Background
Mood disorders, encompassing conditions like depression and bipolar disorder, represent a significant health concern affecting children and adolescents. Hospitalizations due to mood disorders are notably the most frequent primary diagnosis for hospital admissions among teenagers aged 13 to 17 in general hospitals. This article delves into the characteristics of these hospitalizations within the United States, with a specific focus on the duration of hospital stays, associated costs, and geographical variations. Understanding trends and patterns, particularly concerning diagnoses like Diagnosis 296.90, is crucial for healthcare professionals and policymakers alike.
Methods
This study leverages data from the Kids’ Inpatient Database (KID) to analyze hospitalization rates for the years 2000, 2003, and 2006. Each year of data encompasses over 2 million hospitalizations, reflecting an estimated 6.3 to 6.5 million annual hospital stays within acute care, non-psychiatric hospitals. This extensive dataset provides a robust foundation for examining trends in pediatric mood disorder hospitalizations and the prevalence of specific diagnoses, including diagnosis 296.90, which is categorized within unspecified episodic mood disorders.
Results
The study revealed that the rate of pediatric hospitalizations with a principal diagnosis of a mood disorder was 12.4 per 10,000 children in 2000, 13.0 in 2003, and 12.1 in 2006. Interestingly, during this same period, hospitalizations for depressive disorders saw a decrease from 9.1 to 6.4 per 10,000 children. Conversely, hospitalizations for bipolar disorders increased from 3.3 to 5.7 per 10,000 children. The average length of hospital stay also lengthened, rising from 7.1 to 7.7 days. Furthermore, inflation-adjusted hospital charges escalated from $10,600 in 2000 to $13,700 in 2003, and further to $16,300 in 2006. The proportion of mood disorder-related hospital stays covered by government funding also increased, moving from 35.3% to 45.2%. Geographically, the Western region of the U.S. consistently showed the lowest hospitalization rates (9.9/10,000, 11.6, and 10.2 in 2000, 2003, and 2006), while the Midwest region recorded the highest rates (26.4, 27.6, and 25.4). These regional disparities highlight the complex factors influencing mental health service utilization and diagnosis patterns, including the application of codes like diagnosis 296.90.
Discussion
Mood disorders are a significant cause of hospitalization during childhood and adolescence, particularly in the teenage years. While overall mood disorder hospitalizations remained relatively stable between 2000 and 2006, a notable shift occurred within the subtypes. Diagnoses of depressive disorders decreased, while diagnoses of bipolar disorders increased. This shift in diagnostic patterns could reflect changes in diagnostic practices or a real change in the presentation of mood disorders in young people. The most frequent specific mood disorder diagnosis in 2006 was “unspecified episodic mood disorder” (diagnosis 296.90), accounting for 11.0% of all mood disorder hospitalizations. This highlights the importance of understanding and accurately diagnosing unspecified mood disorders in clinical settings.
The prevalence of diagnosis 296.90, unspecified episodic mood disorder, as the leading specific diagnosis within mood disorder hospitalizations warrants further examination. This category may represent a diagnostic challenge, where clinicians are recognizing mood disturbance but are unable to classify it definitively as bipolar or depressive disorder at the time of hospitalization. The rise in bipolar disorder diagnoses alongside the prominence of diagnosis 296.90 suggests a potential diagnostic trend, or perhaps a broadening of the bipolar spectrum in pediatric populations.
Figure 1: Age-specific rates of pediatric hospitalizations for mood disorders per 10,000 children in 2006, illustrating the increased incidence with age, particularly in adolescence. The graph highlights the significant rise in hospitalizations as children transition into their teenage years, underscoring the critical period for mental health interventions and support.
Regional variations in hospitalization rates for mood disorders are substantial and consistent across the study years. The Midwest consistently shows rates more than double those of the West. These regional disparities are not explained by overall pediatric hospitalization rates, which are highest in the South and lowest in the Midwest. This suggests that regional factors specific to mental health service delivery, diagnostic practices, or cultural perceptions of mental illness may be at play. The lower rates in the West might indicate better access to outpatient mental health services, different thresholds for hospitalization, or variations in the application of diagnostic codes, including diagnosis 296.90, across regions.
