Nursing diagnosis is a cornerstone of patient care, serving as the critical second step in the nursing process. It’s more than just identifying a patient’s health problems; it’s a clinical judgment about individual, family, or community responses to actual or potential health conditions and life processes. This guide delves into the fundamental Components Of Nursing Diagnosis, providing a comprehensive understanding for healthcare professionals and nursing students alike.
What is Nursing Diagnosis? A Closer Look
At its core, a nursing diagnosis is a statement that describes a patient’s health condition from a nursing perspective. It’s formulated based on data gathered during a thorough nursing assessment and focuses on the patient’s response to illness, rather than the illness itself. It is a crucial step that enables nurses to create personalized care plans, select appropriate nursing interventions, and achieve specific patient outcomes for which they are accountable.
Nursing diagnoses are dynamic and patient-centered. They address a wide range of human responses, including physiological, psychological, sociological, and spiritual dimensions. By identifying these responses, nurses can tailor their care to meet the unique needs of each patient, promoting holistic and effective healthcare.
The Significance of Nursing Diagnosis
Nursing diagnosis plays a pivotal role in modern healthcare, serving several key purposes:
- Enhancing Critical Thinking: For nursing students, formulating nursing diagnoses is an invaluable exercise in developing problem-solving and critical thinking skills. It requires analyzing patient data, identifying patterns, and making informed judgments.
- Prioritizing Care: Nursing diagnoses help nurses prioritize patient needs. By clearly defining health problems, nurses can effectively allocate resources and direct interventions to the most pressing issues first.
- Guiding Nursing Interventions: A well-defined nursing diagnosis directly informs the selection of appropriate nursing interventions. It acts as a roadmap, guiding nurses in choosing actions that are most likely to achieve desired patient outcomes.
- Establishing Outcome Measures: Nursing diagnoses are essential for setting measurable and realistic patient outcomes. These outcomes are crucial for quality assurance, particularly for third-party payers who require evidence of effective and goal-oriented care.
- Holistic Patient Understanding: Nursing diagnoses encourage a holistic view of the patient. They prompt nurses to consider not just the disease, but also the patient’s overall response to their health condition, including their strengths and available resources.
- Facilitating Communication: Nursing diagnoses provide a standardized and common language for nurses and the entire healthcare team. This shared terminology ensures clear communication, reduces ambiguity, and promotes interprofessional collaboration.
- Evaluating Care Effectiveness: By establishing clear diagnoses and outcomes, nursing diagnoses provide a basis for evaluating the effectiveness of nursing care. This evaluation is vital for determining whether interventions were beneficial and cost-effective, driving continuous improvement in patient care.
Nursing Diagnosis vs. Medical Diagnosis vs. Collaborative Problems
It’s crucial to differentiate nursing diagnoses from medical diagnoses and collaborative problems. While all three are essential in patient care, they represent distinct perspectives and responsibilities.
Nursing Diagnosis: Focuses on the patient’s response to health conditions. It is within the scope of nursing practice and guides independent nursing interventions. For instance, a patient with pneumonia might have a nursing diagnosis of “Ineffective Airway Clearance related to increased mucus production as evidenced by abnormal breath sounds and cough.”
Medical Diagnosis: Identifies diseases or pathological conditions. It is made by physicians or advanced practitioners and dictates medical treatments. Using the same example, the medical diagnosis would be “Pneumonia.” Medical diagnoses guide medical interventions like medication prescriptions and surgical procedures.
Collaborative Problems: These are potential or actual health complications that require both medical and nursing interventions. Nurses monitor for these problems and implement interventions in collaboration with physicians. For a patient with pneumonia, a collaborative problem could be “Potential Complication: Sepsis,” requiring nurses to monitor vital signs, administer antibiotics as ordered, and collaborate with the physician on treatment strategies.
The key difference is the focus: nursing diagnoses address patient responses and guide nursing care, medical diagnoses identify diseases and direct medical treatment, and collaborative problems involve shared responsibility for managing complex patient issues.
Taxonomy of Nursing Diagnoses: Organizing and Classifying
To standardize and organize nursing diagnoses, various classification systems have been developed. The most widely recognized is NANDA-I (North American Nursing Diagnosis Association International) Taxonomy II. This taxonomy provides a hierarchical structure for classifying nursing diagnoses, promoting consistency and clarity in their use.
