Excessive daytime sleepiness (EDS), also known as hypersomnolence, is a widespread condition that can significantly impact daily life and safety, particularly for professionals in demanding fields such as automotive repair and maintenance. Recognizing and properly diagnosing EDS is the first critical step towards effective management and ensuring safety, both on the job and on the road. This guide provides a practical overview of Daytime Sleepiness Diagnosis, tailored for automotive experts and based on current medical guidelines.
Understanding the Problem of Daytime Sleepiness
Excessive daytime sleepiness is more than just feeling a bit tired; it’s a persistent and overwhelming urge to sleep or feeling abnormally drowsy during waking hours. This can manifest in various ways, from struggling to concentrate and feeling sluggish to unintentionally falling asleep in inappropriate situations, such as while driving or during work tasks. For automotive professionals, who often operate heavy machinery, work with precision tools, and require constant vigilance, EDS poses significant risks. It can impair judgment, slow reaction times, and increase the likelihood of errors and accidents. The implications extend beyond workplace safety, affecting driving abilities and overall quality of life.
It’s crucial to understand that subjective self-assessment of sleepiness can be unreliable. Individuals may underestimate or deny their sleepiness, especially if they have become accustomed to feeling tired all the time. Often, it’s colleagues, family members, or even clients who first notice signs of EDS, such as nodding off during conversations or appearing unusually fatigued. Therefore, a comprehensive diagnostic approach is essential to accurately identify and address this condition.
Clinical Diagnostic Pathway
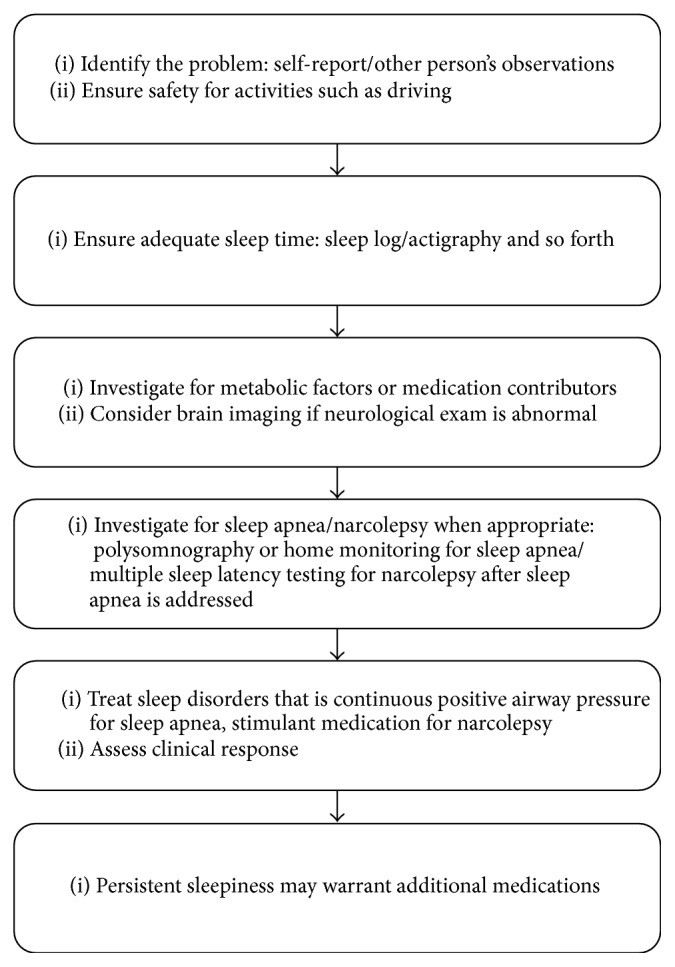 Clinical diagnostic pathway for excessive daytime sleepiness (EDS) in adult patients, outlining initial assessment, symptom evaluation, and testing methods.
Clinical diagnostic pathway for excessive daytime sleepiness (EDS) in adult patients, outlining initial assessment, symptom evaluation, and testing methods.
Identifying the Root Causes of Daytime Sleepiness
Pinpointing the cause of EDS is fundamental to accurate diagnosis and effective treatment. The differential diagnosis is broad, encompassing various lifestyle factors, medical conditions, and sleep disorders.
1. Insufficient Sleep: The most common culprit is simply not getting enough sleep. Adults generally require 7–9 hours of quality sleep per night. In the demanding automotive industry, with often irregular hours or long shifts, sleep deprivation can become chronic. If waking up consistently requires an alarm clock, it’s a strong indicator of insufficient sleep. Maintaining a sleep log, or utilizing sleep tracking apps and devices, can help monitor sleep patterns and identify potential deficits. Shift work, common in some automotive service roles, further disrupts the natural circadian rhythm, exacerbating sleepiness due to both cumulative sleep loss and working during naturally sleepy periods, such as the early morning hours.