The strong association between mood disorders and suicide attempts is a critical finding. Children hospitalized with any mood disorder diagnosis were significantly more likely to have a suicide attempt recorded on their hospital record compared to children without a mood disorder diagnosis. While diagnosis 296.90 itself doesn’t directly indicate suicidal ideation, the broader category of mood disorders clearly places young people at heightened risk. This underscores the need for comprehensive suicide risk assessment and prevention efforts within pediatric mental health care, particularly for those diagnosed with mood disorders, including unspecified types.
The increasing proportion of hospitalizations paid by government sources reflects the growing public health burden of pediatric mood disorders. As government-funded insurance becomes a more significant payer, it highlights the need for efficient and effective allocation of public resources to address mental health needs in young people. The rising hospital charges and length of stay further emphasize the economic impact of these conditions. Understanding the cost drivers associated with mood disorder hospitalizations, including those related to diagnosis 296.90 and related conditions, is essential for developing cost-effective interventions and service delivery models.
Figure 2: Regional hospitalization rates for any mood disorder diagnosis from 2000 to 2006, demonstrating consistent disparities across different regions of the United States. The graph visually represents the significantly higher rates in the Midwest compared to the West, highlighting the need to investigate regional factors influencing mental health service utilization and diagnostic practices.
Table 1. Incidence of hospitalization per 10,000 and 95% Confidence Intervals among children under 18, 2000-2006
| Diagnostic Category | 2000 | 2003 | 2006 |
|---|---|---|---|
| Mood disorders as principal diagnosis | 12.4(12.1-12.7) | 13.0(12.8-13.3) | 12.1(11.9-12.2) |
| Mood disorders as all-listed diagnosis | 18.9(18.5-19.2) | 20.4(20.1-20.6) | 19.6(19.3-19.9) |
| Bipolar disorders as principal diagnosis | 3.3(3.2-3.5) | 4.6(4.4-4.7) | 5.7(5.5-5.8) |
| Depressive disorders as principal diagnosis | 9.1(8.8-9.3) | 8.4(8.3-8.6) | 6.4(5.5-5.8) |
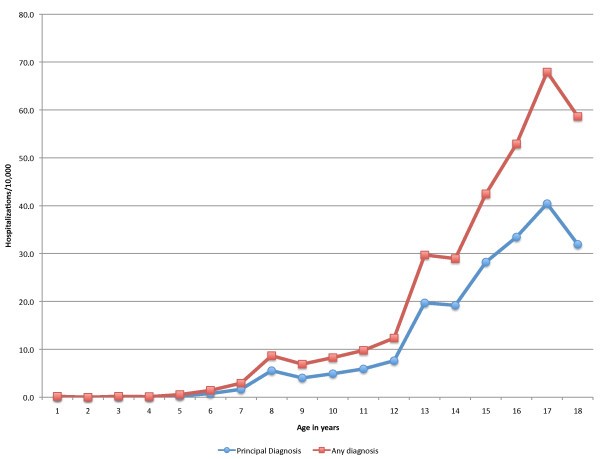
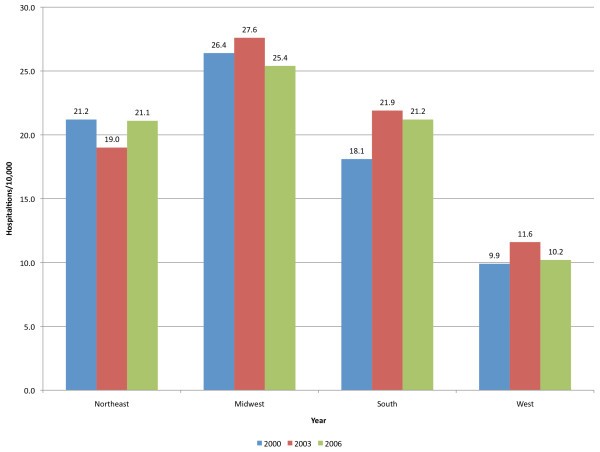
Table 2. The leading ICD-9-CM diagnoses in children hospitalized with a principal diagnosis of mood disorder as a percentage of all hospitalizations with a principal diagnosis of mood disorder, 2006
| Diagnosis (ICD-9-CM code)1 | CCS-MHSASub-category | Percentage of hospitalizations for mood disorders and 95% CI of estimate |
|---|---|---|
| Unspecified episodic mood disorder (296.90) | Bipolar | 11.0 (10.8-11.3) |
| Depressive disorder not elsewhere classified (311) | Depressive | 10.3 (10.1-10.5) |
| Manic-depressive not otherwise specified (296.80) | Bipolar | 8.4 (8.2-8.6) |
| Depressive affective disorders – unspecified (296.2) | Depressive | 6.6 (6.4-6.8) |
