Nursing diagnosis is a cornerstone of effective patient care. It’s more than just identifying a health problem; it’s a clinical judgment about a patient’s response to health conditions and life processes. This guide will walk you through the essential concepts of nursing diagnosis, its purpose, types, and most importantly, how to create accurate and effective nursing diagnoses to enhance patient outcomes.
What is a Nursing Diagnosis?
A nursing diagnosis is defined as a clinical judgment concerning a human response to health conditions, life processes, or vulnerability to that response, from an individual, family, group, or community. It’s a statement that provides the foundation for nurses to select interventions and achieve patient-centered outcomes for which they are accountable. Nursing diagnoses are derived from the data gathered during a comprehensive nursing assessment and serve as the crucial link to developing individualized care plans.
The primary purposes of formulating a nursing diagnosis are multifaceted:
- Enhancing Critical Thinking: For nursing students, the process of creating nursing diagnoses is an invaluable tool for developing problem-solving and critical thinking skills. It challenges them to analyze patient data and make informed clinical judgments.
- Prioritizing Care: Nursing diagnoses help in identifying and prioritizing patient needs. By clearly defining the patient’s problems, nurses can effectively direct interventions based on the urgency and importance of each diagnosis.
- Guiding Interventions: A well-formulated nursing diagnosis directly guides the selection of appropriate nursing interventions. It ensures that care is targeted and addresses the specific needs identified in the diagnosis.
- Establishing Measurable Outcomes: Nursing diagnoses are essential for setting expected outcomes, which are crucial for quality assurance and meeting the requirements of healthcare payers. They provide a benchmark against which the effectiveness of nursing care can be measured.
- Understanding Patient Responses: They help nurses understand how patients respond to actual or potential health issues and life events. This understanding includes recognizing patient strengths and available resources that can be utilized to resolve or prevent problems.
- Facilitating Communication: Nursing diagnoses provide a common language for nurses and the healthcare team, fostering clear and effective communication. This shared understanding is vital for collaborative patient care.
- Evaluating Care Effectiveness: By establishing a clear diagnosis and expected outcomes, nurses can evaluate the effectiveness and cost-efficiency of the nursing care provided. This evaluation is crucial for continuous improvement in patient care delivery.
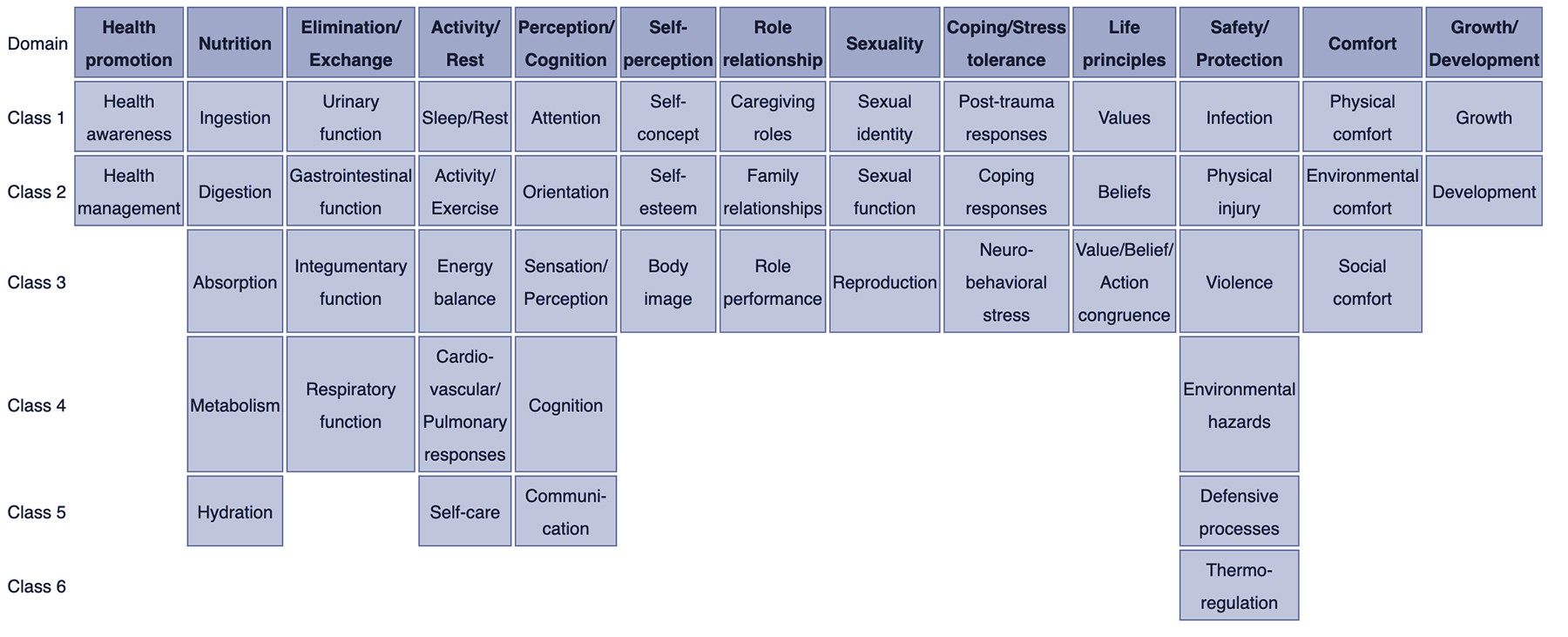
NURSING DIAGNOSIS TAXONOMY II. Taxonomy II for nursing diagnosis contains 13 domains and 47 classes. Image via: Wikipedia.com
Understanding the Nursing Process: The Foundation for Diagnosis
