Introduction
The “crazy paving pattern,” a descriptive term in medical imaging, particularly in high-resolution computed tomography (HRCT) of the lungs, refers to a specific radiological finding. This pattern, characterized by ground-glass opacities superimposed with a linear pattern, resembles irregularly shaped paving stones, hence the name. Initially considered pathognomonic for pulmonary alveolar proteinosis, it is now recognized as a non-specific sign present in a wide array of both acute and chronic lung diseases. For auto repair experts who are expanding their knowledge base into medical diagnostics or simply interested in understanding complex patterns, grasping the differential diagnosis of the crazy paving pattern can be intellectually stimulating and broaden perspectives on pattern recognition in different fields. This article aims to provide a detailed exploration of the crazy paving pattern, its underlying causes, and the range of diseases it can indicate, enhancing your diagnostic acumen. We will correlate computed tomography (CT) findings with histopathological evidence to provide a comprehensive understanding.
What is the Crazy-Paving Pattern?
The crazy-paving pattern is visually defined on CT scans as the combination of two primary features: ground-glass opacity (GGO) and a superimposed linear pattern. Understanding each component is crucial to appreciating the significance of the overall pattern.
Ground-Glass Opacity (GGO): GGO is described as a hazy increase in lung density on CT images. Importantly, it occurs without obscuring the underlying bronchial and vascular structures. This means that while the lung appears denser than normal, the outlines of airways and blood vessels within the affected area are still visible. GGO indicates partial filling of airspaces, thickening of alveolar walls, or interstitial thickening – all of which reduce the air content in the lung tissue, leading to increased X-ray attenuation.
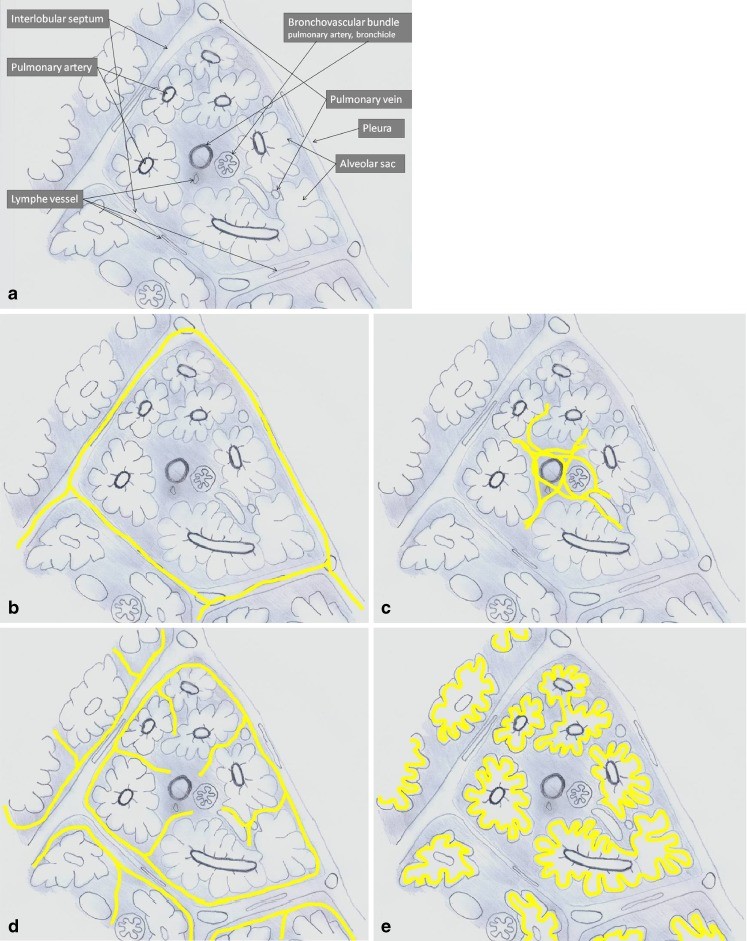
Linear Pattern: Superimposed on the GGO is a network of lines, creating the “crazy paving” appearance. This linear component can arise from several sources within the lung’s structural units, the secondary pulmonary lobules. These include:
- Thickening of interlobular septa: These are the walls between the secondary pulmonary lobules. When they thicken, they appear as lines on CT.