2. Medical and Metabolic Factors: Various underlying medical conditions can contribute to EDS. Anemia and hypothyroidism are common examples, often presenting with fatigue as a primary symptom. Other metabolic disorders, including liver and kidney dysfunction, electrolyte imbalances, and systemic inflammation, can also induce sleepiness. A thorough medical examination and basic blood tests are typically sufficient to identify these medical causes.
3. Medication and Substance Use: Many medications, particularly psychoactive drugs, can induce drowsiness. Antidepressants, anxiety medications, pain relievers, and antiepileptic drugs are known to impair alertness. Over-the-counter medications, such as antihistamines found in many allergy and cold remedies, are also frequent causes of somnolence. Furthermore, alcohol and drug use can significantly contribute to daytime sleepiness. A careful review of a patient’s medication list and substance use habits is crucial in the diagnostic process.
4. Sleep Apnea (SA) and Upper Airway Resistance Syndrome (UARS): Obstructive sleep apnea is a highly prevalent sleep disorder characterized by repeated episodes of upper airway obstruction during sleep, leading to disrupted sleep and EDS. Risk factors include obesity, large neck circumference, and airway abnormalities. Snoring is a common symptom reported by those with sleep apnea. Upper airway resistance syndrome (UARS) is a related condition where subtle airway obstructions, even without significant oxygen desaturation or defined hypopneas, can fragment sleep and result in daytime sleepiness. Both conditions are critical to consider in the differential diagnosis of EDS.
5. Narcolepsy: Although less common, narcolepsy is a neurological disorder characterized by excessive daytime sleepiness, often accompanied by cataplexy (sudden muscle weakness triggered by strong emotions), sleep paralysis, and hypnagogic hallucinations. Narcolepsy affects approximately 1 in 2000 individuals. EDS is the defining symptom of narcolepsy, and while other symptoms may not always be present, their presence increases the likelihood of this diagnosis.
6. Neurological Conditions: Brain abnormalities, such as tumors or lesions affecting midline brain structures, can disrupt wakefulness and cause somnolence. Head injuries can also lead to reduced orexin/hypocretin signaling, similar to narcolepsy, resulting in EDS. Neurodegenerative conditions are also frequently associated with sleepiness. A comprehensive neurological examination and neuroimaging may be necessary to identify these less common causes of EDS.
Objective Measurement of Sleepiness
While subjective reports and clinical assessments are important, objective measures can provide valuable data in diagnosing and quantifying daytime sleepiness.
1. Epworth Sleepiness Scale (ESS): The ESS is a widely used, simple questionnaire consisting of eight questions that assess the likelihood of falling asleep in various everyday situations. Scores above 10 are generally considered indicative of clinically significant daytime sleepiness. While helpful as a screening tool, the ESS is subjective and should be complemented by more objective measures when possible.
2. Polysomnography (PSG): Polysomnography, or a sleep study, is not primarily used to directly quantify sleepiness. However, it is essential for evaluating for underlying sleep disorders that cause EDS, particularly obstructive sleep apnea. PSG is conducted in a sleep laboratory and involves monitoring various physiological parameters during sleep, including brain waves, eye movements, muscle activity, heart rate, and breathing. Ambulatory sleep monitoring devices may be sufficient in cases where sleep apnea is highly suspected. A PSG is a prerequisite for the Multiple Sleep Latency Test (MSLT).
3. Multiple Sleep Latency Test (MSLT): The MSLT is the gold standard neurophysiological test for objectively measuring daytime sleepiness, particularly in the diagnosis of narcolepsy. It is performed during the day following a full night of sleep recorded by PSG. During the MSLT, patients are given multiple opportunities (typically 4-5) to fall asleep in a quiet, dark room, spaced two hours apart. The time it takes to fall asleep (sleep latency) is measured. A mean sleep latency of less than 8 minutes is highly suggestive of narcolepsy, and less than 10 minutes is generally considered clinically significant for EDS. A key advantage of the MSLT is its resistance to patient exaggeration, making it useful in situations where secondary gain or substance abuse is a concern.
4. Maintenance of Wakefulness Test (MWT): The MWT assesses the ability to stay awake in a sleep-promoting environment. Similar to the MSLT, it involves multiple trials (4-5) throughout the day, spaced two hours apart. However, in the MWT, patients are instructed to resist falling asleep for a set period (typically 20-40 minutes). The MWT is considered to have better face validity for assessing safety-critical situations, such as driving. While not specifically validated for driving safety, the ability to remain awake on the MWT is often used as a clinical marker of alertness. It’s important to note that the MWT can be influenced by motivational factors.