| Recurrent depressive disorder – severe (296.33) | Depressive | 5.4 (5.3-5.7) |
| Depressive psychosis -severe (296.23) | Depressive | 4.1 (4.0-4.4) |
| Recurrent depressive disorder – unspecified (296.30) | Depressive | 2.4 (2.3-2.6) |
| Bipolar affective disorder, most recent episode mixed – unspecified (296.60) | Bipolar | 2.3 (2.2-2.6) |
Table 3. Characteristics of hospitalization among children under 18 with any mood disorder diagnosis, 2000-2006¹
| 2000 | 2003 | 2006 | |
|---|---|---|---|
| Primary expected payer | |||
| Medicare or Medicaid | 35.1% | 40.2% | 45.2% |
| Private | 56.5% | 49.7% | 45.3% |
| Other | 8.4% | 9.8% | 9.5% |
| Teaching status of hospital | |||
| Teaching | 51.7% | 58.3% | 62.8% |
| Non-teaching | 48.4% | 41.7% | 37.2% |
| Hospital size | |||
| Small | 9.1% | 10.1% | 10.4% |
| Medium | 24.0% | 22.1% | 21.6% |
| Large | 66.9% | 67.7% | 68.0% |
| Average Length of Stay and 95% Confidence Intervals in days | 7.0(6.9-7.1) | 7.1(7.0-7.2) | 7.6(7.5-7.7) |
| Mean total charges ² | $10,578 | $13,676 | $16,287 |
¹ All differences were statistically significant at 0
² Adjusted for inflation to 2006 dollars
Conclusions
Mood disorders are a major contributor to hospitalizations in children and adolescents, particularly during adolescence. While the overall rate of mood disorder hospitalizations remained relatively stable from 2000 to 2006, the diagnostic landscape shifted, with a decrease in depressive disorder hospitalizations and an increase in bipolar disorder hospitalizations. Diagnosis 296.90, unspecified episodic mood disorder, emerged as the most frequent specific diagnosis within mood disorder hospitalizations, underscoring the complexities of diagnosing mood disorders in young people. Substantial regional variations in hospitalization rates highlight the need to investigate and address factors contributing to these disparities. These findings emphasize the significant burden of mood disorders on child and adolescent health, the increasing demands on public resources, and the crucial need for improved community-based interventions to prevent or effectively treat these conditions, ultimately reducing the necessity for hospitalization. Further research is warranted to explore the reasons behind regional variations, the diagnostic shift between depressive and bipolar disorders, and the specific characteristics of hospitalizations coded as diagnosis 296.90.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors contributed to discussion and interpretation of data analysis, and writing and revisions of the manuscript. TL identified the research question, provided epidemiologic expertise, and led the analysis and manuscript preparation. AK conducted the SAS programming for the data analysis and provided expertise in clinical psychology. AE provided expertise on HCUP KID and data analysis of HCUP KID. BV provided expertise on psychiatry and mental health in children.
Appendix 1
The single level CCS-MHSA category, 657, Mood disorders, and the ICD-9 codes that comprise the multi-level categories, Bipolar disorders, and Depressive disorders.
