Introduction
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, has had a devastating global impact, primarily affecting the respiratory system. However, it’s become increasingly clear that COVID-19 can also lead to a range of neurological complications. Among these, encephalitis, an inflammation of the brain, has emerged as a serious concern. While neurological issues like stroke and anosmia (loss of smell) have been more widely discussed, Covid Encephalitis Diagnosis and the broader characteristics of this condition remain less understood. This is despite growing reports highlighting the severe morbidity and mortality associated with encephalitis in COVID-19 patients.
Early research began to characterize some neurological impacts of COVID-19, but less common yet significant complications such as encephalitis, Guillain-Barré syndrome, and myelitis needed further investigation. The severe outcomes linked to COVID-19 encephalitis underscore the urgent need for systematic research. Understanding the risk factors, clinical presentation, and diagnostic pathways for COVID encephalitis is crucial for effective patient management and improved outcomes. Currently, comprehensive information on COVID encephalitis diagnosis is limited, creating a significant gap in our knowledge. This article aims to address this gap by providing a detailed overview of COVID-19 related encephalitis, focusing on incidence, diagnosis, clinical progression, and patient outcomes, synthesized from available research.
Diagnostic Methods: Study Selection and Criteria
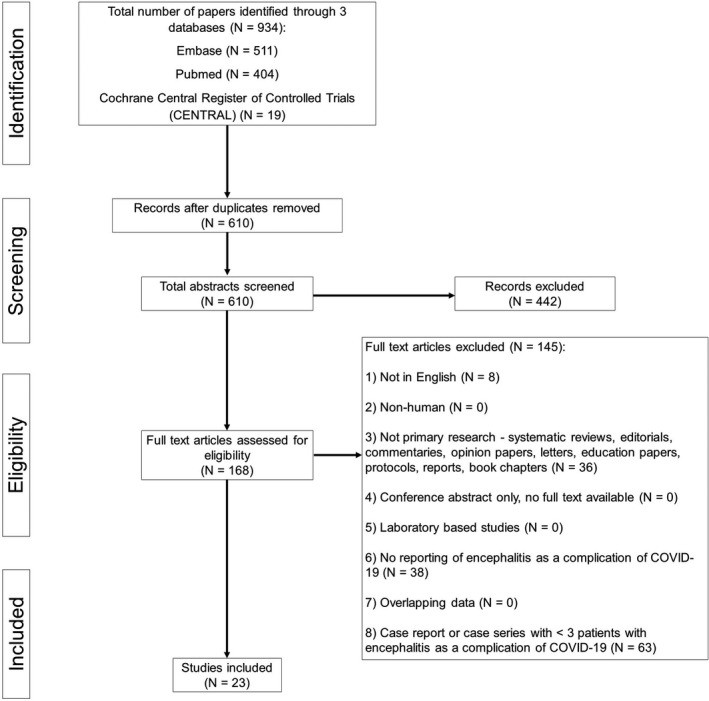
To comprehensively understand COVID encephalitis diagnosis, a systematic review and meta-analysis was conducted, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. This rigorous approach ensured a transparent and reliable synthesis of existing research. The core objective was to analyze studies that reported on encephalitis as a complication of COVID-19, specifically focusing on how these cases were diagnosed and characterized.
A detailed search strategy was developed to identify relevant original research studies. The search targeted major electronic databases, including PubMed, Embase, and CENTRAL, covering publications from November 1, 2019, to October 24, 2020. This timeframe was chosen to capture studies published after the emergence of the novel coronavirus in late 2019. The search strategy employed specific keywords related to COVID-19 and encephalitis to ensure comprehensive identification of relevant literature.
The key diagnostic criterion for inclusion in this analysis was evidence of encephalitis based on radiological and/or biochemical findings. Encephalitis was defined as inflammation of the brain, and studies were included if they reported cases diagnosed through brain imaging, such as computed tomography (CT) or magnetic resonance imaging (MRI) scans, or through cerebrospinal fluid (CSF) analysis. This strict inclusion criterion ensured that only confirmed cases of encephalitis were analyzed, strengthening the reliability of the findings related to COVID encephalitis diagnosis.
Studies were screened independently by two reviewers, and any disagreements were resolved through consensus or a third senior reviewer, ensuring objectivity in study selection. The quality of the included studies was rigorously assessed using established checklists from the Joanna Briggs Institute (JBI), evaluating the methodology and reporting quality of both prevalence studies and case series. Data extraction focused on key variables relevant to COVID encephalitis diagnosis, including study details, patient demographics, clinical symptoms, laboratory and radiological findings, time from COVID-19 diagnosis to encephalitis onset, treatment approaches, and patient outcomes, particularly mortality.