5. Other Tests: Research settings have utilized other tests, such as the psychomotor vigilance task (PVT), which is sensitive to sleep loss and circadian rhythm variations. Driving simulators have also been explored but are not widely available clinically. New and more practical measurement tools for clinical use are continuously under development.
Management and Treatment Strategies
Treatment for EDS is tailored to the underlying cause and severity of the condition.
1. Optimizing Sleep Hygiene: Ensuring adequate sleep duration and quality is the cornerstone of EDS management. This involves establishing a regular sleep schedule, creating a conducive sleep environment, and practicing good sleep hygiene habits. Strategic napping may also be beneficial for some individuals.
2. Treating Underlying Sleep Disorders: Addressing primary sleep disorders, such as obstructive sleep apnea with continuous positive airway pressure (CPAP) therapy, is essential. Treating UARS and other contributing sleep disorders is also crucial for resolving EDS.
3. Lifestyle Modifications: Simple lifestyle changes can significantly improve alertness. Standing up and moving around, exposure to bright light (especially in the evening for shift workers), and avoiding sedative substances, including alcohol and unnecessary sedating medications, can be helpful.
4. Caffeine: Caffeine is a commonly used stimulant to combat sleepiness. However, it should be used judiciously and avoided in the late afternoon or evening to prevent sleep disruption.
5. Medications: When lifestyle measures and treatment of underlying conditions are insufficient, pharmacological interventions may be necessary.
* **Modafinil:** Modafinil is a wake-promoting medication often used as an adjunct to CPAP therapy in patients with residual EDS after sleep apnea treatment. It is generally well-tolerated, with minimal side effects and low abuse potential.
* **Stimulants:** Stimulant medications, such as methylphenidate and amphetamine-like drugs, are used, particularly in narcolepsy and other conditions with severe EDS. These medications require careful prescribing due to their potential for abuse, psychiatric side effects, and cardiovascular risks.
* **Sodium Oxybate:** Sodium oxybate is primarily used for treating cataplexy in narcolepsy but can also improve EDS in these patients.
* **Alerting Antidepressants:** Certain antidepressants, like fluoxetine when taken in the morning, can have alerting effects and may be preferred over sedating antidepressants in patients with EDS and depression.
* **Chronotherapeutics:** Adjusting the timing of medication administration can minimize sedative effects and maximize alertness. Avoiding sleeping pills, which can have "hangover" effects and worsen daytime sleepiness, is generally recommended.Driving Safety and EDS
Driving safety is a paramount concern for individuals with EDS, especially for automotive professionals who spend considerable time on the road or in safety-sensitive work environments. Untreated sleep apnea and insufficient sleep are known to significantly increase the risk of traffic accidents, comparable to driving under the influence of alcohol.
Addressing driving safety should be a priority in the initial consultation for EDS. Clinicians should assess for a history of accidents and untreated sleep disorders. Educating patients about the risks of driving while sleepy and advising them to avoid driving when feeling drowsy is critical. In cases of doubt about a patient’s driving safety, objective testing, such as the MWT, may be warranted. Furthermore, clinicians must be aware of and comply with local regulations regarding reporting sleep disorders to transportation authorities.
Future Directions in EDS Diagnosis and Management
The field of EDS diagnosis and treatment is continually evolving. There is a growing need for more practical, user-friendly, and real-time measurement tools for clinical management. Portable devices and wearable technologies are being developed to better assess alertness and impairment in everyday settings. While current neurophysiological tests like MSLT and MWT are not directly validated for driving safety, they provide valuable insights into sleepiness levels.
Ongoing research into the neurobiology of sleep-wake regulation is leading to the development of new medications targeting specific neurotransmitter systems, such as orexin/hypocretin, histamine, and melatonin. These targeted therapies hold promise for more effective and personalized treatment of EDS with fewer side effects in the future.
Conclusion
Daytime sleepiness is a common and significant health concern that can have far-reaching consequences, particularly for professionals in demanding and safety-critical industries like automotive services. A thorough diagnostic approach, including a detailed history, physical examination, and objective sleepiness measures when appropriate, is crucial for identifying the underlying causes of EDS. Effective management strategies, ranging from lifestyle modifications and treatment of underlying sleep disorders to pharmacological interventions, are available to improve alertness, enhance quality of life, and prevent safety risks. Continued advancements in diagnostic tools and therapeutic options offer hope for even better management of daytime sleepiness in the future.
