Conjunctival cysts are benign, fluid-filled sacs that develop on the conjunctiva, the clear membrane covering the white part of the eye and the inner surface of the eyelids. While often asymptomatic, they can sometimes cause discomfort, redness, or a foreign body sensation, prompting patients to seek medical attention. Establishing an accurate diagnosis is crucial for appropriate management, and this necessitates a thorough understanding of the Conjunctival Cyst Differential Diagnosis. This article aims to provide a comprehensive overview of the differential diagnoses to consider when evaluating a patient presenting with a suspected conjunctival cyst, drawing upon a relevant case study and expanding on the various clinical entities that can mimic this common ocular lesion.
Understanding Conjunctival Cysts and Their Etiology
Conjunctival cysts are broadly classified into two main types: retention cysts and inclusion cysts. Retention cysts, also known as mucous cysts, arise from the blockage of conjunctival glands or ducts, leading to the accumulation of secretions. Inclusion cysts, on the other hand, typically result from the entrapment of conjunctival epithelium following trauma, surgery, or inflammation.
Several factors can contribute to the development of conjunctival cysts. These include:
- Inflammation: Chronic inflammatory conditions of the conjunctiva, such as allergic conjunctivitis or dry eye syndrome, can predispose individuals to cyst formation.
- Trauma: Surgical procedures, accidental injuries, or even minor trauma to the conjunctiva can lead to the development of inclusion cysts.
- Topical Medications: Paradoxically, certain topical medications, particularly those containing preservatives, have been implicated in conjunctival cyst formation, as highlighted in the case report below.
- Idiopathic: In many instances, the exact cause of a conjunctival cyst remains undetermined, and they are considered idiopathic.
Case Report: Drug-Induced Conjunctival Cyst
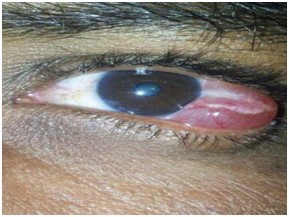
A 34-year-old male presented with a one-year history of swelling in the lateral bulbar conjunctiva of his left eye, accompanied by redness. He reported chronic eye irritation for which he had been using over-the-counter anti-allergic eye drops containing chlorpheniramine maleate, naphazoline hydrochloride, benzalkonium chloride (BAK), and hypromellose for a year without consulting an ophthalmologist. Initially, the drops provided symptom relief, but the irritation recurred, and he noticed a gradually enlarging swelling in his left eye.
Clinical examination revealed a well-defined, firm, immobile, non-tender limbal nodule measuring approximately 5mm x 4mm. The nodule was excised, and histopathological examination revealed a conjunctival cyst. Microbiological analysis showed needle-shaped crystals, identified as BAK crystals, within the cyst. Postoperative follow-up showed no recurrence. The diagnosis was determined to be a drug-induced conjunctival cyst secondary to chronic use of preservative-containing eye drops.
[Table/Fig-1]:
This case underscores the potential for topical ophthalmic medications, particularly those with preservatives like BAK, to contribute to conjunctival cyst formation. Chronic exposure to preservatives can disrupt the conjunctival epithelium and lead to the development of cysts.
Conjunctival Cyst Differential Diagnosis: Mimicking Conditions
While conjunctival cysts are often readily identifiable, several other ocular surface lesions can present similarly, necessitating a comprehensive differential diagnosis. When evaluating a patient with a suspected conjunctival cyst, it is crucial to consider and rule out the following conditions:
Benign Conjunctival Lesions
- Pinguecula: A pinguecula is a yellowish, raised conjunctival degeneration typically located in the interpalpebral fissure, adjacent to the cornea. Unlike cysts, pingueculae are solid lesions and do not contain fluid. They are often associated with sun exposure and aging.
- Pterygium: A pterygium is a wing-shaped fibrovascular growth of the conjunctiva that extends onto the cornea. It is also related to sun exposure and can cause irritation, redness, and blurred vision if it encroaches on the visual axis. Pterygia are solid and vascularized, distinguishing them from cysts.
