual impairment and to further refine the diagnosis, a penetrating keratoplasty (PK) was performed on the patient’s right eye in June 2012. During PK, the full thickness of the central cornea is replaced with donor corneal tissue. The excised recipient corneal tissue was submitted for histopathological examination to confirm the clinical diagnosis.
Pathological Re-evaluation and Diagnostic Shift
The pathology report provided a crucial turning point in the diagnostic process. Contrary to the initial clinical suspicion of CHED, the histopathological analysis revealed that the Descemet’s membrane (DM) and endothelium were healthy. Instead, the report indicated stromal fibrosis, consistent with Congenital Hereditary Stromal Dystrophy (CHSD). This finding underscored the critical role of pathological examination in accurately diagnosing cloudy cornea, especially when clinical features may be overlapping.
Following suture removal 14 months postoperatively, the best-corrected visual acuity (BCVA) in the right eye improved to 0.4 (20/50 Snellen equivalent), demonstrating successful visual rehabilitation after PK (Figure 2).
Refined Surgical Strategy: Embracing DALK
With the definitive diagnosis of CHSD established by pathology, the surgical approach for the left eye was reconsidered. Given that CHSD primarily affects the corneal stroma and spares the endothelium and Descemet’s membrane, a deep anterior lamellar keratoplasty (DALK) was deemed a more appropriate and less invasive alternative to PK.
DALK selectively replaces the diseased corneal stroma while preserving the patient’s own healthy endothelium and Descemet’s membrane. This approach offers several advantages over PK, including a reduced risk of endothelial rejection, faster visual rehabilitation, and potentially fewer long-term complications.
In February 2014, DALK was performed on the patient’s left eye. Intraoperatively, a “big bubble” technique was used to dissect the corneal stroma, and the Descemet’s membrane was confirmed to be transparent after stromal removal. A donor cornea with the Descemet’s membrane removed was then sutured onto the recipient bed.
Postoperatively, the left corneal graft was clear on the first day (Figure 3). Anterior segment optical coherence tomography (AS-OCT) confirmed graft transparency and Descemet’s membrane integrity (Figure 4). At the 3-month follow-up, BCVA in the left eye was also 0.4 (20/50 Snellen equivalent) with spectacle correction. Postoperative endothelial cell density was favorable in both eyes (1541 cells/mm² OD, 2358 cells/mm² OS) (Figure 5).
Alt text: Anterior segment optical coherence tomography (AS-OCT) scan of the left eye post-DALK, showing a well-integrated graft, clear interface, and intact Descemet’s membrane, confirming successful lamellar keratoplasty.
Discussion: Refining the Differential and Therapeutic Strategies
Congenital cloudy cornea presents a diagnostic challenge, requiring careful consideration of a broad differential. In this case, the initial clinical suspicion of CHED was reasonable given the bilateral presentation, congenital onset, and positive family history. However, the pathology report definitively shifted the diagnosis to CHSD.
Distinguishing between CHED and CHSD, as well as other causes of congenital corneal clouding, is crucial for appropriate management. While clinical features can provide clues, histopathological examination often provides definitive diagnostic information. In cases with a suspected primary stromal dystrophy and healthy endothelium, DALK offers a significant advantage over PK.
Congenital Hereditary Stromal Dystrophy (CHSD)
CHSD is a rare autosomal dominant corneal dystrophy characterized by bilateral, symmetric, and diffuse corneal cloudiness present at birth or shortly after. Corneal diameter and intraocular pressure are typically normal, while corneal thickness may be increased. The cloudy appearance is attributed to small opacities throughout the corneal stroma. Our patient’s clinical and pathological findings were consistent with CHSD.
The Role of Keratoplasty in Pediatric Cloudy Cornea
Keratoplasty remains the primary treatment modality for visual rehabilitation in children with congenital cloudy cornea unresponsive to conservative measures. While PK has historically been the standard procedure, DALK and Descemet’s stripping automated endothelial keratoplasty (DSAEK) are increasingly recognized as valuable alternatives, particularly when the endothelium is healthy.
DALK, as utilized in the left eye of our patient, offers several benefits:
- Reduced Endothelial Rejection Risk: By preserving the recipient’s endothelium, the risk of endothelial graft rejection, a major cause of PK failure, is significantly diminished.
- Faster Visual Rehabilitation: DALK often allows for earlier suture removal and faster visual recovery compared to PK.
- Reduced Intraoperative and Postoperative Complications: DALK is an extraocular procedure, reducing the risk of sight-threatening complications associated with open globe surgery, such as endophthalmitis, expulsive choroidal hemorrhage, and retinal detachment.
