Mastocytosis encompasses a spectrum of disorders marked by an abnormal accumulation of mast cells in various tissues, primarily the skin and sometimes internal organs. In children, mastocytosis often manifests differently compared to adults, typically appearing before the age of two and predominantly affecting the skin. Urticaria pigmentosa (UP) represents the most common form in pediatric patients. Understanding the nuances of Cutaneous Mastocytosis Diagnosis in children is crucial for accurate identification and appropriate management, distinct from approaches used for adults. This article provides an in-depth guide to diagnosing cutaneous mastocytosis in pediatric populations.
The initial descriptions of cutaneous mast cell disease date back to the late 19th century, with Nettleship and Tay’s early observations and Sangster’s subsequent term, urticaria pigmentosa. Later, Ellis’s autopsy report on a fatal pediatric case highlighted systemic involvement, broadening the understanding of mastocytosis beyond skin manifestations. Over time, classifications evolved, culminating in the contemporary World Health Organization (WHO) classification system.
Given the distinct presentation and prognosis of pediatric mastocytosis compared to adult forms, it’s vital to adopt a child-centric approach to diagnosis and management. Relying on adult guidelines can be misleading, particularly in therapeutic decisions where anti-proliferative agents carry different risk profiles in children, especially concerning long-term effects. This review focuses on providing age-specific guidance for diagnosing and caring for children with mastocytosis.
Recognizing Cutaneous Mastocytosis in Children: Clinical Presentation
Pediatric cutaneous mastocytosis can present as early as the neonatal period or infancy. Current data suggests an equal prevalence in males and females across all races, with familial occurrences being infrequent. Mast cell mediator-related symptoms are observed in over 60% of pediatric cases, underscoring the importance of recognizing these signs in diagnosis.
While the exact cause of cutaneous mastocytosis in children remains unclear, many pediatric patients lack the c-kit mutations commonly found in adults with systemic mastocytosis. KIT, a receptor crucial for mast cell function, is encoded by c-kit. However, studies have identified c-kit mutations in skin biopsies of some children with cutaneous mastocytosis, including mutations at codons 816, 820, and 839. Activating mutations at codon 816, such as Asp816Val and Asp816Phe, are found in UP, mastocytomas, and diffuse cutaneous mastocytosis (DCM). Notably, the Asp816Phe mutation appears associated with an earlier disease onset compared to the Asp816Val mutation. These genetic findings can aid in understanding the pathogenesis but are not routinely required for diagnosis.
Diagnostic Classification of Cutaneous Mastocytosis in Children
Urticaria pigmentosa (UP) is the most prevalent form of cutaneous mastocytosis in children, accounting for 70–90% of cases. UP lesions are typically reddish-brown to yellowish, ranging from millimeters to a few centimeters in diameter. They appear as multiple macules, plaques, or nodules across the skin. Rubbing or stroking these lesions can induce erythema, swelling, and blister formation, accompanied by itching and dermatographism. Flushing is also seen in a significant portion of UP patients. Darier’s sign, characterized by wheal and flare upon lesion manipulation, is a hallmark diagnostic feature. UP lesions predominantly affect the trunk and extremities, with less involvement of palms, soles, scalp, face, and sun-exposed areas. Onset of UP lesions typically occurs in early infancy, with most cases appearing before six months of age. Importantly, lesions often resolve spontaneously by puberty if onset is in childhood, whereas lesions appearing after age 10 tend to persist. Systemic symptoms and visceral involvement are uncommon in UP, though wheezing and syncope can occur.
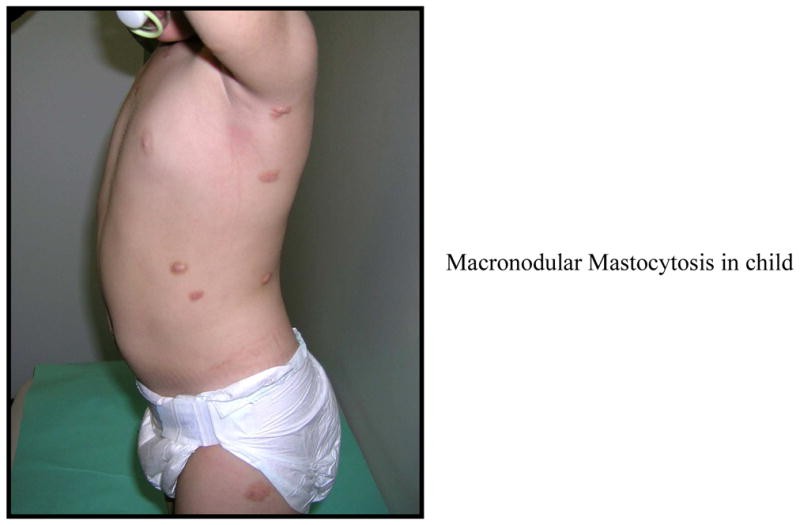
Mastocytomas, or nodular lesions, represent another form of cutaneous mastocytosis, occurring in 10–35% of pediatric cases. These lesions are similar to UP but larger, sometimes vesiculating or blistering. Solitary mastocytomas are often present at birth or develop shortly after. Like UP, mastocytomas usually resolve by puberty, though persistence into adulthood is possible. Systemic involvement is rare with mastocytomas, and Darier’s sign is typically positive.