Bipolar
296.00 MANIC DISORDER-UNSPECIFIED
296.01 MANIC DISORDER-MILD
296.02 MANIC DISORDER-MODERATE
296.03 MANIC DISORDER-SEVERE
296.04 MANIC DISORDER-SEVERE WITH PSYCHOTIC BEHAVIOR
296.05 MANIC DISORDER – PARTIAL REMISSION
296.06 MANIC DISORDER – FULL REMISSION
296.10 RECURRENT MANIC DISORDER-UNSPECIFIED
296.11 RECURRENT MANIC DISORDER-MILD
296.12 RECURRENT MANIC DISORDER-MODERATE
296.13 RECURRENT MANIC DISORDER-SEVERE
296.14 RECURRENT MANIC DISORDER-SEVERE WITH PSYCHOTIC BEHAVIOR
296.15 RECURRENT MANIC DISORDER-PARTIAL REMISSION
296.16 RECURRENT MANIC DISORDER-FULL REMISSION
296.40 BIPOLAR AFFECTIVE DISORDER MANIC-UNSPECIFIED
296.41 BIPOLAR AFFECTIVE DISORDER MANIC-MILD
296.42 BIPOLAR AFFECTIVE DISORDER MANIC-MODERATE
296.43 BIPOLAR AFFECTIVE DISORDER MANIC-SEVERE
296.44 BIPOLAR MANIC-SEVERE WITH PSYCHOTIC BEHAVIOR
296.45 BIPOLAR AFFECTIVE DISORDER MANIC-PART REMISSION
296.46 BIPOLAR AFFECTIVE DISORDER MANIC-FULL REMISSION
296.50 BIPOLAR AFFECTIVE DISORDER DEPRESSED-UNSPECIFIED
296.51 BIPOLAR AFFECTIVE DISORDER DEPRESSED-MILD
296.52 BIPOLAR AFFECTIVE DISORDER DEPRESSED-MODERATE
296.53 BIPOLAR AFFECTIVE DISORDER DEPRESSED-SEVERE
296.54 BIPOLAR DEPRESSED-SEVERE WITH PSYCHOTIC BEHAVIOR
296.55 BIPOLAR AFFECTIVE DEPRESSED-PARTIAL REMISSION
296.56 BIPOLAR AFFECTIVE DEPRESSED-FULL REMISSION
296.60 BIPOLAR AFFECTIVE DISORDER MIXED-UNSPECIFIED
296.61 BIPOLAR AFFECTIVE DISORDER MIXED-MILD
296.62 BIPOLAR AFFECTIVE DISORDER MIXED-MODERATE
296.63 BIPOLAR AFFECTIVE DISORDER MIXED-SEVERE
296.64 BIPOLAR MIXED-SEVERE With PSYCHOTIC BEHAVIOR
296.65 BIPOLAR AFFECTIVE DISORDER MIX-PARTIAL REMISSION
296.66 BIPOLAR AFFECTIVE DISORDER MIX-FULL REMISSION
296.7 BIPOLAR AFFECTIVE NOT OTHERWISE SPECIFIED
296.80 MANIC-DEPRESSIVE NOT OTHERWISE SPECIFIED
296.81 ATYPICAL MANIC DISORDER
296.82 ATYPICAL DEPRESSIVE DISORDER
296.89 MANIC-DEPRESSIVE NOT ELSEWHERE CLASSIFIED
296.90 UNSPECIFIED EPISODIC MOOD DISORDER
296.99 AFFECTIVE PSYCHOSES NOT ELSEWHERE CLASSIFIED
Depressive
293.83 ORGANIC AFFECTIVE SYNDROME
296.20 DEPRESSIVE AFFECTIVE DISORDERS-UNSPECIFIED
296.21 DEPRESSIVE AFFECTIVE DISORDER-MILD
296.22 DEPRESSIVE AFFECTIVE DISORDER-MODERATE
296.23 DEPRESSIVE AFFECTIVE DISORDER-SEVERE WITHOUT PSYCHOTIC BEHAVIOR
296.24 DEPRESSIVE AFFECTIVE DISORDER-SEVERE WITH PSYCHOTIC BEHAVIOR
296.25 DEPRESSIVE AFFECTIVE DISORDER-PARTIAL REMISSION
296.26 DEPRESSIVE AFFECTIVE DISORDER-FULL REMISSION
296.30 RECURRENT DEPRESSIVE DISORDER-UNSPECIFIED
296.31 RECURRENT DEPRESSIVE DISORDER-MILD
296.32 RECURRENT DEPRESSIVE DISORDER-MODERATE
296.33 RECURRENT DEPRESSIVE DISORDER-SEVERE
296.34 RECURRENT DEPRESSIVE DISORDER-SEVERE WITH PSYCHOTIC BEHAVIOR
296.35 RECURRENT DEPRESSIVE DISORDER-PARTIAL REMISSION
296.36 RECURRENT DEPRESSIVE DISORDER-FULL REMISSION
3004 NEUROTIC DEPRESSION
311 DEPRESSIVE DISORDER NOT ELSEWHERE CLASSIFIED
Contributor Information
Tamar Lasky, Email: [email protected].
Aliza Krieger, Email: [email protected].
Anne Elixhauser, Email: [email protected].
Benedetto Vitiello, Email: [email protected].
Acknowledgements
Funds for data analysis by research assistant, Aliza Krieger, were provided by the University of Rhode Island in the summer of 2009.