Chronic Obstructive Pulmonary Disease (COPD) is a prevalent respiratory condition characterized by persistent breathing difficulties. However, patients diagnosed with COPD often experience acute episodes where their symptoms worsen, most notably dyspnea. These exacerbations of COPD (ECOPDs) are frequently accompanied by increased coughing, sputum production, and changes in sputum color. ECOPDs significantly diminish a patient’s quality of life, accelerate the decline of lung function, and elevate the risk of hospitalization and mortality. A concerning statistic is that approximately 20% of patients hospitalized for ECOPD are readmitted within just 30 days, placing a substantial burden on both individuals and healthcare systems. Mortality rates are also alarmingly high, with about 25% of patients dying within a year and 65% within five years following hospitalization for an ECOPD.
COPD patients are typically older and often present with multiple co-existing chronic conditions, including heart failure, coronary artery disease, arrhythmias, interstitial lung diseases, bronchiectasis, asthma, anxiety, and depression. Furthermore, they are at a greater risk of developing pneumonia, pulmonary embolism, and pneumothorax. These comorbidities not only increase the likelihood of subsequent ECOPDs but can also mimic or worsen the symptoms of an exacerbation. Crucially, a significant proportion—nearly 70%—of readmissions following hospitalization for an ECOPD are actually due to the decompensation of these other underlying health issues.
This underscores the critical need for clinicians to consider a broad Copd Differential Diagnosis when evaluating COPD patients presenting with worsening dyspnea, especially when the typical signs of an ECOPD are not clearly evident. A thorough investigation into these potential mimicking conditions is essential for accurate diagnosis and appropriate management. For the majority of these conditions, a detailed clinical assessment, supplemented by relevant diagnostic tests, can guide healthcare providers to a precise diagnosis. This article aims to consolidate the currently scattered information and offer a practical, systematic approach for clinicians managing COPD patients who present with worsening respiratory symptoms, particularly dyspnea. Adopting such a structured approach is expected to improve patient outcomes and reduce the personal and societal costs associated with ECOPDs.
Understanding the Mimics: Conditions in COPD Differential Diagnosis
The clinical course of COPD is often punctuated by acute episodes of respiratory symptom exacerbation, most prominently dyspnea. While these episodes are frequently diagnosed as ECOPDs, it is crucial to recognize that a variety of other conditions can mimic or complicate these exacerbations. A comprehensive copd differential diagnosis is therefore essential to ensure accurate patient management. Several categories of conditions should be considered when assessing a COPD patient presenting with worsening respiratory symptoms.
Cardiovascular Morbidities in COPD Differential Diagnosis
Cardiovascular diseases are highly prevalent in COPD patients and frequently contribute to respiratory distress. It’s vital to consider cardiac conditions in the copd differential diagnosis, as their symptoms can overlap with and exacerbate COPD symptoms.
Acute Heart Failure
Acute Heart Failure (HF) is a critical consideration in the copd differential diagnosis of patients presenting with respiratory distress. It is characterized by the rapid onset or worsening of symptoms and signs of heart failure, such as dyspnea at rest or with exertion, fatigue, and fluid retention. Distinguishing between acute HF and ECOPD can be challenging because many clinical features overlap. Notably, COPD is present in a significant proportion of HF patients, and conversely, HF is common in COPD patients due to shared risk factors like age and smoking, as well as common underlying mechanisms such as systemic inflammation.
Wheezing, a common symptom in ECOPD, is also observed in about 30% of acute HF cases, further complicating differentiation. Conversely, COPD may mask the presence of basilar crackles, a typical sign of HF. However, the presence of basilar crackles, coupled with peripheral edema, elevated jugular venous pressure, and a third heart sound, strongly suggests HF as the primary or contributing cause of acute respiratory symptoms.
Chest X-rays and laboratory markers play a crucial role in differentiating acute HF from ECOPD in the copd differential diagnosis. Cardiomegaly on chest X-ray supports structural heart damage and the likelihood of HF, especially if pulmonary edema is also present. Natriuretic peptides, such as brain natriuretic peptide (BNP) and N-terminal pro-brain natriuretic peptide (NT-proBNP), are valuable biomarkers for HF. Elevated levels support an HF diagnosis, with specific thresholds defined by cardiology guidelines. However, it’s important to note that natriuretic peptides can also be elevated in stable COPD and further increase during ECOPDs even without concomitant acute HF. Therefore, higher thresholds are needed to diagnose acute HF in the context of an ECOPD. Conversely, low natriuretic peptide levels have a high negative predictive value for acute HF, even in ECOPD patients. Point-of-care ultrasonography is also emerging as a helpful tool in differentiating between ECOPD and acute HF, although more research is needed to fully establish its impact on patient outcomes.