Taxonomy II is organized into 13 Domains, representing broad areas of human functioning, and 47 Classes, which are subdivisions within each domain. Nursing diagnoses are then categorized within these classes. This system moves away from earlier classifications based on Functional Health Patterns and instead uses a multi-axial system. The seven axes include:
- Diagnostic Concept: The core concept of the diagnosis (e.g., Airway Clearance).
- Time: The chronicity or acuity of the condition (e.g., Acute, Chronic).
- Unit of Care: The recipient of care (e.g., Individual, Family, Community).
- Age: The age group of the patient (e.g., Child, Adult, Elderly).
- Health Status: The patient’s overall health (e.g., Wellness, Risk, Actual).
- Descriptor: Additional qualifiers that specify the diagnosis (e.g., Ineffective, Impaired).
- Topology: The body part or location involved (e.g., Respiratory, Urinary).
Diagnoses in Taxonomy II are listed alphabetically by their diagnostic concept, simplifying the process of finding and selecting the appropriate diagnosis.
Domains and Classes within Taxonomy II:
- Domain 1. Health Promotion:
- Class 1. Health Awareness
- Class 2. Health Management
- Domain 2. Nutrition:
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Domain 3. Elimination and Exchange:
- Class 1. Urinary Function
- Class 2. Gastrointestinal Function
- Class 3. Integumentary Function
- Class 4. Respiratory Function
- Domain 4. Activity/Rest:
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy Balance
- Class 4. Cardiovascular/Pulmonary Responses
- Class 5. Self-Care
- Domain 5. Perception/Cognition:
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Domain 6. Self-Perception:
- Class 1. Self-Concept
- Class 2. Self-Esteem
- Class 3. Body Image
- Domain 7. Role Relationship:
- Class 1. Caregiving Roles
- Class 2. Family Relationships
- Class 3. Role Performance
- Domain 8. Sexuality:
- Class 1. Sexual Identity
- Class 2. Sexual Function
- Class 3. Reproduction
- Domain 9. Coping/Stress Tolerance:
- Class 1. Post-Trauma Responses
- Class 2. Coping Responses
- Class 3. Neurobehavioral Stress
- Domain 10. Life Principles:
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action Congruence
- Domain 11. Safety/Protection:
- Class 1. Infection
- Class 2. Physical Injury
- Class 3. Violence
- Class 4. Environmental Hazards
- Class 5. Defensive Processes
- Class 6. Thermoregulation
- Domain 12. Comfort:
- Class 1. Physical Comfort
- Class 2. Environmental Comfort
- Class 3. Social Comfort
- Domain 13. Growth/Development:
