Major Depressive Disorder (MDD) stands as a significant global health concern, recognized by the World Health Organization (WHO) as a leading cause of disability worldwide. Projected to be the top cause of disease burden by 2030, MDD is characterized by persistent low mood, loss of interest in pleasurable activities (anhedonia), feelings of worthlessness or guilt, fatigue, concentration difficulties, changes in appetite, psychomotor disturbances, sleep problems, and suicidal thoughts. Accurate diagnosis is crucial, and this article will delve into the differential diagnosis of depressive disorders, ensuring clinicians can effectively distinguish MDD from other conditions with overlapping symptoms.
Understanding Major Depressive Disorder
To properly understand the differential diagnosis, it’s essential to first have a clear understanding of MDD itself. According to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), a diagnosis of MDD requires the presence of at least five of the aforementioned symptoms for a minimum of two weeks, with either depressed mood or anhedonia being one of the symptoms. These symptoms must also cause significant social or occupational impairment. Importantly, to diagnose MDD, any history of manic or hypomanic episodes must be excluded. In children and adolescents, irritability may be a prominent mood symptom instead of depressed mood.
Beyond MDD, the DSM-5 categorizes other depressive disorders including:
- Persistent Depressive Disorder (Dysthymia)
- Disruptive Mood Dysregulation Disorder
- Premenstrual Dysphoric Disorder
- Substance/Medication-Induced Depressive Disorder
- Depressive Disorder Due to Another Medical Condition
- Unspecified Depressive Disorder
Understanding these related disorders is the first step in differential diagnosis.
Etiology and Overlapping Symptomatology
The etiology of MDD is complex and multifactorial, involving biological, genetic, environmental, and psychosocial influences. Initially, neurotransmitter imbalances, particularly serotonin, norepinephrine, and dopamine, were heavily emphasized. This is supported by the effectiveness of antidepressants targeting these systems, such as Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs). However, current understanding points towards more intricate neuroregulatory systems and neural circuits as primary factors, with neurotransmitter imbalances being secondary effects.
Other neurotransmitters like GABA (inhibitory) and glutamate and glycine (excitatory) are also implicated in depression. Lower GABA levels have been observed in depressed patients. Furthermore, hormonal abnormalities, especially thyroid and growth hormones, and the impact of adverse childhood experiences and trauma are significant contributing factors. Early life stress can lead to neuroendocrine and behavioral changes, potentially causing structural changes in the brain and increasing vulnerability to depression later in life. Brain imaging studies have revealed structural and functional abnormalities in depressed individuals. Genetic predisposition also plays a role, as indicated by twin and family studies. Life events, personality traits, and cognitive distortions further contribute to the risk and manifestation of depression.
This complex etiology means that depressive symptoms can arise from a wide range of underlying issues, necessitating a thorough differential diagnosis to rule out conditions that mimic or contribute to depressive presentations.
The Importance of Differential Diagnosis
Accurate differential diagnosis is paramount in managing depressive disorders. Misdiagnosis can lead to ineffective treatment, delayed recovery, and potentially adverse outcomes. For instance, mistaking bipolar disorder for MDD and treating it solely with antidepressants can precipitate manic episodes. Similarly, overlooking an underlying medical condition causing depressive symptoms will prevent effective treatment of the root cause. Therefore, a systematic approach to differential diagnosis is crucial for all clinicians.
Conditions to Differentiate from Major Depressive Disorder
The differential diagnosis of MDD is broad and requires careful consideration of various psychiatric and medical conditions. Key categories to consider include:
1. Bipolar Disorder and Cyclothymia
Bipolar disorder, particularly bipolar II disorder, can be frequently misdiagnosed as MDD. Bipolar II disorder is characterized by episodes of major depression and hypomania. Hypomanic episodes, being less severe than full mania, can be missed by both patients and clinicians, especially if the focus is primarily on depressive symptoms. Key differentiators include:
- History of Mania or Hypomania: Careful questioning about periods of elevated mood, increased energy, decreased need for sleep, racing thoughts, impulsivity, and grandiosity is crucial. Collateral information from family members can be invaluable.