Creating A Nursing Diagnosis is the second step in the nursing process, following assessment. The nursing process is a systematic, five-step approach to patient care: Assessment, Diagnosis, Planning, Implementation, and Evaluation (ADPIE). Each step is interdependent and relies on critical thinking to ensure patient-centered care.
Assessment is the initial phase where nurses collect comprehensive patient data, including physical, psychological, social, and spiritual aspects. This data collection involves various methods such as patient interviews, physical examinations, and reviewing medical records.
Diagnosis is the analytical phase where nurses analyze the assessment data to identify patterns and formulate nursing diagnoses. This step requires clinical judgment to interpret the data and select the appropriate diagnostic labels.
Planning involves setting patient-centered goals and outcomes based on the nursing diagnoses. Nurses develop a care plan that outlines specific interventions to achieve these goals.
Implementation is the action phase where nurses carry out the planned interventions. This may include direct patient care, education, and coordination with other healthcare professionals.
Evaluation is the final step where nurses assess the patient’s response to the interventions and determine if the goals and outcomes have been achieved. This step is crucial for modifying the care plan as needed and ensuring effective patient care.
The nursing diagnosis step is pivotal as it bridges the gap between assessment and planning. Accurate nursing diagnoses are essential for developing effective care plans and ensuring positive patient outcomes. Without a clear and precise nursing diagnosis, interventions may be misdirected, and patient needs may not be adequately addressed.
Differentiating Nursing, Medical, and Collaborative Problems
It’s crucial to differentiate nursing diagnoses from medical diagnoses and collaborative problems to ensure appropriate and effective care planning.
Nursing Diagnoses focus on the patient’s response to health conditions or life processes. They describe problems that nurses, by virtue of their education, experience, and expertise, are licensed and competent to treat. Nursing interventions are primarily independent and aim to address the patient’s physical, psychological, and spiritual responses. For instance, a patient with pneumonia may have a nursing diagnosis of “Ineffective Airway Clearance related to increased mucus production as evidenced by adventitious breath sounds and cough.” The nursing interventions would focus on helping the patient clear their airway through techniques like coughing and deep breathing exercises.
Medical Diagnoses, on the other hand, are made by physicians or advanced practitioners and identify diseases or pathological conditions. Medical diagnoses deal with the disease process itself and are treated with medical interventions such as medications, surgery, and other medical treatments. Using the same example of pneumonia, the medical diagnosis is pneumonia itself. Medical treatment would involve antibiotics and potentially other medications prescribed by a physician.