- Conjunctival Nevus: A conjunctival nevus is a benign melanocytic tumor that can appear as a pigmented or non-pigmented lesion on the conjunctiva. Nevi are solid and may have varying degrees of pigmentation and vascularity.
- Dermoid Cyst (Limbal Dermoid): Limbal dermoids are congenital benign tumors that typically present at the limbus, the junction between the cornea and sclera. They are solid, yellowish-white lesions that may contain hair or sebaceous glands.
- Lymphatic Cyst (Lymphangioma): Conjunctival lymphangiomas are rare, benign tumors of lymphatic vessels. They can appear as clear, fluid-filled vesicles, but are often multiloculated and may have a “cluster of grapes” appearance, differing from the typical solitary conjunctival cyst.
- Inclusion Cyst (Epithelial Inclusion Cyst): While inclusion cysts are a type of conjunctival cyst, the differential diagnosis may involve distinguishing them from other cystic lesions. True epithelial inclusion cysts are often post-traumatic or post-surgical and arise from epithelial implantation.
Inflammatory and Infectious Conditions
- Phlyctenular Keratoconjunctivitis: Phlyctenules are small, nodular inflammatory lesions that can occur on the cornea or conjunctiva. Conjunctival phlyctenules appear as elevated, reddish nodules surrounded by hyperemia. They are associated with hypersensitivity reactions, often to staphylococcal bacteria or tuberculosis.
- Nodular Episcleritis: Episcleritis is inflammation of the episclera, the tissue layer between the conjunctiva and sclera. Nodular episcleritis presents with localized, raised, and tender nodules, often with overlying conjunctival redness. Episcleritis nodules are deeper and scleral-based, unlike superficial conjunctival cysts.
- Conjunctival Granuloma: Granulomas are nodular lesions resulting from chronic inflammation, often due to infectious (e.g., tuberculosis, sarcoidosis) or non-infectious causes. Conjunctival granulomas are solid, firm lesions that may be associated with systemic disease.
Neoplastic Lesions (Less Common Mimics)
- Conjunctival Papilloma: Conjunctival papillomas are benign epithelial tumors that can present as fleshy, wart-like growths on the conjunctiva. They are typically caused by human papillomavirus (HPV) and are solid lesions.
- Squamous Cell Carcinoma or Melanoma of the Conjunctiva: While less common, malignant conjunctival tumors such as squamous cell carcinoma and melanoma can occasionally mimic benign lesions. These are typically more irregular, vascularized, and may show rapid growth or other concerning features. Suspicion for malignancy should be raised with atypical or rapidly progressing lesions, necessitating biopsy.
Diagnostic Approach to Conjunctival Cysts
The diagnosis of a conjunctival cyst is often clinical, based on slit-lamp biomicroscopy. Key features to assess include:
- Location: Limbal, bulbar, or tarsal conjunctiva.
- Appearance: Size, shape, color, presence of fluid, mobility, and consistency.
- Vascularity: Conjunctival cysts are typically avascular, while vascularity may suggest other lesions like pterygia or neoplasms.
- Symptoms: Patient complaints such as irritation, redness, foreign body sensation, or discharge.
- History: History of trauma, surgery, topical medication use, or underlying systemic conditions.
In most cases, the characteristic appearance of a thin-walled, fluid-filled sac on the conjunctiva is sufficient for diagnosis. However, if there is diagnostic uncertainty, atypical features, or suspicion of other pathology, further investigations may be warranted:
- Excisional Biopsy and Histopathology: Excision of the cyst and histopathological examination are often performed for definitive diagnosis, especially if there are atypical features or concerns about malignancy. Histopathology can confirm the cystic nature of the lesion and rule out other conditions. As seen in the case report, it can also identify specific components like BAK crystals.