- Course of Illness: Bipolar disorder typically has a more episodic course with distinct mood swings, while MDD, although recurrent, lacks the clear manic/hypomanic episodes.
- Family History: A family history of bipolar disorder increases the likelihood of bipolar spectrum illness.
- Treatment Response: Antidepressants alone can sometimes worsen bipolar disorder or induce rapid cycling. Mood stabilizers are the cornerstone of treatment for bipolar disorders.
Cyclothymia is a milder, chronic form of bipolar disorder characterized by fluctuating mood disturbances involving numerous periods of hypomanic and depressive symptoms that do not meet the full criteria for hypomania or major depression. Differentiating cyclothymia from MDD is important as the treatment approaches differ.
2. Persistent Depressive Disorder (Dysthymia)
Persistent depressive disorder, or dysthymia, involves chronic low-grade depressive symptoms that persist for at least two years in adults (one year in children and adolescents). While the symptoms are less severe than in MDD, they are persistent and cause significant distress or impairment. Distinguishing features include:
- Chronicity: Dysthymia is defined by its long duration, whereas MDD can be episodic.
- Severity of Symptoms: MDD episodes are typically more severe and disabling than dysthymia.
- “Double Depression”: Individuals with dysthymia can also experience episodes of MDD, known as “double depression.” It is important to recognize both conditions if present.
3. Adjustment Disorder with Depressed Mood
Adjustment disorder with depressed mood is a reaction to an identifiable stressor occurring within three months of the stressor’s onset. Symptoms are clinically significant as evidenced by marked distress that is out of proportion to the severity or intensity of the stressor, or significant impairment in social, occupational, or other important areas of functioning. However, once the stressor or its consequences have terminated, the symptoms do not persist for more than an additional six months. Key differentiators are:
- Identifiable Stressor: The onset of symptoms is directly linked to a specific stressor.
- Timeframe: Symptoms resolve within six months of the stressor being removed.
- Less Severe Criteria: While distressing, the symptom criteria may not fully meet the threshold for MDD.
4. Bereavement
Bereavement, or grief, is a normal reaction to loss. While grief can involve many symptoms overlapping with depression, such as sadness, tearfulness, insomnia, and appetite changes, it is a distinct process. Differentiating features include:
- Context of Loss: Bereavement follows a significant loss, typically the death of a loved one.
- Predominant Emotion: Grief involves a wider range of emotions beyond sadness, including longing, pain of loss, and preoccupation with the deceased. Self-esteem is usually preserved in grief, whereas feelings of worthlessness and guilt are prominent in MDD.
- Course of Grief: Grief typically diminishes in intensity over time, although it can be prolonged in some cases. MDD, in contrast, is a clinical syndrome requiring specific treatment. However, it’s important to note that bereavement can sometimes trigger a major depressive episode, especially in vulnerable individuals.
5. Anxiety Disorders
Anxiety disorders, such as generalized anxiety disorder, panic disorder, social anxiety disorder, and obsessive-compulsive disorder, frequently co-occur with MDD. Furthermore, some symptoms of anxiety and depression overlap, including sleep disturbances, concentration difficulties, and irritability. Differential diagnosis involves:
- Primary Symptom Focus: In anxiety disorders, the primary symptoms are related to excessive worry, fear, and anxiety. In MDD, the core symptoms are depressed mood and anhedonia.
- Specific Anxiety Symptoms: Panic attacks, phobias, compulsions, and excessive worry are more specific to anxiety disorders.
- Comorbidity: It’s crucial to recognize that anxiety disorders and MDD can coexist, requiring treatment for both conditions.
