Cryptococcal meningitis (CM) poses a significant global health challenge, particularly for individuals with compromised immune systems. Accurate and timely laboratory diagnosis is crucial for effective management and improved patient outcomes. This article provides an in-depth overview of the essential laboratory diagnostic methods for cryptococcal meningitis, emphasizing their strengths, limitations, and clinical applications.
Cerebrospinal Fluid (CSF) Culture: The Gold Standard
CSF culture remains the definitive diagnostic test for cryptococcal meningitis, serving as the gold standard against which other methods are compared. This technique involves culturing CSF samples to allow for the growth and identification of Cryptococcus species.
Procedure and Methodology
The process involves inoculating CSF onto mycological media, such as Sabouraud dextrose agar, and incubating it at appropriate temperatures. Quantitative CSF cultures, a valuable tool in research and increasingly in clinical settings, involve serial dilutions of CSF to quantify the fungal burden. This is typically performed using a simple technique with a 100-μl CSF input volume, serial dilutions, and plating on agar.
Advantages of CSF Culture
- High Specificity: Culture definitively identifies viable Cryptococcus organisms, confirming the diagnosis.
- Strain Identification and Susceptibility Testing: Culture allows for species identification and antifungal susceptibility testing, guiding treatment strategies, especially in cases of treatment failure or suspected resistance.
- Quantitative Analysis: Quantitative cultures provide crucial prognostic information. Higher initial fungal burden is associated with increased mortality risk. Monitoring quantitative culture trends during treatment helps assess treatment efficacy and CSF clearance.
Limitations of CSF Culture
- Prolonged Turnaround Time: Culture requires incubation, and definitive results can take several days, sometimes up to two weeks. This delay can be critical in a rapidly progressive infection like CM.
- Lower Sensitivity Compared to CrAg: In early stages of infection or with low fungal loads, culture sensitivity may be lower than antigen detection methods.
Despite these limitations, CSF culture remains indispensable for confirming the diagnosis and providing essential information for patient management.
India Ink Microscopy: A Rapid but Less Sensitive Test
India ink microscopy is a historically significant, rapid, and low-resource method for the presumptive diagnosis of cryptococcal meningitis. It relies on the unique morphology of Cryptococcus and its capsule.
Principle of India Ink Stain
India ink is a negative stain. When mixed with CSF, the ink particles are excluded by the thick polysaccharide capsule of Cryptococcus, creating a clear halo effect around the yeast cells when viewed under a light microscope. This halo effect makes the encapsulated yeast cells visible against the dark background of the ink.
Advantages of India Ink Microscopy
- Rapidity: India ink preparation and microscopy can be performed quickly, providing immediate preliminary diagnostic information, often within minutes.
- Low Cost and Accessibility: India ink is inexpensive and readily available, making it particularly useful in resource-limited settings where advanced diagnostic facilities may be scarce.
- Simplicity: The procedure is simple to perform and does not require specialized equipment beyond a light microscope.
Limitations of India Ink Microscopy
- Lower Sensitivity: The sensitivity of India ink microscopy is significantly lower than other methods, particularly when performed by non-experts. Studies report sensitivities ranging from 50-86% in expert hands, meaning a considerable proportion of cases can be missed. Sensitivity is even lower in early infections with low fungal burdens.
- Subjectivity: Interpretation of India ink slides can be subjective and depends on the expertise of the microscopist.
- Cannot Differentiate Cryptococcus Species: India ink only detects the presence of encapsulated yeast; it does not identify the specific Cryptococcus species.
While India ink microscopy can be a useful initial screening tool, its limitations, especially the lower sensitivity, necessitate the use of more sensitive and specific tests like CrAg assays for definitive diagnosis and to avoid false negatives.
Cryptococcal Antigen (CrAg) Testing: Highly Sensitive and Specific
Cryptococcal antigen (CrAg) testing has revolutionized the diagnosis of cryptococcal meningitis due to its high sensitivity, specificity, and the development of rapid point-of-care assays. CrAg tests detect the polysaccharide capsule antigen of Cryptococcus in CSF and blood.
Latex Agglutination: Traditional Lab-Based CrAg Test
Latex agglutination was the traditional method for CrAg detection. It involves mixing patient samples with latex particles coated with antibodies against cryptococcal antigen. If CrAg is present, agglutination (clumping) of the latex particles occurs, indicating a positive result.
Advantages of Latex Agglutination
- High Sensitivity and Specificity: Historically, latex agglutination CrAg tests demonstrated very high sensitivity and specificity (>99%). However, more recent studies have shown slightly lower but still excellent performance.
- Semi-quantitative Results: Titers can be obtained by serial dilutions, providing an indication of antigen load.
Disadvantages of Latex Agglutination
- Laboratory Infrastructure Required: Latex agglutination requires a laboratory setting, trained personnel, electricity, and refrigeration for reagents, limiting its use in resource-limited settings.