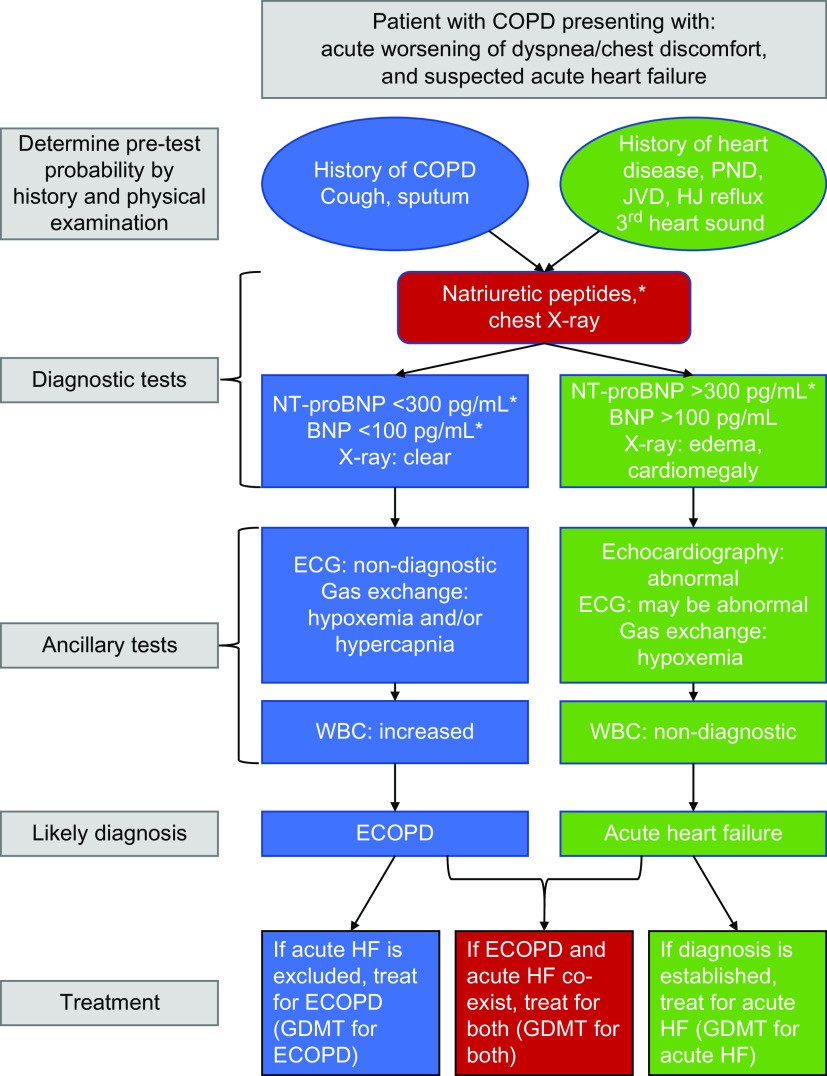
Figure 1. Algorithm for suspected acute heart failure in COPD patients with increased respiratory symptoms. This algorithm highlights the clinical features and diagnostic steps to differentiate acute heart failure from COPD exacerbation, emphasizing the use of natriuretic peptides and other diagnostic tools.
Ischemic Heart Disease
Ischemic Heart Disease (IHD) is another significant cardiovascular comorbidity that must be considered in the copd differential diagnosis. Underlying IHD can prolong ECOPDs and significantly increases the risk of myocardial infarction and stroke in COPD patients, both during and after an exacerbation. Myocardial injury is common during ECOPDs, especially in patients with pre-existing IHD.
When evaluating a COPD patient with suspected ECOPD, clinicians should consider IHD, particularly if the patient presents with chest pain or discomfort, palpitations, signs of systemic atherosclerosis, or symptoms suggestive of acute myocardial ischemia. An electrocardiogram (ECG) is crucial in these patients. While COPD can cause chronic elevations in troponin levels, which may further increase during an ECOPD, the diagnosis of myocardial injury or infarction should adhere to universal criteria, requiring elevated troponin levels along with at least one other ischemic indicator like symptoms or new ECG changes. Given the high co-occurrence of IHD and COPD, evaluation for atherosclerosis and associated cardiac conditions should always be a part of the assessment in patients presenting with symptoms suggestive of ECOPD.
Arrhythmias
Cardiac arrhythmias, particularly atrial fibrillation (AF), are more common in COPD patients and should be part of the copd differential diagnosis. The risk of arrhythmias, including AF, significantly increases during ECOPDs. AF during an ECOPD is associated with increased morbidity and mortality. Symptoms of AF can include chest discomfort, palpitations, lightheadedness, and dyspnea, making differentiation from ECOPD challenging based on symptoms alone. However, an irregular pulse on palpation is a key clinical sign. ECG and cardiac monitoring are essential for detecting arrhythmias in these patients. While the exact role of new-onset AF in causing acute dyspnea in COPD is still being investigated, it is crucial to determine whether AF is a pre-existing condition or a new event in the context of worsening respiratory symptoms.