6. Schizophrenia and Schizoaffective Disorder
Schizophrenia and schizoaffective disorder are psychotic disorders that can sometimes present with depressive symptoms. Schizoaffective disorder, in particular, involves a combination of mood episodes (major depression or mania) and psychotic symptoms (hallucinations, delusions). Key differentiators include:
- Psychotic Symptoms: Hallucinations and delusions are prominent in psychotic disorders and are not typically present in MDD (unless with psychotic features).
- Timing of Symptoms: In schizoaffective disorder, psychotic symptoms occur concurrently with mood episodes. In schizophrenia, psychotic symptoms are present even in the absence of prominent mood episodes.
- Thought Disorder: Formal thought disorder, disorganized thinking, and negative symptoms are more characteristic of schizophrenia spectrum disorders.
7. Eating Disorders
Eating disorders, such as anorexia nervosa and bulimia nervosa, often co-occur with depression. Depressive symptoms can be secondary to the physiological and psychological consequences of disordered eating patterns. Differential diagnosis involves:
- Eating Disorder Symptoms: Preoccupation with weight and body image, restrictive eating, binge eating, and purging behaviors are central to eating disorders.
- Medical Complications: Eating disorders can lead to significant medical complications that can also contribute to depressive symptoms.
- Primary Diagnosis: Determine whether the depressive symptoms are secondary to the eating disorder or represent a comorbid MDD.
8. Substance/Medication-Induced Depressive Disorder
Depressive symptoms can be induced by various substances of abuse and certain medications. It’s crucial to consider substance use history and medication review in the differential diagnosis. Causative agents can include:
- Alcohol and Sedatives: While initially potentially mood-lifting, chronic use and withdrawal can induce depression.
- Stimulant Withdrawal: Withdrawal from stimulants like cocaine and amphetamines can lead to significant depressive symptoms.
- Steroids: Corticosteroids and anabolic steroids can cause mood disturbances, including depression.
- Antihypertensives: Certain antihypertensive medications can have depressive side effects.
- Anticonvulsants and Antibiotics: Some medications in these classes have been linked to depressive symptoms.
9. Depressive Disorder Due to Another Medical Condition
Numerous medical conditions can directly or indirectly cause depressive symptoms. It’s essential to rule out underlying medical causes before diagnosing primary MDD. Important medical conditions to consider include:
- Neurological Conditions: Cerebrovascular accidents (stroke), multiple sclerosis, subdural hematoma, epilepsy, Parkinson’s disease, Alzheimer’s disease, and brain tumors.
- Endocrinopathies: Hypothyroidism, hyperthyroidism, Cushing’s syndrome, Addison’s disease, diabetes.
- Metabolic Disturbances: Hypercalcemia, hyponatremia, vitamin deficiencies (Vitamin D, B12, B6, folate), iron deficiency.
- Infectious Diseases: HIV, syphilis, Lyme disease, infectious mononucleosis.
- Malignancies: Pancreatic cancer, brain tumors, paraneoplastic syndromes.
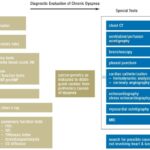
Diagnostic Approach:
Evaluating for medical causes involves:
- Detailed Medical History and Physical Examination: Thorough assessment of past medical history, current symptoms, and physical examination findings.
- Laboratory Investigations: Routine blood work including complete blood count, comprehensive metabolic panel, thyroid function tests (TSH, free T4), vitamin D, vitamin B12, urinalysis, and toxicology screening. Additional tests may be indicated based on clinical suspicion.
- Neuroimaging: Brain imaging (CT or MRI) may be necessary in cases with neurological symptoms or suspected structural brain lesions.
Prognosis and Complications
Untreated MDD episodes can last for 6 to 12 months. A significant concern is suicide risk, with two-thirds of individuals with MDD contemplating suicide and 10-15% completing suicide. MDD is often a chronic, recurrent illness. Recurrence rates are high: approximately 50% after the first episode, 70% after the second, and 90% after the third. A small percentage (5-10%) of patients initially diagnosed with MDD may eventually be diagnosed with bipolar disorder.