Collaborative Problems are physiological complications that require both medical and nursing interventions to monitor and prevent. These are potential problems that nurses monitor to detect onset or changes in status. When collaborative problems occur, nurses work in collaboration with physicians and other healthcare providers to manage them. For example, a patient with pneumonia is at risk for a collaborative problem of “Potential Complication: Respiratory Failure.” Nursing responsibilities include monitoring respiratory status closely and implementing physician-prescribed treatments to prevent or manage respiratory failure.
Understanding these distinctions is vital for creating appropriate care plans. Nursing diagnoses guide independent nursing actions, medical diagnoses guide medical treatments, and collaborative problems require interdependent actions. Nurses must clearly identify and differentiate these to provide holistic and effective patient care.
Types of Nursing Diagnoses: Choosing the Right Category
There are four main types of nursing diagnoses, each serving a distinct purpose in patient care: Problem-Focused (Actual), Risk, Health Promotion, and Syndrome. Understanding these types is crucial for creating accurate diagnoses.
TYPES OF NURSING DIAGNOSES. The four types of nursing diagnosis are Actual (Problem-Focused), Risk, Health Promotion, and Syndrome.
1. Problem-Focused Nursing Diagnosis (Actual Diagnosis): This type identifies a problem that is present at the time of the nursing assessment. It’s based on observable signs and symptoms. A problem-focused diagnosis has three components: the diagnostic label, related factors, and defining characteristics. For example, “Acute Pain related to surgical incision as evidenced by patient report of pain at 7/10, guarding behavior, and increased heart rate.”
2. Risk Nursing Diagnosis: A risk diagnosis describes potential problems that a patient is vulnerable to developing. It’s based on risk factors that increase the patient’s susceptibility to a problem. Risk diagnoses do not have defining characteristics or related factors but instead have risk factors linked to the diagnostic label by “as evidenced by.” For example, “Risk for Infection as evidenced by surgical incision, compromised immune system, and presence of invasive lines.”
3. Health Promotion Nursing Diagnosis: This type focuses on a patient’s desire or motivation to improve their health and well-being. It’s used when a patient is ready to enhance their current health practices. Health promotion diagnoses typically have only a diagnostic label, but related factors can be added for clarity. For example, “Readiness for Enhanced Nutrition as evidenced by patient expressing interest in learning about healthy eating and requesting nutritional information.”
4. Syndrome Nursing Diagnosis: A syndrome diagnosis represents a cluster of nursing diagnoses that occur together and are best addressed collectively. These diagnoses are also written as a one-part statement, consisting only of the diagnostic label. For example, “Rape Trauma Syndrome” which encompasses a range of diagnoses like Anxiety, Fear, and Sleep Disturbance related to the trauma of sexual assault.
Choosing the correct type of nursing diagnosis is essential for directing appropriate nursing interventions. Problem-focused diagnoses require interventions to alleviate existing problems, risk diagnoses require preventative measures, health promotion diagnoses require support and education to enhance wellness, and syndrome diagnoses require a comprehensive approach to address the cluster of associated problems.
Key Components for Formulation: Building Blocks of a Nursing Diagnosis
Creating a nursing diagnosis involves understanding its essential components. A well-structured nursing diagnosis typically includes three parts: the Problem (Diagnostic Label), the Etiology (Related Factors), and the Signs and Symptoms (Defining Characteristics).
1. Problem (Diagnostic Label): This component is a concise term or phrase that represents the patient’s health problem or response. It’s a standardized label from a recognized taxonomy, such as NANDA-I (North American Nursing Diagnosis Association International). The diagnostic label usually has two parts: the qualifier and the focus of the diagnosis. Qualifiers add specific meaning to the label (e.g., “Deficient,” “Impaired,” “Ineffective,” “Risk for”). The focus of the diagnosis pinpoints the area of concern (e.g., “Fluid Volume,” “Gas Exchange,” “Tissue Perfusion,” “Injury”). For example, in “Ineffective Airway Clearance,” “Ineffective” is the qualifier, and “Airway Clearance” is the focus.
2. Etiology (Related Factors): The etiology identifies the probable cause(s) or contributing factors to the patient’s health problem. These are the factors that have led to or are associated with the nursing diagnosis. Identifying the etiology is crucial because it directs nursing interventions towards addressing the underlying cause. The etiology is linked to the problem statement using the phrase “related to.” For example, in “Acute Pain related to surgical incision,” “surgical incision” is the etiology. Nursing interventions will then be directed towards managing pain associated with the surgical incision.
