Introduction
Porokeratosis represents a diverse group of skin disorders characterized by abnormal keratinization. A defining microscopic feature across all variants of porokeratosis is the cornoid lamella. This unique histological structure, however, can sometimes be elusive or mimic other conditions, leading to diagnostic challenges, particularly with benign lichenoid keratosis. Lichenoid keratosis, often considered a regressing seborrheic keratosis or solar lentigo, presents with a lichenoid inflammatory pattern, which can overlap histologically with porokeratosis. The potential for misdiagnosis arises when the cornoid lamella in porokeratosis is not readily apparent or is missed during tissue sampling, leading to a mistaken diagnosis of lichenoid keratosis, or vice versa.
This article delves into the complexities of Cornoid Lamella Differential Diagnosis, specifically in the context of benign lichenoid keratosis and porokeratosis. We aim to provide a comprehensive guide for dermatopathologists and clinicians to enhance diagnostic accuracy. By understanding the subtle histological nuances and recognizing potential pitfalls, we can improve patient care, especially given the low but present risk of malignant transformation associated with porokeratosis. This discussion is based on a critical review of 104 cases initially diagnosed as benign lichenoid keratosis, where we re-evaluated for features suggestive of porokeratosis and identified key diagnostic clues to aid in distinguishing these entities.
Understanding Cornoid Lamella in Differential Diagnosis
Cornoid Lamella: The Histopathological Hallmark of Porokeratosis
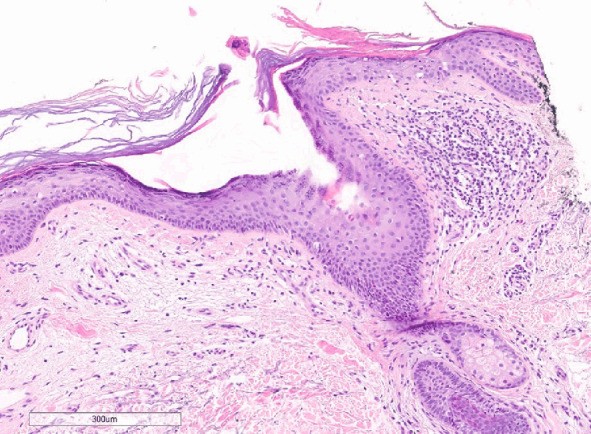
The cornoid lamella is the sine qua non for the diagnosis of porokeratosis. Histologically, it appears as a slender column of parakeratotic cells overlying an area of absent or diminished granular layer and dyskeratotic keratinocytes. Characteristically, the lamella is angled with its base pointing away from the lesion’s center and its apex directed inwards. In certain porokeratosis variants, such as porokeratosis of Mibelli, epidermal invagination may also be observed. While pathognomonic for porokeratosis in the appropriate context, it’s crucial to remember that the cornoid lamella is not exclusive to porokeratosis and can be seen in other conditions. Furthermore, sampling limitations, particularly if the biopsy does not include the peripheral raised border of a porokeratotic lesion where the cornoid lamella is most prominent, can lead to its absence in the histological sections and subsequent diagnostic errors.
Lichenoid Keratosis: A Diagnostic Mimic
Lichenoid keratosis, conversely, is a benign skin lesion typically presenting as a solitary, sometimes itchy, red or skin-colored papule or plaque. Histologically, it is defined by parakeratosis, epidermal thickening (acanthosis), and a dense band-like lymphocytic infiltrate in a lichenoid pattern, often with admixed plasma cells, eosinophils, and neutrophils. The lichenoid inflammatory reaction, a feature shared with porokeratosis, is a key factor contributing to potential diagnostic confusion.
The Challenge of Differential Diagnosis
The diagnostic dilemma arises because both porokeratosis and lichenoid keratosis can exhibit lichenoid inflammation. If the cornoid lamella in a case of porokeratosis is subtle, poorly formed, or missed due to sampling, the histological picture can easily be misinterpreted as lichenoid keratosis. This misdiagnosis can have clinical implications, as porokeratosis requires different management and follow-up strategies compared to lichenoid keratosis due to its potential for malignant transformation, albeit low. Accurate differentiation is therefore paramount for appropriate patient care.
Key Histological Clues for Differentiation
Based on our review and existing literature, we have identified several crucial histological clues that can aid in differentiating porokeratosis from lichenoid keratosis, particularly when the cornoid lamella is not immediately obvious.
