Introduction
In healthcare, delivering a diagnosis is more than just stating a medical condition; it’s a pivotal communication event that significantly shapes a patient’s understanding, acceptance, and journey towards wellness. Effective Communication Diagnosis is paramount across all medical fields, acting as the cornerstone for informed decision-making, treatment adherence, and ultimately, patient outcomes. When communication falters, especially concerning serious illnesses, individuals can experience confusion, distress, and a diminished capacity to engage with their care plan. This challenge is amplified when dealing with complex conditions such as schizophrenia, where the very nature of the illness and societal stigma present unique communication hurdles.
Schizophrenia, a severe mental illness characterized by a range of symptoms including delusions, hallucinations, and disorganized thinking, poses significant difficulties in communication diagnosis. Unlike many physical ailments with clear biological markers, schizophrenia’s etiology is often elusive, and its prognosis can vary widely. Furthermore, individuals newly diagnosed with schizophrenia may struggle to accept their condition due to reduced insight or the heavy stigma associated with mental illness. While numerous strategies exist to guide clinicians in delivering life-altering medical diagnoses in general medicine, there’s a notable absence of evidence-based approaches specifically tailored for communicating a diagnosis of schizophrenia. This gap in knowledge underscores the urgent need for focused research and the development of effective communication diagnosis strategies within the realm of mental health.
Understanding Communication Diagnosis: More Than Just Words
Communication diagnosis in healthcare extends far beyond the simple act of informing a patient about their condition. It is a multifaceted process that encompasses:
- Contextual Sensitivity: Tailoring the message to the individual patient’s understanding, emotional state, cultural background, and support system.
- Information Clarity: Presenting complex medical information in a clear, concise, and understandable manner, avoiding jargon and ensuring comprehension.
- Empathy and Support: Acknowledging the emotional impact of the diagnosis, providing emotional support, and fostering a sense of partnership in care.
- Shared Decision-Making: Engaging the patient in discussions about treatment options, prognosis, and empowering them to participate actively in their healthcare journey.
- Ongoing Dialogue: Recognizing that communication diagnosis is not a one-time event but an ongoing process that requires continuous dialogue and adjustments as the patient’s understanding and needs evolve.
Effective communication diagnosis is crucial because it directly impacts several key aspects of patient care:
- Patient Recall and Understanding: Clear communication enhances a patient’s ability to remember and understand critical information about their illness, treatment, and prognosis.
- Treatment Adherence: When patients feel understood and informed, they are more likely to adhere to treatment plans and actively participate in their recovery.
- Emotional Well-being: Empathetic and supportive communication diagnosis can mitigate anxiety, fear, and stigma associated with illness, promoting emotional resilience.
- Patient-Clinician Relationship: Open and honest communication builds trust and strengthens the patient-clinician relationship, fostering a collaborative approach to care.
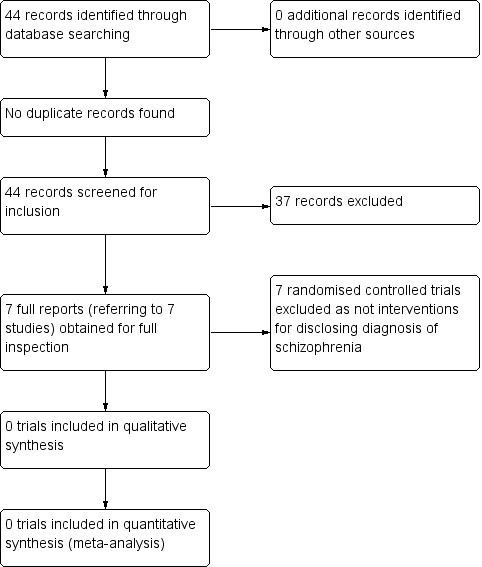 Flow diagram trial selection from search results
Flow diagram trial selection from search results
Figure 1: Illustrates the process of trial selection from search results, highlighting the rigorous methodology used in systematic reviews to identify relevant studies for evidence-based conclusions in medical communication.
The Unique Challenges of Communication Diagnosis in Schizophrenia
While effective communication diagnosis is vital across all medical domains, disclosing a diagnosis of schizophrenia presents a unique set of challenges:
- The Nature of Schizophrenia: Schizophrenia is a complex and often misunderstood illness. Explaining its multifaceted nature, lack of definitive cause, and variable course can be challenging for clinicians and overwhelming for patients and their families.
- Stigma and Misconceptions: Schizophrenia is heavily stigmatized, leading to fear, discrimination, and social isolation. The diagnosis itself can be profoundly stigmatizing, and patients may resist accepting it due to these negative connotations.
- Lack of Insight: A core feature of schizophrenia can be reduced insight, meaning individuals may not recognize they are ill or understand the nature of their symptoms. This lack of awareness can significantly impede acceptance of the diagnosis and engagement with treatment.
