When you undergo a colonoscopy or surgery involving your colon, tissue samples are often sent to a pathologist for examination. This expert doctor specializes in diagnosing diseases by looking at body tissues. The pathologist’s findings are compiled into a pathology report, a crucial document that details the characteristics of your tissue sample. While a pathology report might sound intimidating, especially if you’re unfamiliar with medical jargon, understanding its key components can empower you to better grasp your health status. This article will focus on a particularly reassuring finding in a pathology report: “Colonic Mucosa With No Pathologic Diagnosis.” We will explore what this phrase means, why it’s good news, and how it fits within the broader context of a pathology report.
Decoding the Pathology Report: A Closer Look
Pathology reports can seem dense, but they follow a structured format to ensure clarity and comprehensiveness for healthcare providers. While the exact layout might vary slightly between labs, certain core elements are consistently included. Let’s break down the typical sections you’ll find in a pathology report, understanding how they contribute to the overall diagnosis, or in our focus, the absence of one – “colonic mucosa with no pathologic diagnosis.”
Essential Sections of a Pathology Report
-
Demographic Information: This section contains your personal details like name, date of birth, medical record number, and the referring doctor’s name. It ensures the report is correctly associated with you.
-
Procedure Description: This outlines the procedure performed to obtain the tissue sample, such as a colonoscopy with biopsy or a surgical resection. It also specifies the location from where the sample was taken within the colon.
-
Gross Description: This is a macroscopic examination of the tissue sample – what the pathologist observes with the naked eye. It includes details about the size, shape, color, and any notable features of the tissue. For instance, in a colon sample, it might describe the length of the colon segment and any visible masses or irregularities. Consider this example from a colon sample following a colectomy:
“Sample #1 is labeled ‘colon’ and consists of a segment of bowel measuring 13cm in length after fixation. The sample is surrounded by a moderate amount of pericolonic fat. 3cm from one resection margin is an ulcerated round tumor measuring 3.2cm in diameter. The rest of the mucosa is grossly unremarkable.”
This gross description provides an initial visual overview of the sample before microscopic examination.
-
Microscopic Description: This is where the pathologist meticulously examines the tissue sample under a microscope. This detailed analysis at a cellular level is crucial for identifying any abnormalities. The microscopic description focuses on the different layers of the colon and their cellular characteristics. To appreciate this better, let’s briefly understand the structure of the colon.
The colon, or large intestine, is a tubular organ approximately 5 to 6 feet long. It’s divided into sections: cecum, ascending, transverse, descending, and sigmoid colons, rectum, and anus. The colon wall itself is composed of several layers. Starting from the innermost layer and moving outwards, these are:
- Mucosa: The innermost lining of the colon, directly exposed to the contents of the digestive tract. It’s made up of the epithelium (surface lining cells), the lamina propria (connective tissue), and the muscularis mucosa (a thin muscle layer). The “colonic mucosa” in our keyword refers specifically to this innermost layer.
- Submucosa: A layer of connective tissue beneath the mucosa, containing blood vessels, lymphatic vessels, and nerves.
- Muscularis Propria: Two layers of muscle responsible for the contractions that move waste through the colon.
- Serosa: The outermost layer, a membrane that covers and protects the colon. Outside the serosa is adipose tissue (fat) containing lymph nodes and blood vessels.
Understanding these layers is vital for interpreting the microscopic description, particularly when assessing the depth of any abnormalities.