- Class 1. Growth
- Class 2. Development
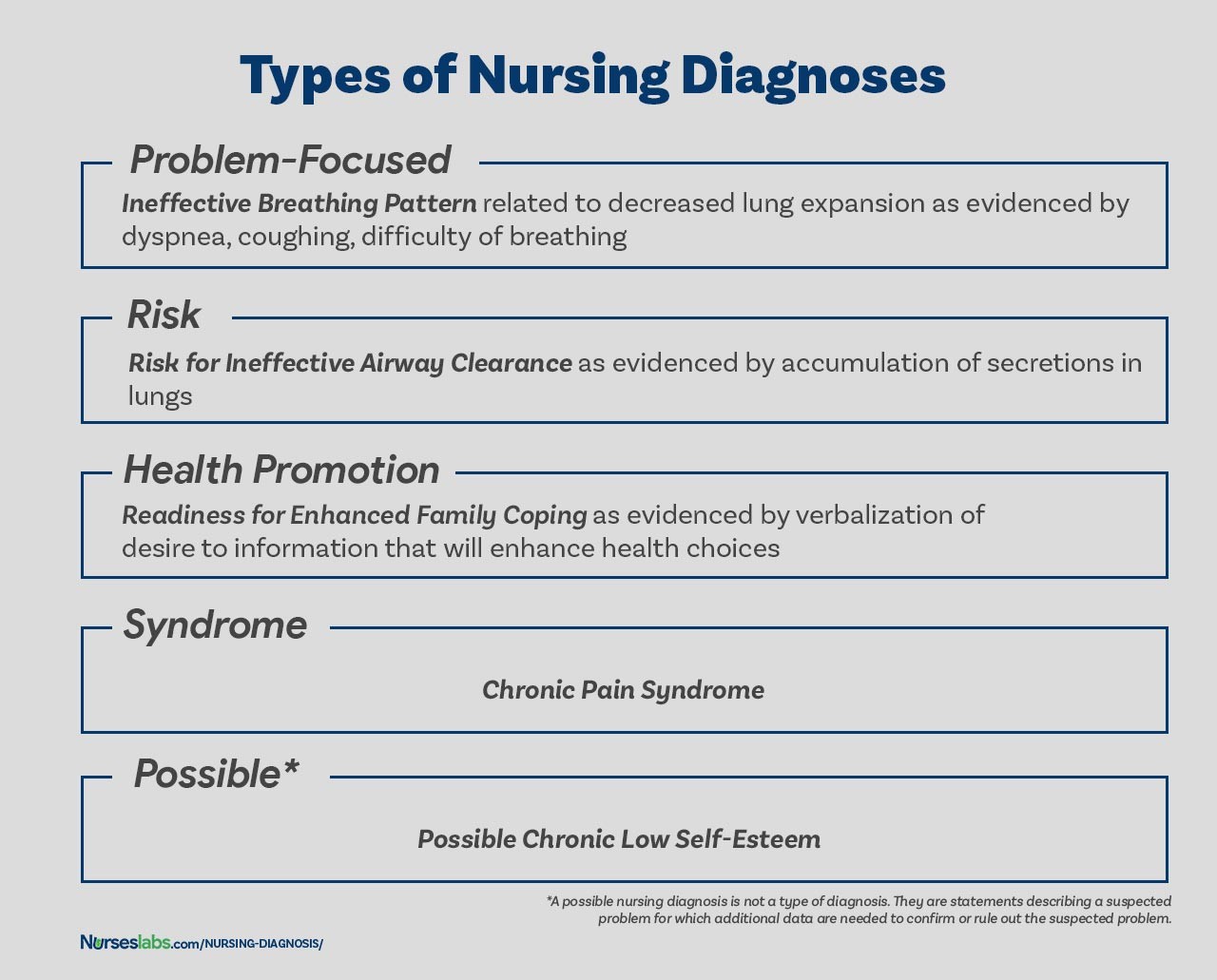
Types of Nursing Diagnoses: Categorizing Patient Needs
Nursing diagnoses are further categorized into four main types, each addressing different aspects of patient health:
-
Problem-Focused (Actual) Nursing Diagnoses: These diagnoses describe existing patient problems that are present at the time of assessment. They are supported by defining signs and symptoms. An example is “Acute Pain related to surgical incision as evidenced by patient report of pain at 7/10, guarding behavior, and increased heart rate.”
-
Risk Nursing Diagnoses: These diagnoses identify potential problems that a patient is at risk of developing. They are based on risk factors that increase vulnerability. For example, “Risk for Infection as evidenced by surgical incision, compromised immune system, and presence of invasive lines.”
-
Health Promotion Nursing Diagnoses: These diagnoses focus on a patient’s desire and motivation to improve their health and well-being. They highlight strengths and readiness to enhance wellness. An example is “Readiness for Enhanced Nutrition as evidenced by patient expressing interest in learning about healthy eating and requesting dietary information.”
-
Syndrome Nursing Diagnoses: These diagnoses are used when a cluster of actual or risk nursing diagnoses are likely to occur together due to a specific situation or event. An example is “Rape-Trauma Syndrome” which encompasses a range of potential diagnoses following sexual assault.
Dissecting the Components of a Nursing Diagnosis
A well-formulated nursing diagnosis typically comprises three essential components, particularly for problem-focused diagnoses. These components ensure clarity, accuracy, and guide effective care planning.
-
Problem (Diagnostic Label) and Definition: This component concisely describes the patient’s health problem or response. The diagnostic label is a standardized term from a recognized taxonomy like NANDA-I. It usually consists of two parts: the qualifier and the focus of the diagnosis.
- Qualifiers (Modifiers): Words that add specific meaning or detail to the diagnostic label (e.g., Deficient, Impaired, Ineffective, Risk for).
- Focus of the Diagnosis: The specific area of health concern (e.g., Fluid Volume, Gas Exchange, Tissue Perfusion, Injury).
For example, in “Deficient Fluid Volume,” “Deficient” is the qualifier, and “Fluid Volume” is the focus. Some diagnoses are single-word terms (e.g., Anxiety, Constipation) where the qualifier and focus are inherent.