Pathological Examination: A Cornerstone of Diagnosis
This case highlights the indispensable role of pathological examination of excised corneal tissue in the differential diagnosis of congenital cloudy cornea. In situations where clinical diagnoses are uncertain, or when surgical intervention is planned, pathological analysis can provide definitive diagnostic confirmation, guiding subsequent management and surgical strategies, as demonstrated by the shift from PK to DALK in our patient.
Conclusion: Optimizing Outcomes in Congenital Cloudy Cornea
Management of congenital cloudy cornea requires a comprehensive approach encompassing meticulous clinical evaluation, accurate differential diagnosis, and tailored surgical intervention. Pathological examination of corneal tissue is a critical tool in refining diagnoses and guiding surgical choices. While penetrating keratoplasty remains a valuable option, alternative keratoplasty techniques like DALK and DSAEK offer compelling advantages, particularly in cases where the corneal endothelium is healthy. By strategically employing these techniques and prioritizing accurate diagnosis, ophthalmologists can optimize visual outcomes and improve the quality of life for children with congenital corneal opacities.
Learning Points
- Differential diagnosis of cloudy cornea in infants is broad and requires systematic evaluation.
- Pathological examination of recipient corneal tissue is crucial for definitive diagnosis, especially in congenital corneal dystrophies.
- Deep anterior lamellar keratoplasty (DALK) is a valuable alternative to penetrating keratoplasty (PK) in pediatric patients with stromal corneal dystrophies and healthy endothelium, offering reduced risks and faster visual rehabilitation.
- Keratoplasty, including PK and DALK, remains the mainstay of treatment for visually significant congenital cloudy cornea, aiming to prevent amblyopia and improve visual function.
References
[1] Duke-Elder S, Wybar KC. System of ophthalmology. Vol III, Part 2. Congenital deformities. London: Henry Kimpton; 1963.
[2] Waring GO 3rd, Bourne WM, Edelhauser HF, Kenyon KR. Ultrastructural alterations of Descemet’s membrane in congenital hereditary endothelial dystrophy. Ophthalmology. 1978;85(3):244-77.
[3] Kenyon KR, Maumenee AE. The cornea in mucopolysaccharidosis. Birth Defects Orig Artic Ser. 1971;7(3):23-34.
[4] Traboulsi EI. Congenital corneal opacities. Saudi J Ophthalmol. 2012;26(3):295-301.
[5] Goldberg MF, McKusick VA. Cornea plana in siblings. Am J Ophthalmol. 1967;63(4):848-58.
[6] Baum JL, Feingold M. Ocular and systemic manifestations of Goldenhar-Gorlin syndrome. Am J Ophthalmol. 1973;75(2):250-7.
[7] Weiss JS, Moller HU, Aldave AJ, et al. IC3D classification of corneal dystrophies–edition 2. Cornea. 2015;34(2):117-59.
[8] Pearce WG, Walter MA, McKinnon CJ, et al. Congenital endothelial corneal dystrophy: clinical, pathological, and genetic aspects. Can J Ophthalmol. 1993;28(6):323-8.
[9] Sutphin JE, Tasman W. Pediatric ophthalmology. 3rd ed. Philadelphia: WB Saunders; 1997.
[10] Hittner HM, Friedlander M, Draeger J. Dominant congenital stromal dystrophy of the cornea. Arch Ophthalmol. 1976;94(9):1442-7.
[11] Waring GO 3rd, Rodrigues MM, Laibson PR. Congenital hereditary stromal dystrophy of the cornea. Am J Ophthalmol. 1978;86(6):717-27.
[12] Malbran ES, Ferrari JA, Suarez E. Corneal dystrophies: a clinical, pathological and genetic study of 84 families. Adv Ophthalmol. 1990;41:1-114.
[13] Kirkness CM, McCartney AC, Rice NS, Garner A. Congenital hereditary stromal dystrophy of the cornea–a clinicopathological study. Br J Ophthalmol. 1987;71(12):929-35.
[14] Dana MR, Schaumberg DA, Moyes AL, Gomes JA, Jones DM, Sugar J. Penetrating keratoplasty in children with congenital corneal opacities. Ophthalmology. 1996;103(5):716-23.
[15] Melles GR, Lander F, Rietveld FJ, Remeijer L, Beekhuis WH, Binder PS. Clinical application of cryopreserved donor cornea lenticules for lamellar keratoplasty. Br J Ophthalmol. 1999;83(6):747-51.
[16] Shimazaki J, Ishioka M, Tsubota K. Penetrating keratoplasty versus deep lamellar keratoplasty. Curr Opin Ophthalmol. 2002;13(4):217-21.
[17] Price FW Jr, Price MO. Descemet’s stripping with endothelial keratoplasty: comparative outcomes with penetrating keratoplasty. Arch Ophthalmol. 2006;124(4):449-56.