- Thickening of intralobular septa and interstitium: Within the lobules, the interstitium and septa can also thicken, creating a finer, reticular pattern.
- Periacinar pattern: This involves the linear deposition of material within the airspaces, specifically at the borders of the acini (small air sacs) and secondary pulmonary lobules.
Fig. 1. Illustrating the anatomy of the secondary pulmonary lobule (a) and various reticular patterns (b-e) including thickening of interlobular septa (b), intralobular interstitium (c), irregular fibrosis (d), and periacinar pattern (e), which contribute to the crazy-paving appearance on CT scans.
Differential Diagnosis of the Crazy-Paving Pattern
The crazy-paving pattern, while striking, is not specific to a single disease. Its presence necessitates a differential diagnosis, considering a range of acute and chronic conditions. These conditions can be broadly categorized to aid in systematic evaluation.
Acute Diseases Presenting with Crazy-Paving Pattern
Several acute conditions can manifest with a crazy-paving pattern. These often involve rapid onset and significant respiratory symptoms.
1. Pulmonary Edema:
Pulmonary edema, or fluid accumulation in the lungs, can result from various causes, most commonly heart failure. In cardiogenic pulmonary edema, increased hydrostatic pressure in the pulmonary capillaries leads to fluid transudation into the interstitium and alveoli.
- CT Findings: Patchy or diffuse ground-glass opacities, often with a perihilar and basilar distribution. Superimposed interlobular septal thickening is common, contributing to the linear component of the crazy-paving pattern. Vascular engorgement and pleural effusions may also be present.
2. Pulmonary Infections:
A variety of infections, both typical and atypical, can cause a crazy-paving pattern.
- Bacterial Pneumonia: Certain bacterial pneumonias, especially those causing diffuse alveolar damage, can present with GGO and interlobular septal thickening.
- Viral Pneumonia: Viral infections like influenza, adenovirus, and particularly COVID-19, are well-known to cause GGO and crazy-paving patterns. The linear component in viral pneumonia often reflects interstitial inflammation and edema.
- Pneumocystis jirovecii Pneumonia (PCP): Common in immunocompromised individuals, PCP typically shows bilateral GGO and superimposed reticular or linear patterns, including interlobular septal thickening. Histologically, the alveolar exudate and interstitial thickening contribute to these findings.
Fig. 9. CT scan demonstrating a patchy crazy-paving pattern in a patient with Pneumocystis jirovecii infection, characterized by ground-glass opacities and a superimposed linear pattern, predominantly in the central lung regions.
- Mycoplasma Pneumonia: This atypical bacterial infection can also present with GGO and a reticular pattern, sometimes mimicking crazy paving.
3. Pulmonary Hemorrhage:
Pulmonary hemorrhage, or bleeding into the lung tissue, can be caused by various conditions such as vasculitis, coagulopathies, and trauma.
- CT Findings: Ground-glass opacities are the predominant finding, reflecting blood in the alveoli. Superimposed linear opacities can occur, especially in cases of alveolar hemorrhage associated with capillaritis or interstitial involvement.
4. Acute Interstitial Pneumonia (AIP) / Acute Respiratory Distress Syndrome (ARDS):
AIP and ARDS represent severe forms of acute lung injury. ARDS can arise from sepsis, trauma, or pneumonia, while AIP is often idiopathic.
- CT Findings: Diffuse and bilateral ground-glass opacities progressing to consolidation are typical. Crazy-paving pattern can be seen in the early to intermediate phases due to a combination of alveolar edema, hemorrhage, and hyaline membrane formation, along with interstitial thickening.
Fig. 10. CT image showing bilateral crazy-paving pattern in a patient with Acute Respiratory Distress Syndrome, with extensive ground-glass attenuation and superimposed reticular lines indicative of interlobular and intralobular septal thickening.
5. Eosinophilic Pneumonia (Acute):
Acute eosinophilic pneumonia is characterized by rapid onset of respiratory symptoms and eosinophilic infiltration of the lungs.
- CT Findings: Peripheral ground-glass opacities and consolidation are common. Crazy-paving pattern can occur, especially in the GGO areas, due to interstitial and alveolar eosinophilic inflammation.