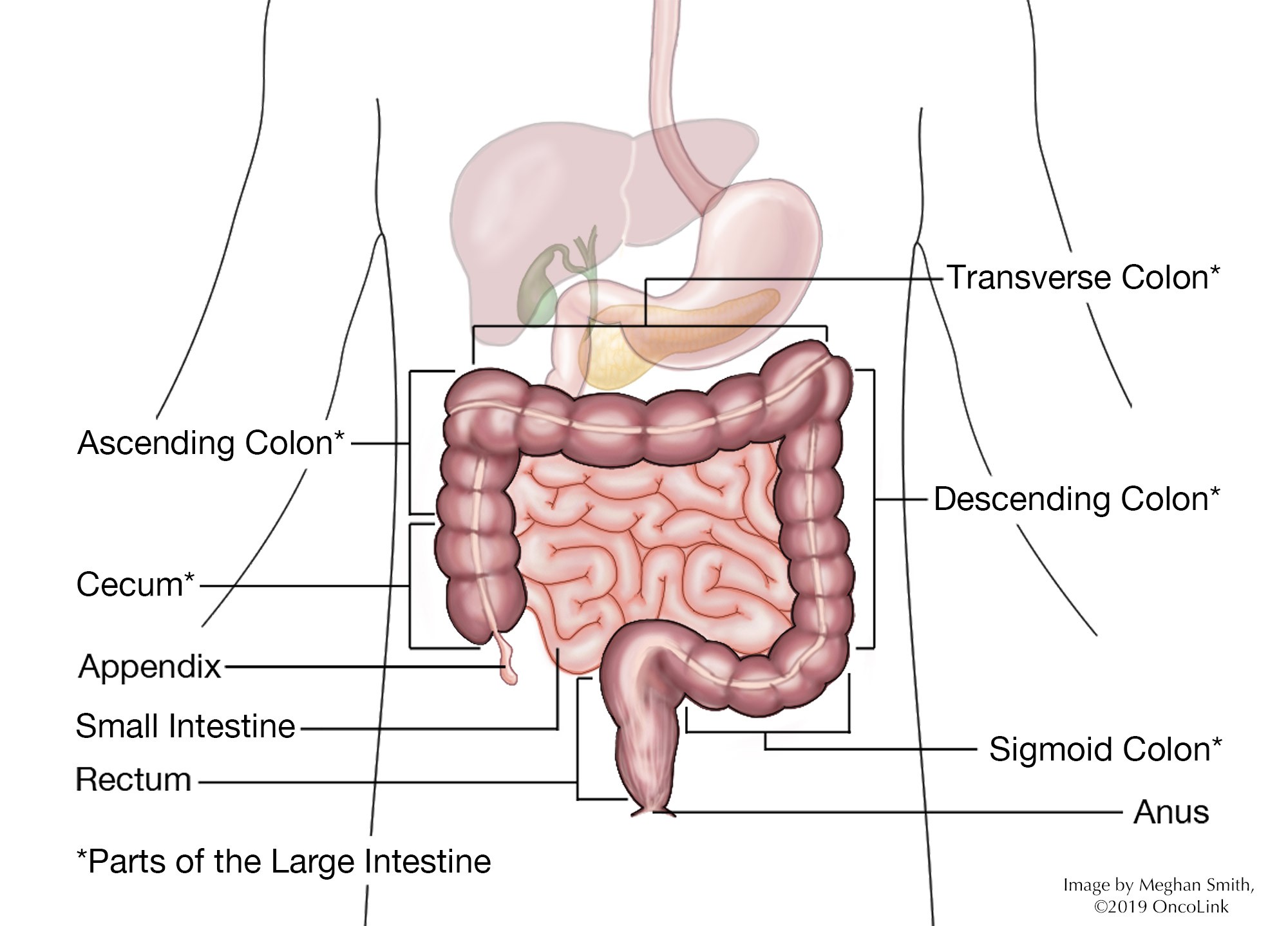 Diagram of colon anatomy
Diagram of colon anatomy -
Tumor Cell Type (If Applicable): If a tumor is present, this section identifies the specific type of cells that constitute the tumor. Adenocarcinoma is the most prevalent type of colon cancer, originating from the glandular cells lining the colon. Other less common types exist. However, in the context of “colonic mucosa with no pathologic diagnosis,” this section would essentially be absent or indicate “no tumor identified.”
-
Histologic Grade (If Applicable): For cancerous tumors, the histologic grade indicates how abnormal the tumor cells appear compared to normal cells. Grades range from well-differentiated (cells closely resemble normal cells) to undifferentiated (cells are highly abnormal and aggressive). Again, with a normal mucosa diagnosis, this is not relevant.
-
Lymphovascular Invasion (If Applicable): This assesses whether cancer cells have invaded blood vessels or lymphatic vessels, which can be a sign of more aggressive disease. This is not applicable when the diagnosis is “colonic mucosa with no pathologic diagnosis.”
-
T-stage (If Applicable): The T-stage describes the extent of tumor invasion into the colon wall and surrounding tissues. It ranges from T1 (innermost layer) to T4 (outermost layer and beyond). In a normal pathology report, this staging is irrelevant. Examples of T-stage descriptions in abnormal reports include:
- “The biopsy shows involvement of the mucosal lamina propria by neoplastic glands. The submucosa is not involved.” This tumor invades only the innermost layer of the colon (T1s)
- “The tumor invades through the muscularis propria but not into the pericolonic adipose tissue. The serosal surface is not involved.” This tumor invades the muscle layer but does not invade the serosa (the outer layer of the colon) or the surrounding fat (T2).
- “The tumor is invasive through the muscularis propria into the pericolonic fat.” This tumor has penetrated through the colon wall and into the surrounding fat (T3).
-
Lymph Nodes (If Applicable): If lymph nodes are removed during surgery, they are examined for cancer cells. The report states the number of lymph nodes examined and how many contain cancer. This section is not pertinent to a “no pathologic diagnosis” report on the mucosa itself.