3. Signs and Symptoms (Defining Characteristics): Defining characteristics are the observable cues, signs, and symptoms that cluster together as evidence of the nursing diagnosis. These are the patient’s subjective and objective data that validate the presence of an actual nursing diagnosis. For risk diagnoses, risk factors take the place of defining characteristics and indicate vulnerability. Defining characteristics are linked to the problem and etiology using the phrase “as evidenced by” or “as manifested by.” For example, in “Acute Pain related to surgical incision as evidenced by patient report of pain at 7/10, guarding behavior, and increased heart rate,” the patient’s report of pain, guarding behavior, and increased heart rate are the defining characteristics.
Understanding and correctly identifying these three components are crucial for creating comprehensive and accurate nursing diagnoses. Each component plays a vital role in guiding care planning and ensuring that interventions are targeted and effective.
The Diagnostic Process: A Step-by-Step Approach to Creating Nursing Diagnoses
The process of creating a nursing diagnosis involves three key phases: Data Analysis, Problem Identification, and Diagnostic Statement Formulation.
1. Data Analysis: This initial phase involves examining the data collected during the nursing assessment. It includes three main steps:
* **Comparing Data to Standards:** Nurses compare the collected patient data against established norms and standards. This helps identify significant deviations from health or wellness. For instance, comparing a patient's blood pressure to normal ranges helps identify hypertension or hypotension.
* **Clustering Cues:** Nurses group related cues or pieces of data together to identify patterns. This clustering helps in recognizing potential health problems. For example, clustering cues like shortness of breath, fatigue, and chest pain might indicate a problem related to cardiac function.
* **Identifying Gaps and Inconsistencies:** Nurses look for any missing information or inconsistencies in the data. Gaps in data may require further assessment, while inconsistencies need clarification. For example, if a patient reports no pain but exhibits guarding behavior, further assessment is needed to clarify the pain status.2. Problem Identification: After analyzing the data, nurses identify potential health problems, risks, and strengths. This involves:
* **Identifying Health Problems:** Based on the clustered cues and data analysis, nurses identify actual or potential health problems that require nursing intervention. This step involves determining if the identified problem is a nursing diagnosis, medical diagnosis, or collaborative problem.
* **Identifying Strengths and Resources:** It's equally important to identify the patient's strengths, resources, and coping mechanisms. These strengths can be leveraged in the care plan to promote patient resilience and recovery. For example, identifying a patient's strong family support system can be a valuable resource in their care.
* **Ruling Out Medical Diagnoses and Collaborative Problems:** Nurses must differentiate between problems they can independently address (nursing diagnoses) and those requiring medical interventions or collaborative management. This distinction ensures appropriate care planning and referral when necessary.3. Diagnostic Statement Formulation: This final phase involves creating a clear and concise nursing diagnostic statement. This includes:
* **Choosing a Standardized Diagnostic Label:** Nurses select a standardized label from a recognized taxonomy like NANDA-I that accurately represents the identified health problem.
* **Determining Related Factors or Risk Factors:** For actual diagnoses, nurses identify related factors (etiology). For risk diagnoses, they identify risk factors. These factors should be causally linked to the diagnostic label.
* **Writing the Diagnostic Statement:** Nurses combine the diagnostic label, related factors (or risk factors), and defining characteristics (for actual diagnoses) into a structured statement. This statement can be in a two-part (for risk diagnoses) or three-part (for actual diagnoses) format.By following these three phases systematically, nurses can ensure a thorough and accurate diagnostic process, leading to effective and patient-centered care plans.