Incidence of COVID Encephalitis: A Meta-Analysis of Available Data
Analyzing data from 23 studies encompassing 129,008 patients, including 138 diagnosed with encephalitis, this meta-analysis sheds light on the incidence of encephalitis as a complication of COVID-19. The pooled incidence rate was found to be 0.215% (95% CI = 0.056%–0.441%). This relatively low overall incidence suggests that while COVID encephalitis diagnosis is not a common outcome for all COVID-19 patients, it remains a clinically significant complication due to its severity.
Interestingly, when considering only severely ill COVID-19 patients, the incidence of encephalitis was substantially higher, reaching 6.7% (95% CI = 4.3%–9.4%). This significant increase highlights that severe COVID-19 illness is a major risk factor for developing encephalitis. The data indicates that while COVID encephalitis diagnosis might be infrequent in the general COVID-19 population, it is a more pertinent concern in patients experiencing severe COVID-19 symptoms requiring intensive care.
The average time from COVID-19 diagnosis to the onset of encephalitis symptoms was 14.5 days (range = 10.8–18.2 days). This timeframe is crucial for clinicians to consider when monitoring COVID-19 patients, particularly those with severe illness, for potential neurological complications. The delayed onset of encephalitis post-COVID-19 diagnosis suggests a potential window for heightened vigilance and early diagnostic evaluation if neurological symptoms arise.
Clinical Presentation for COVID Encephalitis Diagnosis: Symptoms and Severity
Understanding the clinical presentation is vital for accurate and timely COVID encephalitis diagnosis. The analysis revealed that the majority of patients who developed encephalitis had severe COVID-19 illness (83.8%, 95% CI = 62.0%–98.6%). Severe illness was defined as requiring intensive care unit (ICU) or high-dependency unit (HDU) admission, indicating a strong correlation between COVID-19 severity and the risk of encephalitis.
Common COVID-19 symptoms reported prior to encephalitis diagnosis included shortness of breath (84.6%) and fever (63.6%). Cough (60.0%) and fatigue (50.0%) were also prevalent, but to a lesser extent. Notably, a significant proportion of patients (23.8%) were asymptomatic for typical COVID-19 symptoms, suggesting that encephalitis can occur even in the absence of prominent respiratory signs.
The hallmark symptoms of encephalitis, crucial for COVID encephalitis diagnosis, included loss or decreased level of consciousness (77.1%) and altered mental state (72.3%). Seizures (38.2%) and headaches (27.3%) were also common neurological manifestations. Weakness (15.4%) and less frequent symptoms like aphasia, ataxia, and myoclonus were also reported. This diverse range of neurological symptoms emphasizes the complexity of COVID encephalitis diagnosis and the need for a comprehensive clinical assessment.
Laboratory and Radiological Findings: Aids in COVID Encephalitis Diagnosis
Laboratory and radiological investigations play a crucial role in confirming COVID encephalitis diagnosis and differentiating it from other neurological conditions. Serum analysis of patients with COVID encephalitis revealed several key derangements. D-dimer levels, a marker of coagulation activation, were significantly elevated, averaging 13.4 mg/L. Lactate dehydrogenase (LDH) levels, indicative of tissue damage, were also raised, averaging 358.7 U/L. Inflammatory markers such as C-reactive protein (CRP), averaging 58.8 mg/L, and Interleukin-6 (IL-6), averaging a markedly elevated 1327.9 pg/ml, were also significantly increased, reflecting a systemic inflammatory response.
Cerebrospinal fluid (CSF) analysis, when performed, showed elevated protein levels, averaging 64.8 mg/dl, and mild pleocytosis (increased white blood cell count), averaging 14.8 cells/µl. These CSF findings, while not always present or dramatic, support the inflammatory nature of COVID encephalitis.
Brain imaging, particularly MRI, is essential for COVID encephalitis diagnosis. Common MRI findings included diffuse white matter hyperintensities and hemorrhagic lesions, particularly on fluid-attenuated inversion recovery (FLAIR) and T2-weighted sequences. These findings are consistent with inflammatory and demyelinating processes in the brain. While CT scans of the head were generally less informative, MRI proved to be a more sensitive modality for detecting brain abnormalities in COVID encephalitis. However, it is important to note that some cases of COVID encephalitis may present with normal brain imaging, potentially due to milder disease or imaging performed too early in the disease course.
Patient Demographics and Risk Factors in COVID Encephalitis Diagnosis
Demographic factors and pre-existing comorbidities appear to influence the risk of COVID encephalitis diagnosis. The mean age of patients diagnosed with COVID encephalitis was 59.4 years, with a range from 43.0 to 80.0 years, indicating older age as a potential risk factor. There was no significant gender predilection, with approximately equal proportions of males and females affected (49.3% male).
A significant majority of patients (71.7%) had at least one comorbidity. Hypertension (45.5%), hyperlipidemia (24.0%), and diabetes mellitus (16.0%) were the most common pre-existing conditions. Less frequent comorbidities included chronic kidney disease, chronic liver disease, and congestive cardiac failure. These findings suggest that older individuals with pre-existing conditions are at higher risk of developing encephalitis as a complication of COVID-19, likely due to reduced physiological reserves and increased vulnerability to severe complications.