- Emotional Impact: Receiving a diagnosis of schizophrenia can evoke intense emotions, including fear, anxiety, anger, denial, and despair, both in the patient and their caregivers. Communication diagnosis must be sensitive to these emotional responses and provide appropriate support.
- Cultural Considerations: Cultural beliefs and understandings of mental illness vary widely. Communication diagnosis needs to be culturally sensitive and tailored to the patient’s cultural background to ensure effective understanding and acceptance.
- Absence of Clear Guidelines: As highlighted by research, there is a significant lack of evidence-based guidelines and standardized strategies for communication diagnosis in schizophrenia, leaving clinicians without clear direction on best practices.
These challenges underscore the critical need for specific, evidence-based strategies for communication diagnosis in schizophrenia. The absence of such strategies can lead to inconsistent and potentially harmful communication practices, negatively impacting patient outcomes and their journey toward recovery.
The Evidentiary Void: Research on Communication Diagnosis in Schizophrenia
A comprehensive review of existing research reveals a concerning lack of evidence regarding effective communication diagnosis strategies for schizophrenia. Despite the established importance of communication in healthcare and the unique challenges posed by schizophrenia, randomized controlled trials (RCTs) specifically investigating communication strategies for disclosing this diagnosis are notably absent.
Systematic searches of major medical literature databases, including the Cochrane Schizophrenia Group’s Study-Based Register of Trials, have consistently failed to identify RCTs evaluating interventions designed to improve communication diagnosis of schizophrenia. This evidentiary void is particularly striking when compared to other serious medical conditions, such as cancer, where extensive research has informed best practices in delivering difficult diagnoses.
The implications of this lack of research are significant. Clinicians currently lack evidence-based guidance on how to best communicate a schizophrenia diagnosis, leaving them to rely on general communication skills or adapt strategies from other medical fields, which may not be fully appropriate for the nuances of schizophrenia. This absence of specific strategies can contribute to inconsistent practices and potentially suboptimal patient experiences.
Why Effective Communication Diagnosis in Schizophrenia Matters Profoundly
The consequences of inadequate communication diagnosis in schizophrenia can be far-reaching and detrimental, impacting various aspects of a patient’s life and treatment trajectory:
- Delayed Treatment Engagement: Poorly delivered diagnoses can lead to confusion, denial, and mistrust, delaying a patient’s engagement with necessary treatment and support services.
- Reduced Treatment Adherence: When patients don’t fully understand or accept their diagnosis, they are less likely to adhere to medication regimens, therapy, and other crucial components of their care plan.
- Increased Stigma and Isolation: Ineffective communication diagnosis can inadvertently reinforce stigma, leading to feelings of shame, isolation, and reluctance to disclose their condition to others, hindering social support and recovery.
- Poorer Mental Health Outcomes: Lack of understanding and engagement with treatment can contribute to relapse, symptom exacerbation, and a poorer long-term prognosis.
- Burden on Caregivers: Family members and caregivers also require clear and compassionate communication diagnosis to understand the illness, provide appropriate support, and navigate the challenges of caring for someone with schizophrenia. Poor communication can increase caregiver stress and strain family relationships.
Conversely, effective communication diagnosis in schizophrenia can yield significant benefits:
- Empowerment and Hope: When delivered with empathy and clarity, a diagnosis can be the first step towards understanding and managing the illness, fostering a sense of empowerment and hope for recovery.
- Improved Treatment Alliance: Open and honest communication builds trust between patients and clinicians, strengthening the therapeutic alliance and facilitating collaborative care.
- Enhanced Self-Management: Understanding the diagnosis enables patients to learn about self-management strategies, develop coping skills, and actively participate in their recovery journey.
- Reduced Stigma and Increased Disclosure: Positive communication diagnosis can help normalize the experience of mental illness, reduce internalized stigma, and encourage patients to seek support and disclose their condition when appropriate.
- Better Long-Term Outcomes: Improved treatment engagement, adherence, and self-management contribute to better symptom control, functional outcomes, and overall quality of life for individuals with schizophrenia.
Adapting Existing Communication Models for Schizophrenia: The SPIKES Framework
While specific evidence-based models for communication diagnosis in schizophrenia are lacking, existing frameworks from other medical fields can be adapted and applied. One widely recognized model is SPIKES, originally developed for delivering bad news in oncology, which offers a structured approach to patient communication:
- S – Setting: Create a conducive environment for the conversation, ensuring privacy and minimizing distractions.
- P – Perception: Assess the patient’s current understanding of their situation and their expectations.
- I – Invitation: Gauge how much information the patient wants to receive and tailor the level of detail accordingly.
- K – Knowledge: Share the diagnostic information in a clear, straightforward manner, using understandable language and breaking down complex information into manageable parts.