Writing Effective Nursing Diagnostic Statements: Formats and Examples
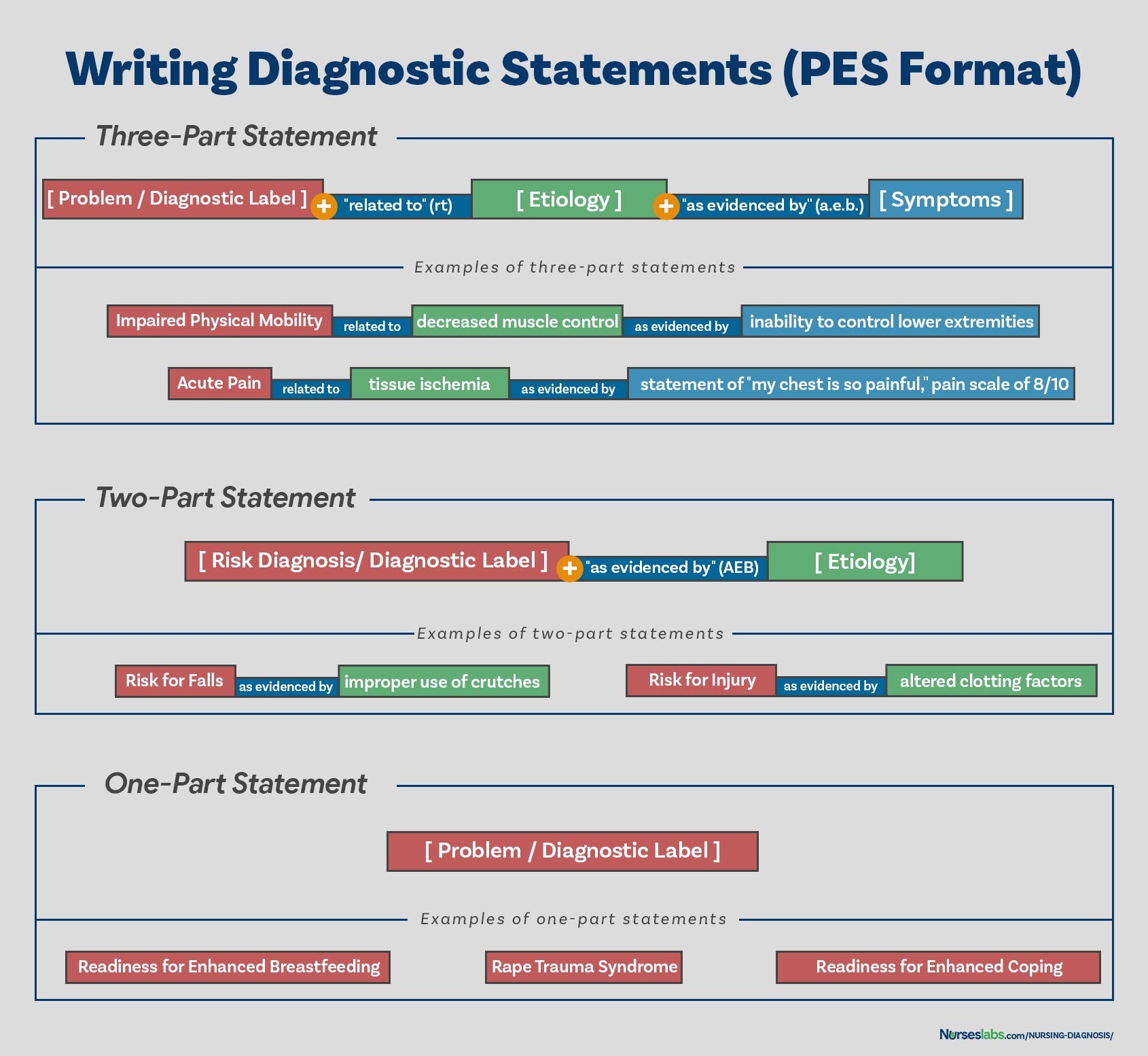
Formulating a nursing diagnosis involves writing a clear and precise diagnostic statement. The structure of this statement varies depending on the type of nursing diagnosis. The PES format (Problem, Etiology, Signs/Symptoms) is a common framework used for writing diagnostic statements, particularly for actual or problem-focused diagnoses.
WRITING DIAGNOSTIC STATEMENTS. Your guide on how to write different nursing diagnostic statements.
1. One-Part Nursing Diagnosis Statement: Health promotion and syndrome diagnoses are typically written as one-part statements, including only the diagnostic label.
* **Health Promotion Diagnosis Example:** "Readiness for Enhanced Coping"
* **Syndrome Diagnosis Example:** "Rape Trauma Syndrome"2. Two-Part Nursing Diagnosis Statement: Risk and possible nursing diagnoses are written as two-part statements. For risk diagnoses, it includes the diagnostic label and risk factors, connected by “as evidenced by.” Possible diagnoses also use a two-part statement but are less frequently used in practice.