Pulmonary Embolism in COPD Differential Diagnosis
Pulmonary Embolism (PE) is a critical and potentially life-threatening condition that must be promptly considered in the copd differential diagnosis of patients with suspected ECOPD. The prevalence of PE in patients presenting with ECOPD varies widely, but it is more common in those with atypical or unexplained exacerbations. PE requires specific and timely management to improve patient outcomes.
PE should be suspected in COPD patients presenting with worsening dyspnea, especially when accompanied by risk factors such as a history of venous thromboembolic disease, recent hospitalization for heart failure, or malignancy. While dyspnea is a common symptom in both PE and ECOPD, patients with PE are more likely to report pleuritic chest pain, hemoptysis, and signs of right heart failure, and less likely to have a productive cough with purulent sputum.
Clinical probability scores, such as the revised Geneva score, can help assess the pretest probability of PE. Patients with a high clinical probability should undergo Computed Tomography Pulmonary Angiography (CTPA). For patients with a low clinical probability, D-dimer testing can be used to further risk-stratify. A negative D-dimer result can help exclude PE without the need for imaging. Lower limb compression ultrasonography (CUS) can be used to detect deep vein thrombosis (DVT), especially when CTPA is contraindicated or negative in patients with persistent suspicion of thromboembolism.
Figure 2. Algorithm for suspected pulmonary embolism in COPD patients with increased respiratory symptoms. This algorithm details the risk stratification and diagnostic pathways for pulmonary embolism in COPD patients, incorporating clinical probability scores, D-dimer testing, and imaging modalities.
Infectious Diseases in COPD Differential Diagnosis
Infections, particularly pneumonia, are frequent triggers for respiratory symptoms in COPD patients and are crucial to consider in the copd differential diagnosis.
Pneumonia
Pneumonia and ECOPD share several overlapping symptoms, such as worsened cough, increased sputum production, dyspnea, and fever, making copd differential diagnosis challenging. COPD itself increases the risk and severity of pneumonia, so pneumonia must always be considered in patients presenting with ECOPD symptoms. Physical examination can provide clues, with signs of lung consolidation like localized crackles and dullness on percussion being more suggestive of pneumonia.
For mild to moderate suspected ECOPD without signs of consolidation, further diagnostic testing to differentiate pneumonia may not be immediately necessary. However, in severe or prolonged episodes, or when consolidation signs are present, a thorough evaluation for pneumonia is warranted. Chest X-rays are often the initial diagnostic step, but CT scans can detect opacities not visible on X-ray in some cases.
Serum biomarkers can aid in differentiating pneumonia from ECOPD in the copd differential diagnosis. Higher CRP levels are more indicative of pneumonia, particularly bacterial pneumonia. Procalcitonin can also be helpful, with low levels suggesting a non-bacterial etiology in patients with a low pretest probability of pneumonia. Additionally, viral infections like respiratory syncytial virus, SARS-CoV-2 (COVID-19), and influenza should be considered, especially during relevant seasons, as specific treatments are available. Sputum purulence suggests bacterial infection and may guide antibiotic use. In severe cases, sputum Gram stain, cultures, and molecular point-of-care tests can help guide antibiotic therapy, and urine antigen tests for pneumococcal and Legionella antigens should be considered.
Figure 3. Algorithm for suspected pneumonia in COPD patients with increased respiratory symptoms. This algorithm outlines the diagnostic approach for pneumonia in COPD patients, emphasizing clinical assessment, chest imaging, and biomarkers to differentiate pneumonia from COPD exacerbations.
Bronchiectasis
Bronchiectasis, characterized by abnormal widening of the bronchi, frequently coexists with COPD and should be considered in the copd differential diagnosis. Patients with COPD and bronchiectasis experience more exacerbations, increased pneumonia risk, and higher mortality compared to those with either condition alone. The overlapping symptoms and increased risk of bacterial infections complicate the clinical picture.
While COPD diagnosis is primarily based on physiology (spirometry), bronchiectasis is diagnosed radiologically (CT scan). However, severe bronchiectasis can also lead to airflow obstruction meeting COPD spirometric criteria. In patients with frequent suspected ECOPDs, particularly those with persistent sputum production despite COPD management, CT scans should be considered to rule out bronchiectasis.
Inflammatory Morbidities in COPD Differential Diagnosis
Inflammatory conditions, such as asthma and interstitial lung diseases, can mimic or exacerbate COPD symptoms and need to be included in the copd differential diagnosis.