- Longer Turnaround Time: The test process, including sample preparation and result interpretation, typically takes several hours.
- Cold Chain Dependency: Reagents require cold-chain shipping and storage, adding to the logistical and cost challenges, especially in low-income countries.
- Becoming Archaic: Compared to newer lateral flow assays, latex agglutination is generally considered more expensive, labor-intensive, and less practical.
CrAg Lateral Flow Assay (LFA): Point-of-Care Revolution
The CrAg lateral flow assay (LFA) is an immunochromatographic dipstick test that has transformed cryptococcal meningitis diagnosis, particularly in resource-limited settings.
Principle of CrAg LFA
The LFA is a point-of-care test that can be performed on CSF, serum, plasma, or even fingerstick whole blood. It contains gold-conjugated anti-cryptococcal antibodies. If CrAg is present in the sample, it binds to these antibodies, and the complex migrates along the test strip. A visible line appears in the test region if the antigen is present, indicating a positive result.
Advantages of CrAg LFA
- Point-of-Care Testing: LFA can be performed at the patient’s bedside or in clinics without laboratory infrastructure, significantly improving access to diagnosis, especially in remote areas.
- Rapid Results: Results are available within 10-20 minutes, enabling prompt clinical decision-making and treatment initiation.
- High Sensitivity and Specificity: CrAg LFA demonstrates excellent sensitivity and specificity, comparable to or even better than CSF culture and latex agglutination. Studies show sensitivities around 99% and specificities exceeding 99% in CSF.
- Ease of Use: The test is simple to perform, requiring minimal training. Semiskilled healthcare workers can accurately perform and interpret the test.
- No Refrigeration Required: LFA reagents do not require refrigeration, simplifying logistics and reducing costs, particularly in settings with unreliable cold chains.
Clinical Impact of CrAg LFA
The introduction of CrAg LFA has had a profound impact on cryptococcal meningitis management:
- Early Diagnosis and Treatment: Rapid point-of-care diagnosis allows for earlier initiation of antifungal therapy, improving patient outcomes and reducing mortality.
- Screening Programs: CrAg LFA facilitates screening programs for cryptococcal antigenemia in high-risk populations, such as HIV-infected individuals, enabling pre-emptive treatment and preventing progression to meningitis.
- Streamlined Care: In resource-limited settings, combining diagnostic CrAg LFA testing with the first therapeutic lumbar puncture can streamline care, especially where access to lumbar punctures is challenging. Using blood CrAg LFA can guide the need for lumbar puncture.
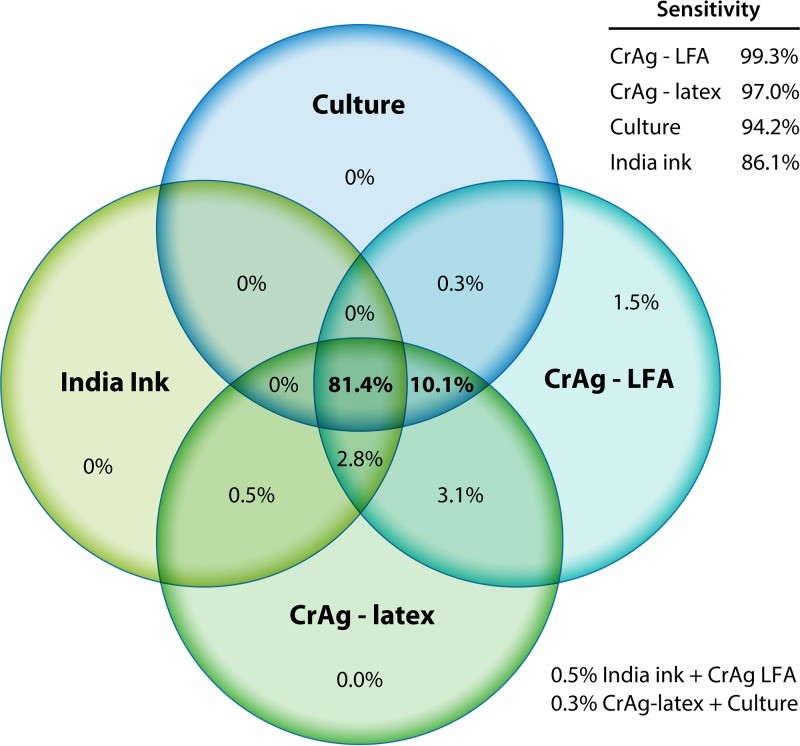
Figure 1: Distribution of CSF Diagnostic Testing in Uganda and South Africa. This Venn diagram illustrates the overlap and unique contributions of different CSF diagnostic tests for cryptococcal meningitis in a large study population. CrAg LFA demonstrated superior sensitivity in detecting cases compared to other methods.