* **Risk Diagnosis Example:** "Risk for Infection as evidenced by weakened immune system response"
* **Risk Diagnosis Example:** "Risk for Injury as evidenced by unstable hemodynamic profile"3. Three-Part Nursing Diagnosis Statement: Actual or problem-focused nursing diagnoses are written as three-part statements using the PES format:
* **Problem (P): Diagnostic Label:** This is the NANDA-I approved diagnostic label.
* **Etiology (E): Related Factors:** These are the factors contributing to the problem, linked by "related to."
* **Signs and Symptoms (S): Defining Characteristics:** These are the observable cues that validate the diagnosis, linked by "as evidenced by" or "as manifested by."
* **Example of Three-Part (PES) Statement:** "Ineffective Airway Clearance related to increased mucus production as evidenced by adventitious breath sounds and cough."
{width=1690 height=1554}
*PES FORMAT. Writing nursing diagnoses using the PES format.*Variations in Basic Statement Formats:
* **Using "Specify":** Sometimes, adding specificity to the diagnostic label enhances clarity. For instance, "Impaired Physical Mobility related to musculoskeletal impairment affecting lower extremities."
* **Using "Secondary to":** When the etiology is secondary to a medical diagnosis, it can be included for clarity. For example, "Deficient Knowledge related to newly diagnosed diabetes mellitus secondary to lack of prior education."
* **Two Diagnostic Labels:** In some cases, two diagnostic labels might be used to fully describe the patient's response. For example, "Anxiety and Fear related to upcoming surgery."Writing effective diagnostic statements requires practice and familiarity with NANDA-I terminology. Accurate statements are crucial for guiding individualized care and achieving positive patient outcomes.
Practical Tips for Creating Accurate and Effective Nursing Diagnoses
Creating accurate and effective nursing diagnoses is a skill that improves with practice. Here are some practical tips to enhance your diagnostic abilities:
- Focus on Patient Response: Always focus on the patient’s response to their health condition, not just the medical diagnosis. Nursing diagnoses address how the patient is affected by the illness or situation.
- Use Standardized Language: Utilize NANDA-I approved diagnostic labels to ensure clear communication and consistency in documentation. Familiarize yourself with the NANDA-I taxonomy and regularly update your knowledge as new diagnoses are added or revised.
- Be Specific and Precise: Avoid vague or broad statements. Be as specific as possible in describing the problem, etiology, and defining characteristics. Specificity leads to more targeted and effective interventions.
- Base Diagnoses on Assessment Data: Ensure that your diagnoses are directly supported by your assessment data. Every component of the diagnostic statement should be validated by the data you have collected.
- Avoid Medical Diagnoses in Nursing Diagnoses: Do not include medical diagnoses within your nursing diagnostic statement. Nursing diagnoses are distinct from medical diagnoses and focus on patient responses, not diseases themselves.
- Determine Treatable Etiologies: Ensure that the etiology (related factors) is something that nurses can address with nursing interventions. The goal is to identify factors that are modifiable through nursing care.
- Involve the Patient: When possible, involve the patient in the diagnostic process. Patient input can provide valuable insights into their experience and help validate the accuracy of the diagnosis.
- Validate Diagnoses: Review and validate your diagnoses with experienced nurses or preceptors. Seek feedback to refine your diagnostic reasoning skills and ensure accuracy.
- Continuously Review and Update: Nursing diagnoses are not static. Regularly review and update diagnoses based on changes in the patient’s condition and response to interventions.
- Use Resources: Utilize nursing diagnosis handbooks, online resources, and decision trees to assist in the diagnostic process. These resources can provide guidance in selecting appropriate labels and identifying related factors and defining characteristics.
- Practice Regularly: The more you practice creating nursing diagnoses, the more proficient you will become. Engage in case studies, simulations, and real-patient scenarios to hone your diagnostic skills.
By following these tips and continuously practicing, nurses can improve their ability to create accurate and effective nursing diagnoses, leading to enhanced patient care and outcomes.