[Table/Fig-2]:
[Table/Fig-3]:
- Microbiological Analysis: In cases of suspected infection or drug-induced cysts, microbiological analysis of cyst contents or biopsy specimens may be helpful to identify causative organisms or substances, as demonstrated by the BAK crystal identification in the reported case.
[Table/Fig-4]:
Conclusion
Conjunctival cysts are common benign lesions of the ocular surface. While often easily recognized, a thorough understanding of the conjunctival cyst differential diagnosis is essential to accurately distinguish them from other mimicking conditions, ranging from benign lesions like pingueculae and pterygia to inflammatory conditions and, less commonly, neoplastic lesions. A careful clinical examination, consideration of patient history, and, when necessary, histopathological and microbiological investigations are crucial for accurate diagnosis and appropriate management, ensuring optimal patient care and avoiding unnecessary interventions or delayed treatment of more serious conditions. The presented case highlights the importance of considering drug-induced etiologies, particularly in patients with a history of chronic topical medication use, and reinforces the need for judicious use of preserved eye drops.
References
[1] No authors listed. Adverse effects of topical antiglaucoma medications. Side Effects of Drugs Annual. 1996;19:173-88.
[2] Baudouin C. Side effects of antiglaucoma drugs. Curr Opin Ophthalmol. 1996 Apr;7(2):61-9.
[3] Burstein NL. Ocular preservative cytotoxicity: Fluorophotometric studies of corneal permeability and cell damage. Invest Ophthalmol Vis Sci. 1984 Jun;25(6):726-32.
[4] Wilson WS, Duncan AJ, Jay JL. Effect of benzalkonium chloride on the rabbit corneal epithelium. An examination by scanning electron microscopy. Br J Ophthalmol. 1975 Dec;59(12):719-23.
[5] de Saint-Jean JP, Debbasch C, Brignole F, Warnet JM, Baudouin C. Induction of apoptosis and activation of inflammatory pathways by benzalkonium chloride in Chang conjunctival cells. Invest Ophthalmol Vis Sci. 1999 Feb;40(2):619-30.
[6] Baudouin C, Garcher C, Haouat N, Bron AM, Trautmann JC, Stegmann R, et al. Expression of inflammatory markers by conjunctival cells in chronically treated glaucoma patients. Ophthalmology. 1994 May;101(5):736-42.
[7] Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular surface damage after long-term glaucoma treatment. Br J Ophthalmol. 2004 Jul;88(7):908-12.
[8] Fechtner RD, Zinberg P, samples JR, Stewart JA, Holmes-Higgin DK, Liu JH, et al. Preservative-free tafluprost in patients with dry eye after discontinuation of preserved prostaglandin analogs. J Ocul Pharmacol Ther. 2011 Apr;27(2):151-7.
[9] Pauly A, Brignole-Guillemin F, Warnet JM, Baudouin C. Benzalkonium chloride induces proinflammatory and proapoptotic effects on Chang conjunctival cells. Invest Ophthalmol Vis Sci. 2009 Apr;50(4):1742-52.
[10] Tripathi BJ, Tripathi RC. Benzalkonium chloride as a preservative in ophthalmic preparations. Surv Ophthalmol. 1973 Jan-Feb;17(3):195-205.
[11] Green K, Bowman K, Cheeks L, Cottrell C. Cytotoxicity of ophthalmic preservatives. Toxicol Lett. 1983 Aug;18(1-2):169-75.
[12] Bernstein P, Wagh VK, Cohen S, Jones D, Zimmerman R, Katz IM. Toxicity of preservatives on immortalized human corneal epithelial cells. J Ocul Pharmacol Ther. 2003 Jun;19(3):205-13.
[13] Wright P. Adverse reactions to topical glaucoma therapy. Trans Ophthalmol Soc U K. 1984;103 ( Pt 4):449-51.
[14] Shields CL, Shields JA, White CL, Augsburger JJ. Conjunctival cysts in adults. Clinical features, histopathology, and management in 250 cases. Ophthalmology. 1995 Sep;102(9):1386-95.