Outcomes and Mortality Associated with COVID Encephalitis Diagnosis
Despite its relatively low overall incidence, COVID encephalitis carries a significant risk of adverse outcomes. The pooled mortality rate among patients diagnosed with COVID encephalitis was 13.4% (95% CI = 3.8%–25.9%). This substantial mortality rate underscores the severity of this neurological complication and the importance of early COVID encephalitis diagnosis and appropriate management.
The high mortality rate, coupled with the potential for significant morbidity among survivors, highlights the clinical importance of recognizing and effectively managing COVID encephalitis. While the incidence might be uncommon, the severe consequences for affected individuals necessitate vigilance, particularly in high-risk populations such as severely ill and older COVID-19 patients.
Discussion: Implications for COVID Encephalitis Diagnosis and Management
This systematic review and meta-analysis provides a comprehensive overview of COVID encephalitis diagnosis, incidence, clinical features, and outcomes. The findings emphasize that while encephalitis is an uncommon complication of COVID-19, it is a serious condition associated with significant morbidity and mortality, especially in severely ill patients.
The diagnosis of COVID encephalitis relies on a combination of clinical presentation, laboratory investigations, and neuroimaging. Clinicians should be vigilant for neurological symptoms, particularly altered mental status, decreased consciousness, and seizures, in COVID-19 patients, especially those with severe illness. Elevated inflammatory markers in serum and suggestive findings on brain MRI, particularly white matter hyperintensities and hemorrhagic lesions, can further support the diagnosis. CSF analysis may provide additional evidence of inflammation, although it is not always diagnostic.
The pathophysiology of COVID encephalitis is likely multifactorial, involving direct viral invasion of the nervous system, systemic inflammation, and autoimmune mechanisms. While direct viral invasion is debated, systemic inflammation and molecular mimicry are considered important contributors to the development of encephalitis in the context of COVID-19.
Treatment strategies for COVID encephalitis are still evolving. Current approaches include corticosteroids, intravenous immunoglobulin, plasmapheresis, and monoclonal antibodies like rituximab. While case series suggest potential benefits of these treatments, large-scale randomized controlled trials are needed to establish definitive treatment protocols for COVID encephalitis.
Further research is crucial to improve our understanding of COVID encephalitis diagnosis, pathophysiology, and optimal management. Collaborative international registries and ongoing studies are needed to collect more comprehensive data, refine diagnostic criteria, and evaluate the effectiveness of different treatment strategies. Enhanced vigilance and research efforts are essential to mitigate the impact of this serious neurological complication of COVID-19.
Conclusion
COVID encephalitis, although an uncommon complication of COVID-19, presents a significant clinical challenge due to its severity and associated mortality. Severely ill COVID-19 patients are at a higher risk of developing encephalitis. Early COVID encephalitis diagnosis, based on clinical suspicion, neuroimaging, and laboratory findings, is crucial for timely intervention and potentially improved outcomes. Continued research and international collaboration are vital to further elucidate the complexities of COVID encephalitis and enhance patient care.
Conflict of Interest
The authors declare no financial or other conflicts of interest.
Author Contributions
Isabel Siow: Conceptualization (lead), methodology (lead), visualization (lead), writing–original draft (lead), writing–review & editing (lead). Keng Siang Lee: Writing–original draft (supporting), writing–review & editing (supporting). John J. Y. Zhang: Writing–original draft (supporting), writing–review & editing (supporting). Seyed Ehsan Saffari: Data curation (lead), formal analysis (lead), software (lead). Adeline Ng: Supervision (lead).
Ethical Approval
Research ethics approval was not applicable, as this submission did not involve human participants. All information was obtained from publicly available, published articles.
Disclaimers
The views expressed in this article are entirely our own and not an official position of our institutions.
Supporting information
Fig S1
Click here for additional data file. (385.8KB, jpg)
Fig S2
Click here for additional data file. (691.4KB, jpg)
Supplementary Material
Click here for additional data file. (28.9KB, docx)
Acknowledgements
We thank Toh Kim Kee for her assistance in designing the initial search strategy.
Siow I, Lee KS, Zhang JJY, Saffari SE, Ng A. Encephalitis as a neurological complication of COVID‐19: A systematic review and meta‐analysis of incidence, outcomes, and predictors. Eur J Neurol. 2021;28:3491–3502. 10.1111/ene.14913
Contributor Information
Isabel Siow, Email: [email protected].
Adeline Ng, Email: [email protected].
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in PubMed. Additionally, the data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Click here for additional data file. (385.8KB, jpg)
Fig S2
Click here for additional data file. (691.4KB, jpg)
Supplementary Material
Click here for additional data file. (28.9KB, docx)
Data Availability Statement
The data that support the findings of this study are openly available in PubMed. Additionally, the data that support the findings of this study are available from the corresponding author upon reasonable request.