FIGURE 1.
Diffuse cutaneous mastocytosis (DCM) is a less common but more severe variant, accounting for 1–3% of pediatric cutaneous mastocytosis cases. DCM can affect the entire skin surface, often most prominently on the central body and scalp. It can be congenital or appear in early infancy. Blistering, including hemorrhagic blisters, is a common presenting symptom. The skin may become thickened and leathery, with persistent hyperpigmentation and marked dermatographism. Extensive bullae can rupture, leading to erosions and crusts. DCM is associated with a higher risk of systemic symptoms due to widespread mast cell mediator release, potentially causing flushing, itching, diarrhea, intestinal bleeding, hypotension, anemia, and even shock. Visceral involvement, such as lymphadenopathy and hepatomegaly, can also occur.
FIGURE 2.
Telangiectasia macularis eruptiva perstans (TMEP) is the rarest form of cutaneous mastocytosis in children, characterized by red, telangiectatic macules on a tan or brown background. It can sometimes coexist with UP.
All forms of cutaneous mastocytosis in children can, although rarely, present with acute mast cell activation events, including anaphylaxis. These events can manifest as whole-body flushing, breathing difficulties, wheezing, nausea, vomiting, diarrhea, and hypotension. Cyanotic episodes have also been reported in some cases.
FIGURE 3.
Histopathological Examination in Cutaneous Mastocytosis Diagnosis
Histopathology plays a crucial role in confirming the diagnosis of cutaneous mastocytosis. In UP, an increased number of mast cells is observed in the papillary dermis, although standardized quantification is lacking. Mast cells tend to cluster around blood vessels and may be associated with eosinophils. In mastocytomas and nodular UP, mast cell infiltration can extend throughout the dermis and into subcutaneous tissues. Electron microscopy reveals both round and spindle-shaped mast cells that stain positive for tryptase and chymase, sometimes in a sheet-like pattern. Mast cell counts can be significantly elevated, up to tenfold higher than in normal skin. Notably, even non-lesional skin in patients with UP and mastocytomas shows higher mast cell numbers compared to healthy controls.
Mast Cell Mediator-Related Symptoms: Diagnostic Clues
All forms of cutaneous mastocytosis can present with symptoms stemming from the release of mast cell mediators. Darier’s sign, a key clinical feature, is attributed to the release of histamine, leukotrienes, and prostaglandins from mast cells in the skin. However, the presence and intensity of symptoms do not always correlate with the extent of skin involvement. Patients with limited skin lesions, such as a single mastocytoma or few UP lesions, can still experience significant symptoms. Skin symptoms include flushing, itching, redness, and swelling, which can be spontaneous or triggered. Flushing episodes are common, but hypotension is less frequent. Anaphylactic reactions to insect stings have been reported in adolescents with UP, but immunotherapy safety and efficacy in this age group are not well-established.
Gastrointestinal symptoms are also prominent, with abdominal pain and diarrhea affecting up to 40% of children. While hyperacidity and peptic ulcers are reported, peptic ulcer disease is rare in children. Severe complications like blistering, bullae, prolonged bleeding, and hypotensive episodes are more characteristic of DCM but uncommon in UP and mastocytomas. Elevated levels of histamine metabolites in urine from children with UP and mastocytomas provide further evidence of mast cell degranulation.
Correlation of Cutaneous Findings with Systemic Involvement and Tryptase Levels in Diagnosis
Initial bone marrow evaluations in children with cutaneous mastocytosis, predominantly UP, have generally shown no adult-type mast cell aggregates, suggesting limited internal organ involvement in most pediatric cases. This finding has historically argued against routine bone marrow biopsies for prognosis in children with typical cutaneous mastocytosis. However, more recent studies exploring the relationship between cutaneous disease and systemic involvement reveal a more nuanced picture. While the extent and density of skin lesions in children and adults with cutaneous mastocytosis can be similar, children may present with larger UP lesions. Some children with cutaneous mastocytosis may have indolent systemic mastocytosis (ISM), but skin lesion characteristics alone are not predictive of systemic involvement. Serum tryptase levels, while not correlated with skin involvement, are significantly elevated in children with systemic disease. Thus, cutaneous presentation alone is not sufficient to rule out systemic disease, highlighting the heterogeneous nature of mastocytosis and the need for comprehensive diagnostic evaluation.