Asthma Exacerbation
Comorbid bronchial asthma is common in COPD patients. Distinguishing between asthma exacerbations and ECOPDs can be challenging, as both conditions can present with similar symptoms and triggers (viral infections, pollutants). While sputum purulence is traditionally associated with ECOPD, it can also occur in asthma exacerbations. In patients with known COPD and asthma, an acute worsening of respiratory symptoms could be either an ECOPD or an asthma exacerbation, or both. The management approach for patients with coexisting COPD and asthma is often similar to that of asthma, emphasizing bronchodilators and anti-inflammatory medications.
Interstitial Lung Diseases
Interstitial Lung Diseases (ILDs) should be considered in the copd differential diagnosis, particularly in patients with dry cough and dyspnea. While COPD and ILDs have different underlying mechanisms and static respiratory mechanics, both can cause dyspnea and cough. Furthermore, ILDs, especially idiopathic pulmonary fibrosis (IPF), are also characterized by exacerbations that can mimic ECOPDs, although IPF exacerbations typically have a worse prognosis.
In patients with combined pulmonary fibrosis and emphysema, differentiating between an ECOPD and an IPF exacerbation can be particularly difficult. Imaging studies, such as chest CT, can help. The presence of new widespread alveolar abnormalities (ground-glass opacities) on imaging in a patient presenting with ECOPD-like symptoms may suggest an ILD exacerbation is contributing to the clinical picture.
Miscellaneous Morbidities in COPD Differential Diagnosis
Several other conditions can present with respiratory symptoms that may be confused with ECOPDs and should be included in a comprehensive copd differential diagnosis.
Anxiety and Depression
Anxiety and depression are highly prevalent comorbidities in COPD patients and can significantly impact their respiratory symptoms. These conditions can increase the risk of ECOPDs and hospitalizations. Panic attacks and anxiety can cause tachypnea, which in COPD patients may lead to hyperinflation and potentially acute hypercapnic respiratory failure. Conversely, hypercapnia itself can trigger panic attacks, creating a vicious cycle. In COPD patients experiencing a panic attack, the absence of increased cough and sputum, and the lack of inflammatory markers or other clear causes of dyspnea and tachypnea, may point towards anxiety as the primary driver of symptoms.
Pneumothorax
Pneumothorax, or collapsed lung, is a potentially life-threatening condition that can occur in COPD patients and mimic an ECOPD. Patients with emphysema, especially older males with bullae, are at increased risk. Pneumothorax typically presents with sudden onset dyspnea and chest pain, often accompanied by hypoxemia. Diagnosis is usually confirmed by chest X-ray, and lung ultrasound can also be a rapid diagnostic tool, particularly in emergency settings.
Pleural Effusion
Large pleural effusions, or fluid accumulation in the pleural space, can contribute to worsening dyspnea in COPD patients. Pleural effusions can alter lung mechanics and cause restrictive ventilatory defects. The nature of the pleural effusion can provide clues to its etiology. Effusions associated with elevated natriuretic peptides are more likely cardiac in origin (HF), while those with high CRP levels suggest parapneumonic effusion or empyema due to infection. Chest X-ray, ultrasound, and CT scans are useful for detecting and characterizing pleural effusions.
Anemia
Anemia, a common comorbidity in COPD, can contribute to breathlessness and should be considered in the copd differential diagnosis. While polycythemia can indicate chronic hypoxemia in untreated COPD, anemia is also prevalent, particularly in older COPD patients with more severe airflow limitation and cardiac comorbidities. Although anemia may not directly increase ECOPD incidence, it can worsen dyspnea during exacerbations and impact severity. Anemia in COPD patients is associated with longer hospital stays and increased mortality, possibly due to its association with other comorbidities.
Conclusion: The Importance of a Systematic COPD Differential Diagnosis
Accurately diagnosing the cause of worsening respiratory symptoms in COPD patients is paramount. While many cases presenting with classic symptoms can be confidently diagnosed as ECOPDs, clinicians must be vigilant in considering and investigating other potential conditions in a copd differential diagnosis. Decompensation of comorbidities like heart failure, or acute events such as pneumonia or pulmonary embolism, can mimic or contribute to what may initially appear to be an ECOPD. Therefore, a systematic approach, incorporating thorough clinical evaluation, appropriate investigations, and a high index of suspicion for mimicking conditions, is crucial for all COPD patients presenting with worsening respiratory symptoms, particularly dyspnea without clear signs of infection. Adopting a precise diagnostic approach will not only improve individual patient care but also enhance the accuracy of clinical trials and reduce the mislabeling of hospital admissions, ultimately leading to better outcomes and reduced healthcare costs associated with COPD and its exacerbations.
References