Qualifier Focus of the Diagnosis Deficient Fluid volume Imbalanced Nutrition: Less Than Body Requirements Impaired Gas Exchange Ineffective Tissue Perfusion Risk for Injury 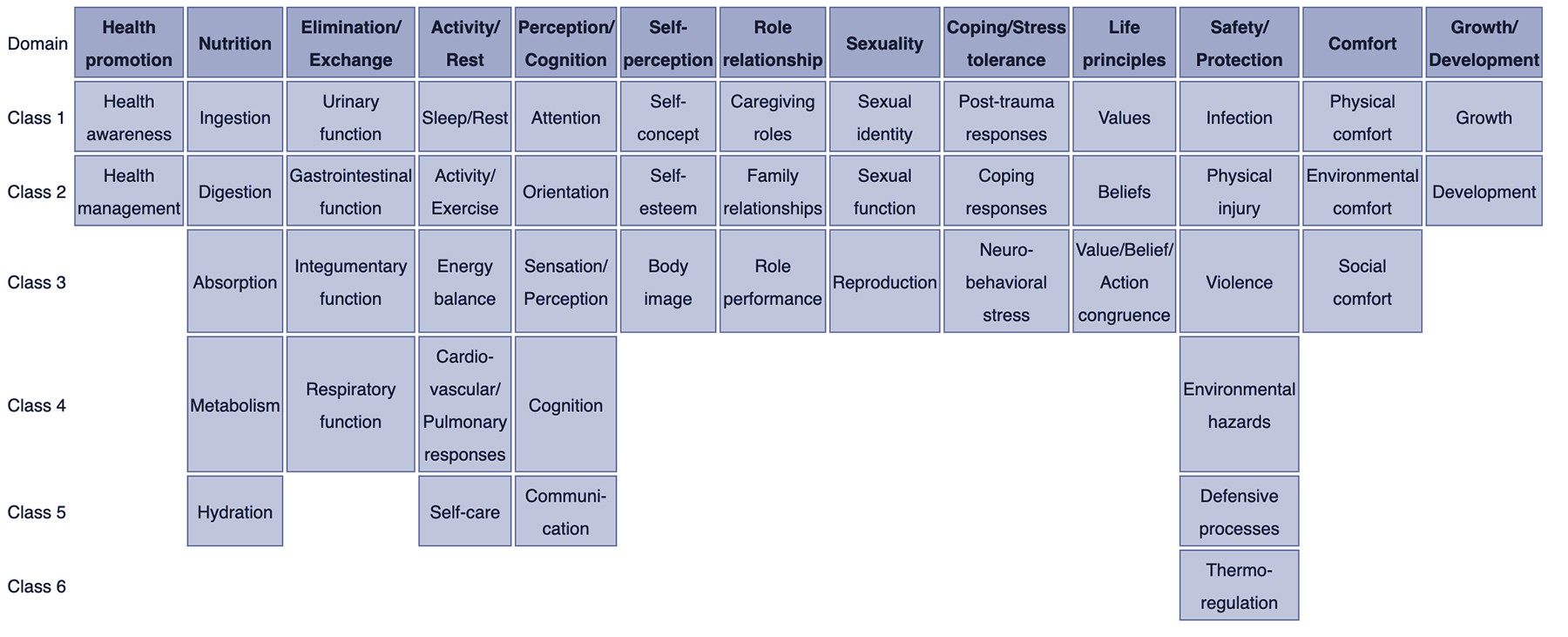
-
Etiology (Related Factors): This component identifies the probable cause(s) or contributing factors to the health problem. Etiology provides context and direction for nursing interventions. It is linked to the problem statement using the phrase “related to.” Effective nursing interventions aim to address these etiological factors to resolve the underlying cause of the diagnosis.
For example: “Impaired Physical Mobility related to musculoskeletal impairment.” Here, “musculoskeletal impairment” is the etiology contributing to the problem of impaired physical mobility.
-
Defining Characteristics (Signs and Symptoms) or Risk Factors: This component provides the evidence that supports the nursing diagnosis.
-
Defining Characteristics: For actual nursing diagnoses, these are the observable signs and symptoms that indicate the presence of the problem. They are linked to the problem and etiology using the phrase “as evidenced by” or “as manifested by.”