Tryptase levels generally correlate with mast cell burden in the skin, with higher levels often seen in more severe disease. However, elevated tryptase in children with cutaneous mastocytosis does not automatically indicate systemic involvement. Studies have shown a positive correlation between the extent of skin involvement, lesion appearance, associated symptoms (itching, flushing, Darier’s sign), and tryptase levels. Other mediators like histamine also correlate with skin mast cell numbers, but their levels are age-dependent in children.
Natural History of Cutaneous Mastocytosis: Implications for Diagnosis and Monitoring
Studies on the natural history of cutaneous mastocytosis in children indicate a tendency for spontaneous resolution before puberty. Lesion onset is typically early in life, often before six months of age. Darier’s sign is usually positive across different forms. Associated symptoms are common, including itching, flushing, and less frequently, palpitations, angioedema, hypotension, and cyanosis. Bullae are more frequent in mastocytomas. Temperature changes are a common trigger for symptoms. A significant proportion of children experience improvement or spontaneous resolution of their disease, particularly those with childhood-onset UP and mastocytomas. Long-term follow-up is essential to monitor disease course and identify any evolution towards systemic forms, although rare in pediatric cases.
Diagnostic Approach for Cutaneous Mastocytosis in Children
Diagnosing cutaneous mastocytosis in children requires clinical suspicion, particularly in cases of new skin lesions with or without mediator-related symptoms. The diagnostic process involves:
- Physical Examination: Assess skin lesions, document Darier’s sign.
- Serum Tryptase: Measure baseline serum tryptase levels.
- Complete Blood Count and Differential: Routine blood work to assess overall health.
- Skin Biopsy: A 3-mm punch biopsy is essential for histological confirmation. Staining should include hematoxylin & eosin and Giemsa, with immunostaining for tryptase and KIT. Consider c-kit mutation analysis of skin mast cells if available.
Skin biopsy findings compatible with cutaneous mastocytosis include:
- Aggregates of >20 mast cells.
- Mast cells with abnormal morphology.
- Presence of D816V c-kit mutation (if tested).
Further investigations are guided by clinical presentation and initial findings:
- Solitary Mastocytoma: If a single lesion is confirmed as mastocytoma by biopsy, typically no further studies are needed.
- UP, TMEP, DCM, or other forms:
- Selected Laboratory Tests: Repeat peripheral blood count, differential, platelet count, and routine biochemistries periodically (e.g., every 6-8 months or more frequently if symptoms are severe).
- Abdominal Ultrasound: Consider if organomegaly is suspected or in cases of severe systemic symptoms (GI, flushing, syncope, cyanotic spells), persistent skin lesions post-puberty, or clinical changes suggesting systemic involvement.
- Bone Marrow Biopsy and Aspirate: Recommended if there are severe, recurrent systemic symptoms, organomegaly, significant lymphadenopathy, persistent skin lesions after puberty, or clinical changes suggesting systemic involvement, or significantly elevated tryptase levels.
Table 1. Diagnostic Approach in Pediatric Mastocytosis
| For suspected cutaneous mastocytosis (multiple or single lesions) |
|---|
| Skin biopsy (3 mm punch): histology, mutational studies if possible |
| Compatible with diagnosis: aggregates of >20 mast cells +/− abnormal morphology, +D816V c-kit |
| If single lesion: mastocytoma, no further studies required |
| If UP, TEMP or other forms diagnosed, need: |
| Selected laboratory tests: peripheral blood count, differential and platelet count; routine biochemistries as required; baseline serum tryptase |
| Studies can be repeated every 6 to 8 months. If severe MC-mediator related symptoms are present, analytical studies may be repeated more frequently |
| Abdominal ultrasound if organomegaly suspected or with: |
| Severe systemic mast cell-mediators related symptoms: |
| GI, flushing, syncope or pre-syncope, cyanotic spells |
| Persistence of skin lesions after puberty |
| Clinical changes suggestive of systemic involvement |
| Bone marrow biopsy and aspirate if: |
| Severe recurrent systemic mast cell-mediators related symptoms: |
| GI, flushing, syncope or pre-syncope, cyanotic spells |
| Organomegaly or significant lymphadenopathy |
| Persistence of skin lesions after puberty |
| Clinical changes suggestive of systemic involvement |


Once a diagnosis of cutaneous mastocytosis is established, regular follow-up every 6 to 12 months is recommended. Parents should be informed about the low risk of progression to systemic mastocytosis in pediatric cases, while remaining vigilant for any concerning changes.
This comprehensive diagnostic approach ensures accurate identification of cutaneous mastocytosis in children, enabling timely and appropriate management strategies tailored to the specific needs of pediatric patients.