Prognosis is generally better for patients with milder episodes, absence of psychotic symptoms, good treatment compliance, strong social support, and good premorbid functioning. Poorer prognosis is associated with comorbid psychiatric disorders, personality disorders, multiple hospitalizations, and older age of onset.
Complications of MDD are significant. It is a leading cause of disability, impairing functioning, interpersonal relationships, and quality of life. Comorbid anxiety and substance use disorders are common and further increase suicide risk. Depression can also worsen medical comorbidities like diabetes, hypertension, COPD, and coronary artery disease. Self-destructive behaviors can emerge as maladaptive coping mechanisms.
Enhancing Healthcare Team Outcomes
Effective management of MDD requires an interdisciplinary approach. Primary care physicians, psychiatrists, nurses, therapists, social workers, and case managers all play vital roles. Depression screening in primary care is crucial, utilizing tools like the Patient Health Questionnaire-9 (PHQ-9). Early diagnosis, psychoeducation, lifestyle modifications (including exercise), and suicide risk assessment are essential components of care. Collaborative care models, involving integrated mental health services within primary care, have demonstrated superior outcomes compared to usual care. Close monitoring, follow-up, and family involvement are critical for ensuring treatment adherence and improving patient safety and outcomes.
Conclusion
The differential diagnosis of depressive disorders, particularly MDD, is a complex but essential clinical skill. By systematically considering psychiatric and medical conditions that can mimic or contribute to depressive symptoms, clinicians can ensure accurate diagnoses and develop effective, targeted treatment plans. This comprehensive approach improves patient outcomes and reduces the significant burden associated with depressive disorders.
Alt text: A pensive man with a furrowed brow, illustrating the internal struggle and emotional burden often associated with depressive disorders.
Alt text: A healthcare professional engaged in a clinical interview with a patient, highlighting the importance of detailed patient history in diagnosing depressive disorders.
References
1.Malhi GS, Mann JJ. Depression. Lancet. 2018 Nov 24;392(10161):2299-2312. [PubMed: 30396512]
2.Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, Gillespie CF, Berg T, Evces M, Newport DJ, Stowe ZN, Heim CM, Nemeroff CB, Schwartz A, Cubells JF, Ressler KJ. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008 Feb;65(2):190-200. [PMC free article: PMC2443704] [PubMed: 18250257]
3.Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010 Feb;67(2):113-23. [PMC free article: PMC2822662] [PubMed: 20124111]
4.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000 Oct;157(10):1552-62. [PubMed: 11007705]
5.Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, Mortensen PB, Eaton WW. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014 May;71(5):573-81. [PubMed: 24806211]
6.Lyness JM, Niculescu A, Tu X, Reynolds CF, Caine ED. The relationship of medical comorbidity and depression in older, primary care patients. Psychosomatics. 2006 Sep-Oct;47(5):435-9. [PubMed: 16959933]
7.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003 Nov;41(11):1284-92. [PubMed: 14583691]
8.Cuijpers P, Dekker J, Hollon SD, Andersson G. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis. J Clin Psychiatry. 2009 Sep;70(9):1219-29. [PubMed: 19818243]
9.Cuijpers P, van Straten A, Warmerdam L, Andersson G. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety. 2009;26(3):279-88. [PubMed: 19031487]
10.Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J ECT. 2004 Mar;20(1):13-20. [PubMed: 15087991]
11.Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, McGorry PD, Scott J, Berk M, Cotton SM. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. 2017 Apr;135(4):273-284. [PubMed: 28097648]
12.Sighinolfi C, Nespeca C, Menchetti M, Levantesi P, Belvederi Murri M, Berardi D. Collaborative care for depression in European countries: a systematic review and meta-analysis. J Psychosom Res. 2014 Oct;77(4):247-63. [PubMed: 25201482]
Disclosure: Navneet Bains declares no relevant financial relationships with ineligible companies.
Disclosure: Sara Abdijadid declares no relevant financial relationships with ineligible companies.