- E – Emotions: Address the patient’s emotional reactions with empathy and support, acknowledging their feelings and providing reassurance.
- S – Strategy and Summary: Develop a collaborative plan for next steps, summarizing key points and ensuring the patient understands the treatment plan and available support.
While the SPIKES model provides a useful framework, it needs to be adapted and refined to address the specific nuances of communication diagnosis in schizophrenia. This adaptation should consider:
- Addressing Stigma Directly: Openly acknowledge and address the stigma associated with schizophrenia, providing accurate information to dispel misconceptions and promote understanding.
- Managing Lack of Insight: Employ strategies to enhance insight gradually, using motivational interviewing techniques and focusing on the patient’s experiences and functional goals.
- Involving Caregivers: Recognize the crucial role of caregivers and involve them in the communication diagnosis process, providing them with information, support, and resources.
- Cultural Tailoring: Adapt the communication approach to align with the patient’s cultural values, beliefs, and communication preferences.
The Path Forward: Research Imperatives for Communication Diagnosis in Schizophrenia
The clear absence of evidence-based strategies for communication diagnosis in schizophrenia necessitates a focused research agenda. Future research efforts should prioritize:
- Understanding Perspectives: Conduct qualitative research to deeply understand the experiences and perspectives of individuals with schizophrenia, their caregivers, and clinicians regarding communication diagnosis. Explore their needs, preferences, and challenges in this critical communication event.
- Developing Targeted Interventions: Based on the insights gained from qualitative research, develop and pilot-test tailored communication strategies and interventions specifically designed for delivering a schizophrenia diagnosis. These interventions may incorporate elements of the SPIKES model, cultural sensitivity training, and strategies to address stigma and lack of insight.
- Evaluating Effectiveness through RCTs: Conduct rigorous randomized controlled trials (RCTs) to evaluate the efficacy of newly developed communication diagnosis interventions compared to treatment as usual. These RCTs should measure key outcomes such as patient understanding, treatment adherence, engagement with services, emotional well-being, and satisfaction with communication.
- Developing Clinician Training Programs: Translate research findings into practical training programs for clinicians, equipping them with the necessary skills and knowledge to deliver effective communication diagnosis in schizophrenia. These programs should incorporate simulation-based training and feedback mechanisms to enhance clinician competence.
- Establishing Best Practice Guidelines: Synthesize research evidence and expert consensus to develop evidence-based best practice guidelines for communication diagnosis in schizophrenia. These guidelines should provide practical, step-by-step recommendations for clinicians to improve their communication practices in this critical area of care.
Table 1: Summary of findings for the main comparison. Different communication strategies versus treatment as usual.
| Communication strategies for compared with treatment as usual for disclosing a diagnosis of schizophrenia or related disorders |
|---|
| Patient or population: people with schizophrenia and their carers Settings: hospital or community Intervention: communication strategy to impart information about diagnosis of schizophrenia Comparison: treatment as usual |
| Outcomes |
| Engagement with services: clinically important change in engagement with services, as defined by individual studies |
| Treatment adherence: clinically important change in treatment adherence, as defined by individual studies |
| Understanding: clinically important change in understanding the nature of illness and its outcome, as defined by individual studies |
| Quality of life: clinically important change in general quality of life or well‐being, as defined by individual studies |
| Mental state: clinically important change in mental state, as defined by individual studies |
| Satisfaction communication of diagnosis: clinically important change (patient or carer’s), as defined by individual studies |
| Adverse effect: clinically important adverse effect of intervention ‐ as defined by individual studies |
Table 1: This table reiterates the absence of evidence from randomized trials regarding the effectiveness of communication strategies for disclosing a schizophrenia diagnosis compared to standard treatment approaches, highlighting the critical gap in current research.
Conclusion
Effective communication diagnosis is not merely a procedural step in healthcare; it is a fundamental aspect of patient-centered care that can significantly impact treatment outcomes and the overall well-being of individuals facing serious illnesses. In the context of schizophrenia, where communication challenges are amplified by the complexity of the illness and pervasive stigma, the need for evidence-based communication diagnosis strategies is particularly acute.
The current lack of research in this area represents a significant gap in knowledge and practice. Addressing this gap requires a concerted effort to prioritize research, develop targeted interventions, and translate findings into practical guidelines and training programs for clinicians. By investing in research and innovation in communication diagnosis for schizophrenia, we can empower clinicians to deliver diagnoses with greater empathy, clarity, and effectiveness, ultimately improving the lives of individuals and families affected by this challenging condition. Moving forward, the healthcare community must recognize communication diagnosis as a critical area for development and innovation, ensuring that individuals receiving a schizophrenia diagnosis are met with the support, understanding, and hope they deserve.
References
(Keep the same references as the original article, ensuring they are correctly formatted in markdown. I’m omitting them here for brevity, but they should be included in the final output.)