For example: “Acute Pain related to surgical incision as evidenced by patient report of pain at 7/10, guarding behavior, and increased heart rate.” The patient’s report of pain, guarding behavior, and increased heart rate are the defining characteristics.
-
Risk Factors: For risk nursing diagnoses, instead of defining characteristics, risk factors are identified. These are factors that increase the patient’s vulnerability to the potential problem. Risk factors are also linked using “as evidenced by.”
For example: “Risk for Falls as evidenced by history of falls, impaired mobility, and use of assistive devices.” History of falls, impaired mobility, and use of assistive devices are the risk factors for falls.
-
For health promotion and syndrome diagnoses, the components may be simpler, often consisting of just the diagnostic label or a one-part statement.
The Diagnostic Process: From Data to Diagnosis
Formulating a nursing diagnosis is a systematic process that involves three key phases:
-
Data Analysis: This initial phase involves examining the data collected during the nursing assessment. It includes:
- Comparing data against standards: Identifying deviations from normal or expected findings.
- Clustering cues: Grouping related data points to identify patterns.
- Identifying gaps and inconsistencies: Recognizing missing information or conflicting data that needs further investigation.
-
Identification of Health Problems, Risks, and Strengths: In this phase, nurses interpret the analyzed data to:
- Identify actual and potential health problems: Determine the specific nursing diagnoses that are supported by the data.
- Differentiate between nursing diagnoses, medical diagnoses, and collaborative problems: Ensure the identified problems fall within the scope of nursing practice.
- Recognize patient strengths and resources: Identify factors that can be leveraged to promote health and coping.
-
Formulation of Diagnostic Statements: The final phase involves crafting clear and concise nursing diagnostic statements using the appropriate format (PES or two-part for risk diagnoses). This includes selecting the correct diagnostic label, identifying related factors or risk factors, and listing defining characteristics where applicable.
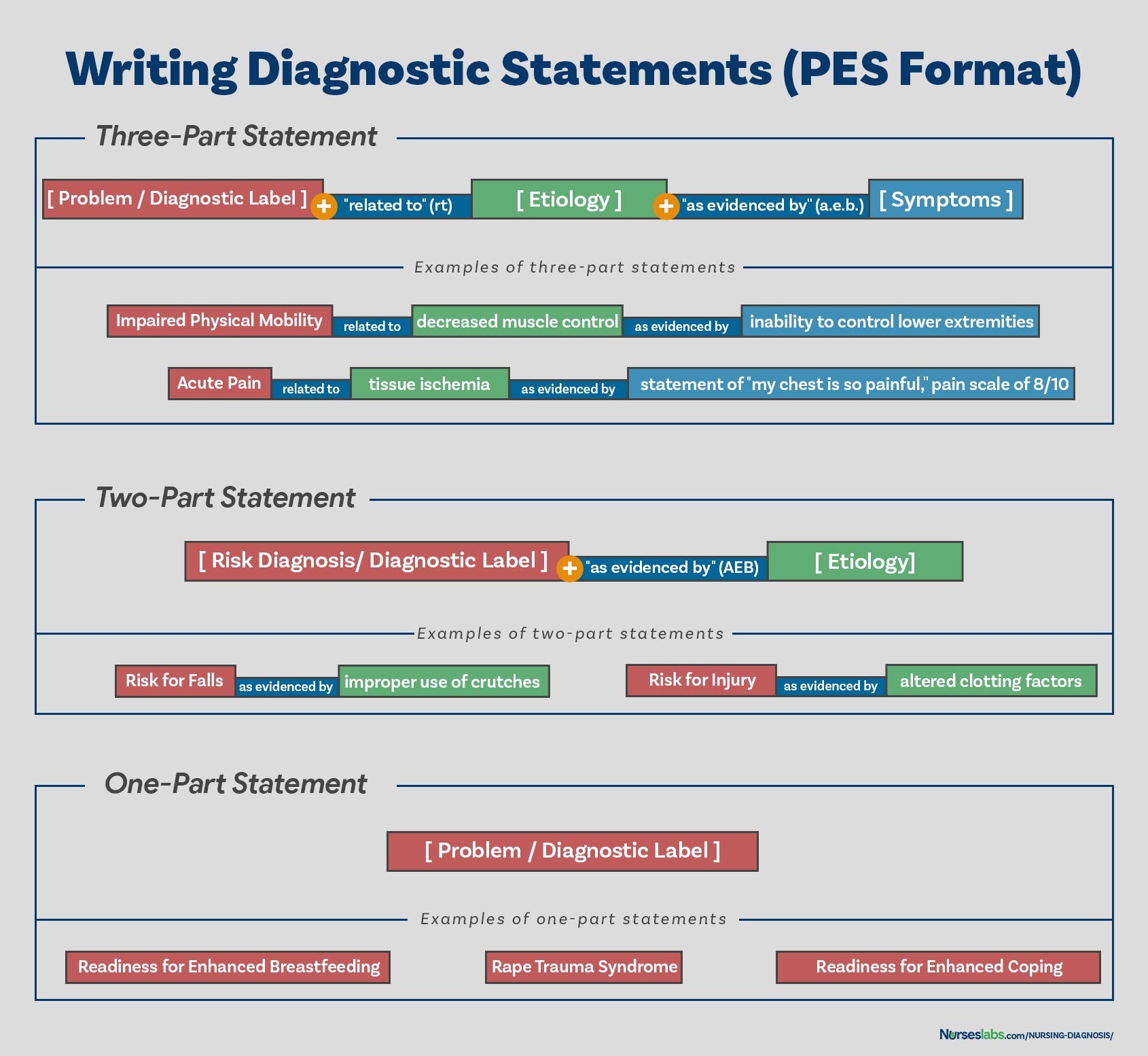
Writing Effective Nursing Diagnostic Statements
Writing clear and accurate nursing diagnostic statements is crucial for effective communication and care planning. The PES format is a widely used method for structuring these statements, particularly for problem-focused diagnoses.
PES Format Breakdown:
- P – Problem (Diagnostic Label): This is the NANDA-I approved diagnostic label that concisely describes the patient’s health problem.
- E – Etiology (Related Factors): These are the factors contributing to or causing the problem, linked by “related to.”
- S – Signs and Symptoms (Defining Characteristics): These are the observable cues that validate the presence of the problem, linked by “as evidenced by.”
Examples of PES Statements:
- Problem-Focused (Actual): “Constipation related to decreased physical activity and inadequate fluid intake as evidenced by reported infrequent bowel movements, abdominal distention, and hard, dry stools.”
- Risk: “Risk for Infection as evidenced by surgical incision and compromised immune system.” (Two-part statement, as signs and symptoms are not yet present).
- Health Promotion: “Readiness for Enhanced Knowledge related to diabetes management.” (One-part statement, as related factors are inherent in the desire for improvement).
- Syndrome: “Rape-Trauma Syndrome.” (One-part statement, as it’s a recognized cluster of diagnoses).
Variations in Statement Formats:
While PES format is common for problem-focused diagnoses, other types may use different formats:
- One-part statements: Often used for health promotion and syndrome diagnoses, focusing on the diagnostic label.
- Two-part statements: Typically used for risk and possible diagnoses, including the diagnostic label and risk factors or suspected problem.
Nursing Diagnoses: The Foundation of Nursing Care Plans
Nursing diagnoses are not just labels; they are the foundation upon which comprehensive nursing care plans are built. Each nursing diagnosis guides the development of specific interventions and expected outcomes tailored to the patient’s unique needs. By accurately identifying and articulating patient problems through nursing diagnoses, nurses can deliver targeted, effective, and patient-centered care.
Recommended Resources for Further Learning:
To deepen your understanding and skills in nursing diagnosis, consider exploring these highly recommended resources:
- Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: This handbook provides an evidence-based approach to nursing interventions and offers a step-by-step system for client assessment, nursing diagnosis, and care planning.
- Nursing Care Plans – Nursing Diagnosis & Intervention: Offering hundreds of care plans based on the latest evidence-based guidelines, this book is an invaluable tool for developing comprehensive care strategies.
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: A quick-reference guide that helps identify correct diagnoses and plan efficient patient care, including the most recent nursing diagnoses and interventions.
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: This manual assists in planning, individualizing, and documenting care for a wide range of conditions, offering sample clinical applications and prioritized interventions for each diagnosis.
- All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health: This comprehensive resource includes care plans across various specialties, familiarizing users with interprofessional patient problem approaches.
By mastering the components of nursing diagnosis and utilizing these resources, nurses can significantly enhance their ability to provide high-quality, patient-centered care, contributing to improved patient outcomes and a more effective healthcare system.
References:
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.