-
Margins (If Applicable): In surgical resections, margins refer to the edges of the removed tissue. Pathologists check if cancer cells extend to the margins. Clear margins (no cancer cells at the edge) are desired. This is not relevant when the mucosa is diagnosed as normal.
-
Diagnosis: This is the culmination of the pathologist’s evaluation. It summarizes the findings and provides a formal diagnosis. In our case of interest, the diagnosis would be along the lines of “Colonic mucosa with no pathologic diagnosis,” “Benign colonic mucosa,” or “Negative for malignancy.” This is the key takeaway and the most reassuring part of the report.
“Colonic Mucosa with No Pathologic Diagnosis”: Understanding the Good News
Now, let’s focus specifically on our keyword phrase: “colonic mucosa with no pathologic diagnosis.” This is unequivocally good news. It means that when the pathologist examined the tissue sample from your colonic mucosa under the microscope, they found no evidence of disease or abnormality. In simpler terms, your colonic mucosa appears normal and healthy.
Let’s break down the components of this phrase to fully understand its meaning:
- Colonic Mucosa: As discussed earlier, this refers to the innermost lining of your colon. This is the tissue layer that is most often sampled during procedures like colonoscopies, as it’s the site where many colon conditions, including polyps and cancers, originate.
- No Pathologic Diagnosis: “Pathologic” refers to disease or abnormality. “Diagnosis” is the identification of a disease or condition. Therefore, “no pathologic diagnosis” means that the pathologist did not find any signs of disease or abnormality in the colonic mucosa sample.
What does “no pathologic diagnosis” exclude? This finding essentially rules out a range of concerning conditions within the mucosa itself, including:
- Cancer: The absence of a pathologic diagnosis means there is no evidence of cancerous or precancerous cells in the mucosal tissue examined. This is particularly reassuring regarding colon cancer, which often begins in the mucosa.
- Polyps (Neoplastic): Neoplastic polyps, such as adenomas and villous adenomas, are precancerous growths that arise from the mucosa. A “no pathologic diagnosis” suggests that no such polyps were identified in the sampled mucosa.
- Inflammation: While inflammation might be present in other parts of the colon (and might be noted separately in the report if relevant to the clinical context), “no pathologic diagnosis” concerning the mucosa typically implies no significant mucosal inflammation was detected in the biopsy sample itself. Conditions like ulcerative colitis and Crohn’s disease, which involve mucosal inflammation, would likely result in a different pathology diagnosis.
- Infection: Certain infections can affect the colonic mucosa. A normal pathology report suggests no evidence of infectious agents causing mucosal abnormalities in the examined sample.
Why is this finding reassuring? Receiving a pathology report stating “colonic mucosa with no pathologic diagnosis” is a positive outcome. It provides reassurance that, at least in the area sampled, your colon lining appears healthy. This can alleviate anxiety, especially if you underwent a colonoscopy or biopsy due to symptoms or screening recommendations.
Important Considerations:
While “colonic mucosa with no pathologic diagnosis” is excellent news, it’s important to keep the following points in mind:
- Sampling Limitations: A biopsy or even a surgical sample represents only a portion of your entire colon. While the sampled mucosa may be normal, it doesn’t guarantee that the entire colon is completely free of any potential issues. Colonoscopies are designed to visualize the entire colon, and biopsies are taken from areas of concern or for routine screening. However, very small lesions or abnormalities in unsampled areas could theoretically be missed.
- Clinical Context is Key: Pathology reports should always be interpreted in conjunction with your overall clinical picture, including your symptoms, medical history, and other test results. If you continue to experience concerning symptoms, even with a normal mucosal pathology report, it’s crucial to discuss these with your doctor. Further investigations or follow-up might be necessary depending on your individual situation.
- Focus on Mucosa: The phrase specifically refers to the colonic mucosa. The report might contain findings related to other layers of the colon wall or surrounding tissues. However, when focusing on “colonic mucosa with no pathologic diagnosis,” the positive interpretation primarily concerns the health of this innermost lining.
Conclusion: Embracing a Normal Pathology Result
Receiving a pathology report can be a source of anxiety for many individuals. However, encountering the phrase “colonic mucosa with no pathologic diagnosis” should bring significant relief. It signifies that the examined lining of your colon is healthy, without evidence of cancer, precancerous polyps, or significant inflammation in the sampled area. While it’s crucial to understand the limitations of any single test and to consider your overall health context, a normal mucosal pathology report is a decidedly positive finding. It underscores the importance of regular screenings and procedures like colonoscopies in monitoring and maintaining your colon health. Always discuss your pathology report and any health concerns with your healthcare provider for personalized guidance and peace of mind.