6. Radiation Pneumonitis (Acute Phase):
Following radiation therapy to the chest, radiation pneumonitis can develop in the treated field.
- CT Findings: Ground-glass opacities and consolidation within the radiation field are typical. Crazy-paving pattern may be seen in the acute phase (4-12 weeks post-radiation) due to alveolar damage, edema, and capillary congestion, resulting in both GGO and linear patterns.
Fig. 6. CT scan showing a patchy crazy-paving pattern in a patient with radiation pneumonitis, demonstrating ground-glass opacities and thickening of interlobular septa in the radiation field.
Subacute/Chronic Diseases Presenting with Crazy-Paving Pattern
Chronic conditions evolving over a longer period can also manifest with a crazy-paving pattern.
1. Alveolar Proteinosis (Pulmonary Alveolar Proteinosis – PAP):
PAP is a rare disorder characterized by the accumulation of surfactant in the alveoli.
- CT Findings: Crazy-paving pattern was initially described as pathognomonic for PAP. It typically shows diffuse ground-glass opacities with superimposed interlobular and intralobular septal thickening. The linear pattern in PAP is partly due to material deposition along the interlobular septa and within the acini (periacinar pattern). Histopathology confirms alveoli filled with proteinaceous material.
Fig. 2. CT image illustrating a patchy crazy-paving pattern in alveolar proteinosis, with ground-glass opacities and superimposed lines corresponding to material deposition along interlobular and intralobular septa.
2. Interstitial Lung Diseases (ILDs):
Various chronic ILDs can present with a crazy-paving pattern, although it is not always the dominant feature.
- Non-Specific Interstitial Pneumonia (NSIP): NSIP often shows subpleural and patchy ground-glass opacities. Crazy-paving can be present due to the combination of GGO and superimposed reticular opacities from interstitial thickening and fibrosis.
- Usual Interstitial Pneumonia (UIP): While UIP is more typically characterized by honeycombing and traction bronchiectasis, focal areas of GGO and crazy paving can be seen, especially in early stages or areas of active inflammation superimposed on fibrosis.
- Organizing Pneumonia (OP): OP, also known as cryptogenic organizing pneumonia (COP) when idiopathic, can present with patchy consolidation and GGO. Crazy-paving pattern can be seen, though less commonly than consolidation.
Fig. 5. CT scan demonstrating a crazy-paving pattern in non-specific interstitial pneumonia, particularly in the peripheral lung regions, with ground-glass opacification and superimposed reticular pattern due to interlobular and intralobular septal thickening.
- Hypersensitivity Pneumonitis (HP): In subacute HP, GGO and crazy-paving pattern can be prominent, along with air trapping and centrilobular nodules. Chronic HP may show fibrosis and honeycombing, but crazy-paving can still be present in areas of active inflammation.
Fig. 3. CT image showing a crazy-paving pattern in hypersensitivity pneumonitis, with geographic distribution of ground-glass opacities and superimposed thickened interlobular and intralobular septa, predominantly in the upper lung fields.
3. Vasculitis (e.g., Churg-Strauss Syndrome):
Pulmonary involvement in vasculitis, such as Churg-Strauss syndrome (eosinophilic granulomatosis with polyangiitis), can manifest with various patterns, including crazy paving.
- CT Findings: Ground-glass opacities, consolidation, and interlobular septal thickening can be seen. The crazy-paving pattern reflects alveolar hemorrhage, inflammation, and interstitial involvement associated with vasculitis.
4. Eosinophilic Pneumonia (Chronic):
Chronic eosinophilic pneumonia tends to have more persistent and migratory infiltrates compared to the acute form.
- CT Findings: Similar to acute eosinophilic pneumonia, but findings are more chronic and may show migratory patterns. Crazy-paving can be seen in areas of GGO.
5. Sarcoidosis:
Pulmonary sarcoidosis typically presents with perilymphatic nodules and bronchovascular bundle thickening. However, ground-glass opacities and crazy-paving patterns can also occur.
- CT Findings: Crazy-paving in sarcoidosis is often associated with granulomatous inflammation and interstitial fibrosis. It is less common than other typical sarcoidosis findings like nodules and lymphadenopathy.
Fig. 12. CT scan demonstrating a diffuse crazy-paving pattern in sarcoidosis, showing a widespread increase in lung attenuation with superimposed irregular reticular pattern due to interstitial and peribronchovascular thickening.