Careful Examination of Serial Sections
One of the most effective strategies is to meticulously examine consecutive tissue sections. The cornoid lamella may be fragmented or only partially represented in a single section. As demonstrated in Figure 1, the lamella may appear at the edge of the specimen and become more apparent in deeper levels. Therefore, if there is any suspicion of porokeratosis, or if the initial sections are inconclusive, examining deeper serial sections is highly recommended to increase the chances of identifying a cornoid lamella.
Cornoid Lamella Morphology and Location
Even when present, the cornoid lamella can vary in its morphology and presentation. It may appear discontinuous across serial sections, exhibiting a “migratory” pattern as shown in Figure 2. In some sections, it might be subtle, while in deeper levels, it becomes more prominent and extends across the specimen. Recognizing this dynamic appearance is vital.
Adjacent Epidermal and Inflammatory Features
Features surrounding the suspected cornoid lamella can also provide important diagnostic hints. Areas of epidermal thinning with adjacent lichenoid inflammation near a parakeratotic column should raise suspicion for porokeratosis. This combination is less typical in lichenoid keratosis, where epidermal thinning is not a primary feature.
Flattening of the Cornoid Lamella
The cornoid lamella may not always exhibit its classical, prominent appearance. In some instances, it can be notably flattened and inconspicuous (Figure 3). In these cases, careful scrutiny is required to identify the subtle parakeratosis and the associated thinning of the adjacent epidermis, which are still indicative of a cornoid lamella, albeit a less pronounced one.
Dysplasia and Apoptotic Bodies
Careful assessment for dysplasia beneath a parakeratotic column can further strengthen the diagnosis of a cornoid lamella. Additionally, the presence of apoptotic bodies within the superficial dermis can be an accompanying feature supporting porokeratosis.
Follicular Involvement
In some challenging cases, the cornoid lamella may involve and appear to be concealed within a hair follicle (Figure 4). This follicular involvement can obscure the typical lamellar architecture and lead to diagnostic oversight. Being aware of this presentation, especially in biopsies where a clear cornoid lamella is not immediately evident on the surface epidermis, is crucial.
Stratum Corneum Alterations
The stratum corneum within the lesion or inside the cornoid lamella itself may exhibit alterations, such as compression (Figure 5). This altered stratum corneum, in conjunction with other features like thinned epidermis and lichenoid inflammation adjacent to a potential cornoid lamella, can be another helpful clue in distinguishing porokeratosis.
Study Findings: Reclassification of Lichenoid Keratosis Cases
Our critical re-evaluation of 104 cases initially diagnosed as benign lichenoid keratosis revealed that 9.6% of these cases displayed histological features more consistent with porokeratosis. This significant finding underscores the potential for misdiagnosis and highlights the importance of vigilance in identifying subtle cornoid lamellae. Only one of these reclassified cases had “porokeratosis” listed as a differential diagnosis on the clinical request form, further emphasizing the diagnostic challenge.
Clinical Significance and Diagnostic Recommendations
This study emphasizes that porokeratosis can be underdiagnosed and mistakenly categorized as benign lichenoid keratosis. The overlapping histological features and the potential for a subtle or missed cornoid lamella contribute to this diagnostic pitfall. To improve diagnostic accuracy in cornoid lamella differential diagnosis, we recommend the following:
- Maintain a High Index of Suspicion: When evaluating biopsies clinically suggestive of lichenoid keratosis, especially if there are atypical features or a lack of typical lichenoid keratosis characteristics, consider porokeratosis in the differential diagnosis.
- Thorough Histological Examination: Scrutinize all histological sections meticulously, paying close attention to parakeratotic columns, even subtle or flattened ones.
- Step Sections: If the initial sections are inconclusive but clinical suspicion for porokeratosis remains, obtain and examine deeper serial sections to maximize the chance of identifying a cornoid lamella.
- Evaluate Contextual Features: Assess for the presence of epidermal thinning, adjacent lichenoid inflammation, dyskeratosis, apoptotic bodies, follicular involvement, and stratum corneum alterations in conjunction with any parakeratotic columns.
- Clinicopathological Correlation: Integrate histological findings with clinical presentation. Clinical information, when available, can be invaluable in guiding the diagnostic process.
Conclusion
Distinguishing between porokeratosis and lichenoid keratosis can be challenging due to histological similarities, particularly the shared feature of lichenoid inflammation and the potential for a subtle or missed cornoid lamella in porokeratosis. A heightened awareness of the variations in cornoid lamella morphology, meticulous histological examination, and the consideration of ancillary histological features are crucial for accurate cornoid lamella differential diagnosis. By incorporating these strategies into routine dermatopathology practice, we can enhance diagnostic precision, ensuring appropriate management and follow-up for patients with these conditions.