Commercially Available CrAg LFA Tests
Several CrAg LFA tests are commercially available, with varying levels of validation and regulatory approvals. The Immy CrAg LFA (FDA-approved and CE-marked) is the most extensively validated and widely used globally. Other tests, such as Biosynex CryptoPS LFA and StrongStep CrAg LFA, are also available but may have more limited validation data or specific limitations, such as lower specificity in plasma for some tests. Clinicians should be aware of the performance characteristics of the specific LFA test they are using.
Blood CrAg Testing for Meningitis Detection
CrAg testing in blood, particularly using the LFA, has emerged as a valuable tool for detecting cryptococcal antigenemia and indirectly for identifying individuals at high risk of developing or having cryptococcal meningitis.
Utility of Blood CrAg LFA
- Screening for Cryptococcal Antigenemia: Blood CrAg LFA is highly effective for screening HIV-positive individuals for cryptococcal antigenemia. A positive blood CrAg test in asymptomatic individuals indicates the need for pre-emptive antifungal therapy to prevent progression to CM.
- Predictive Value for Meningitis: A positive blood CrAg test in patients with suspected meningitis is highly predictive of cryptococcal meningitis. In settings where immediate lumbar puncture is not feasible, a positive blood CrAg LFA can strongly suggest CM and guide initial management.
- Facilitating Therapeutic Lumbar Puncture: Point-of-care fingerstick CrAg LFA allows for rapid diagnosis before lumbar puncture. A positive result confirms the need for therapeutic lumbar puncture to relieve intracranial pressure, a critical aspect of CM management.
Figure 2: Positivity Distribution by Blood CrAg, CSF CrAg, and CSF Culture. This diagram shows the concordance and discordance between blood CrAg LFA, CSF CrAg LFA, and CSF culture in diagnosing cryptococcal meningitis. Fingerstick blood CrAg LFA shows high positive predictive value for detecting CrAg in blood and for cryptococcal meningitis.
Limitations of Blood CrAg Testing
- False Negatives in Early or Low Burden Disease: In asymptomatic individuals with very low fungal burdens, blood CrAg LFA may yield false negative results compared to serum or plasma testing.
- Not a Direct Meningitis Diagnostic: Blood CrAg testing is not a direct diagnostic test for meningitis itself. While a positive blood CrAg strongly suggests the likelihood of CM, CSF examination is still required to confirm meningitis and assess CSF parameters.
Despite these limitations, blood CrAg testing, especially with the LFA, is a crucial advancement in cryptococcal disease management, enabling proactive screening and rapid risk stratification.
Other Advanced Diagnostic Methods
In high-income settings, more advanced molecular diagnostic methods are available, although their routine use for cryptococcal meningitis diagnosis may be limited due to cost and complexity.
PCR-Based Assays
Multiplex PCR panels, such as the FilmArray meningitis/encephalitis panel, can detect Cryptococcus DNA in CSF along with other bacterial and viral pathogens. PCR offers rapid detection and high sensitivity, particularly when fungal burden is adequate. However, the expense of multiplex PCR may not justify its use solely for cryptococcal diagnosis, especially when CrAg LFA is readily available and cost-effective. PCR can be valuable in complex cases or when differential diagnosis with other meningitis etiologies is needed.
MALDI-TOF Mass Spectrometry
Matrix-assisted laser desorption ionization–time-of-flight mass spectrometry (MALDI-TOF) is another advanced technique reported to detect Cryptococcus directly from clinical specimens. MALDI-TOF is primarily used for rapid identification of cultured isolates but may have potential applications for direct detection in CSF in the future.
Conclusion: Optimizing Cryptococcal Meningitis Lab Diagnosis
Accurate and timely laboratory diagnosis is paramount for effective management of cryptococcal meningitis. While CSF culture remains the gold standard for definitive diagnosis and antifungal susceptibility testing, CrAg testing, particularly the point-of-care LFA, has revolutionized the diagnostic landscape. CrAg LFA offers rapid, highly sensitive, and specific diagnosis, especially valuable in resource-limited settings and for point-of-care applications. Blood CrAg testing plays a crucial role in screening and risk stratification. Clinicians should utilize these diagnostic tools strategically to ensure prompt diagnosis, appropriate treatment, and improved outcomes for patients with or at risk of cryptococcal meningitis. Integrating rapid and accessible diagnostic methods like CrAg LFA into routine clinical practice and public health programs is essential to combat the global burden of this life-threatening fungal infection.
References
[5] – (Reference to original article #5)
[6] – (Reference to original article #6)
[7] – (Reference to original article #7)
[8] – (Reference to original article #8)
[9] – (Reference to original article #9)
[10] – (Reference to original article #10)
[11] – (Reference to original article #11)
[12] – (Reference to original article #12)
[13] – (Reference to original article #13)
[14] – (Reference to original article #14)
[15] – (Reference to original article #15)
[16] – (Reference to original article #16)
[17] – (Reference to original article #17)
[18] – (Reference to original article #18)
[19] – (Reference to original article #19)