Utilizing Nursing Diagnosis in Care Planning
Nursing diagnoses are the linchpin of the nursing care plan. They provide the framework for developing individualized, patient-centered care. Once nursing diagnoses are identified, they directly guide the subsequent steps of the nursing process: planning, implementation, and evaluation.
In the planning phase, nursing diagnoses are used to formulate patient goals and expected outcomes. Goals should be patient-centered, measurable, achievable, realistic, and time-bound (SMART). Nursing diagnoses ensure that goals are directly related to the patient’s identified health problems and responses. For each nursing diagnosis, specific goals are set to counteract the problem stated in the diagnosis.
For example, for the nursing diagnosis “Acute Pain related to surgical incision,” a patient-centered goal might be: “Patient will report pain level of 3 or less on a 0-10 scale within 2 hours after pain medication administration.” This goal is directly derived from the nursing diagnosis and sets a measurable outcome for pain management.
In the implementation phase, nursing diagnoses guide the selection of appropriate nursing interventions. Interventions are actions that nurses take to achieve the patient goals and resolve the identified problems. Interventions should be evidence-based, safe, and tailored to the patient’s needs and preferences. The etiology component of the nursing diagnosis is particularly useful in guiding intervention selection, as interventions should aim to address the root causes of the problem.
Continuing with the “Acute Pain” example, interventions might include: administering prescribed analgesics, using non-pharmacological pain relief measures (e.g., positioning, relaxation techniques), assessing pain regularly, and educating the patient about pain management. These interventions are directly aimed at managing pain related to the surgical incision, as stated in the nursing diagnosis.
In the evaluation phase, the effectiveness of the nursing care is evaluated based on the achievement of patient goals and resolution of nursing diagnoses. Evaluation involves reassessing the patient to determine if the goals have been met and if the nursing diagnosis has been resolved or improved. If goals are not met, the nursing process is revised, which may involve modifying the nursing diagnosis, goals, or interventions.
Nursing diagnoses, therefore, are not just labels but are dynamic and integral to the entire nursing process. They ensure that care is focused, personalized, and outcome-driven. By accurately creating and utilizing nursing diagnoses, nurses can significantly enhance the quality and effectiveness of patient care.
Recommended Resources for Further Learning
To deepen your understanding and skills in creating nursing diagnoses, consider these recommended resources:
Books:
-
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: This handbook is praised for its evidence-based approach and user-friendly three-step system for client assessment, nursing diagnosis, and care planning. It’s an excellent resource for building diagnostic reasoning and critical thinking skills.
-
Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition): This comprehensive guide includes over two hundred care plans reflecting the latest evidence-based guidelines, including ICNP diagnoses and care plans on contemporary health issues.
-
Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: A quick-reference tool ideal for identifying correct diagnoses and planning efficient patient care. The latest edition includes updated nursing diagnoses and interventions for a wide range of disorders.
-
Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: This manual is invaluable for planning, individualizing, and documenting care for over 800 diseases and disorders. It provides detailed information for each diagnosis, including sample clinical applications and prioritized interventions.
-
All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health: This e-book offers over 100 care plans across various specialties, focusing on interprofessional patient problems to enhance communication and collaborative care.
Online Resources:
- NANDA-I Website: The official website of NANDA-I provides access to the latest nursing diagnoses, resources, and updates on diagnostic terminology.
- Nursing Journals and Databases: Explore journals like Nursing Diagnosis Quarterly and databases like CINAHL for research articles and scholarly discussions on nursing diagnoses.
- Online Nursing Forums and Communities: Engage with other nurses in online forums and communities to discuss challenging diagnoses and share best practices.
These resources can provide ongoing support and learning opportunities to master the art and science of creating nursing diagnoses and applying them effectively in nursing practice.
Conclusion
Mastering the creation of nursing diagnoses is fundamental for every nurse. It is the critical step that transforms patient assessment data into a roadmap for individualized care. By understanding the definition, purpose, types, components, and process of formulating nursing diagnoses, you equip yourself with the tools to provide holistic, patient-centered care. Accurate nursing diagnoses not only guide effective interventions and care planning but also enhance communication within the healthcare team and contribute to improved patient outcomes. Continuous learning, practice, and utilization of available resources are key to refining your diagnostic skills and ensuring excellence in nursing practice.
References and Sources
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.