6. Lymphangitic Spread of Tumor (Lymphangitis Carcinomatosa):
Malignancy spreading through the lymphatic vessels of the lung can cause interlobular septal thickening and GGO.
- CT Findings: Crazy-paving pattern in lymphangitic carcinomatosa is due to a combination of tumoral infiltration of the lymphatics, interstitial edema, and fibrosis. Nodular or irregular septal thickening is characteristic, along with GGO.
Fig. 8. CT image showing a diffuse crazy-paving pattern in lymphangitic carcinomatosis, with ground-glass attenuation and thickened interlobular septa, along with nodular lesions suggesting pulmonary metastases.
7. Lipid Pneumonia (Exogenous Lipid Pneumonia):
Chronic inhalation of oils or lipids can lead to lipid pneumonia, primarily affecting the alveolar spaces.
- CT Findings: Ground-glass opacities and consolidations, often in the lower lobes, are typical. Crazy-paving pattern can be present. Fat attenuation within the lesions can be a clue.
Fig. 7. CT image showing a crazy-paving pattern in exogenous lipid pneumonia, with areas of ground-glass attenuation and thickening of interlobular and intralobular interstitium, predominantly in the right middle and lower lobes.
8. Alveolar Microlithiasis:
A rare disease characterized by the intra-alveolar accumulation of calcium-phosphate microliths.
- CT Findings: Diffuse, bilateral, and symmetrical sand-like micronodules are the hallmark. Crazy-paving pattern can be a less common associated finding.
9. Barium Aspiration:
Aspiration of barium contrast, though rare, can cause a crazy-paving pattern in acute or chronic phases.
- CT Findings: Dense consolidation or GGO, often with a crazy-paving appearance, depending on the timing and severity of aspiration.
10. Graft-versus-Host Disease (GVHD):
Pulmonary GVHD in hematopoietic stem cell transplant recipients can manifest with various CT patterns, including crazy paving.
- CT Findings: Diffuse interstitial and alveolar infiltrates, including ground-glass opacities and linear patterns, can result in a crazy-paving appearance.
Fig. 13. CT image showing a crazy-paving pattern in graft-versus-host disease, with multiple areas of ground-glass attenuation and consolidations, and superimposed thickened interlobular and intralobular septa.
11. Tumor (Bronchioloalveolar Carcinoma/Adenocarcinoma in situ):
Bronchioloalveolar carcinoma (BAC), now classified as adenocarcinoma in situ and minimally invasive adenocarcinoma, can present with a range of CT appearances, including crazy paving.
- CT Findings: Crazy-paving pattern in BAC reflects lepidic growth along alveolar walls and infiltration of the interstitium by tumor or inflammatory cells.
Fig. 15. CT scan showing a patchy crazy-paving pattern in bronchioloalveolar carcinoma, with areas of ground-glass opacification and consolidation, and a superimposed reticular pattern due to interstitial thickening.
Diagnostic Approach and Conclusion
When encountering a crazy-paving pattern on CT, a systematic diagnostic approach is crucial. This involves:
- Clinical Correlation: Detailed clinical history, symptoms, and risk factors are paramount. Acute vs. chronic presentation, immunocompromised status, occupational exposures, and medication history are critical.
- Radiological Assessment: Careful evaluation of the CT pattern, distribution (diffuse, patchy, peripheral, central), associated findings (consolidation, nodules, pleural effusion, lymphadenopathy, honeycombing), and temporal changes are essential.
- Laboratory and Bronchoscopic Investigations: Depending on the clinical context, investigations may include blood tests, bronchoalveolar lavage (BAL), and lung biopsy for histopathological confirmation.
The crazy-paving pattern, while not pathognomonic, is a significant radiological finding that narrows the differential diagnosis to a specific set of lung conditions. By integrating radiological findings with clinical and pathological data, accurate diagnoses can be achieved. For auto repair experts, understanding this pattern in medical imaging highlights the broader concept of pattern recognition and differential diagnosis, skills valuable across diverse fields.
References
The references from the original article should be included here to maintain academic integrity and allow readers to delve deeper into the primary literature. (Please include the original references as provided in the source document)