Cirrhosis is a significant health concern affecting approximately 2.2 million adults in the United States. Alarmingly, mortality rates associated with cirrhosis have been on the rise, increasing from 14.9 per 100,000 in 2010 to 21.9 per 100,000 in 2021. Understanding the diagnosis and management of cirrhosis and its complications is crucial for improving patient outcomes.
Common Causes and Symptoms of Cirrhosis
Several factors contribute to the development of cirrhosis, with overlap frequently observed among them. Alcohol use disorder is a leading cause, implicated in approximately 45% of cirrhosis cases. Nonalcoholic fatty liver disease (NAFLD) accounts for around 26%, and hepatitis C is another significant contributor at 41%. These conditions can independently or synergistically lead to chronic liver damage and cirrhosis.
Patients with cirrhosis often experience a range of debilitating symptoms that significantly impact their quality of life. Muscle cramps are highly prevalent, affecting approximately 64% of individuals. Pruritus, or persistent itching, is reported by 39% of patients. Sleep disturbances are also common, with 63% experiencing poor sleep quality. Furthermore, sexual dysfunction affects a substantial proportion, with 53% of patients reporting issues. Recognizing these symptoms is important for early identification and management.
Diagnosis of Cirrhosis
Diagnosing cirrhosis can be achieved through various methods, ranging from invasive to non-invasive approaches. Liver biopsy remains a definitive diagnostic tool, providing detailed histological information. However, non-invasive techniques have gained prominence. Elastography, a method that assesses liver stiffness, offers a valuable non-invasive alternative. Measurements of 15 kilopascals (kPa) or greater obtained through elastography typically indicate the presence of cirrhosis. The availability of non-invasive diagnostic tools is crucial for timely assessment and monitoring of liver health.
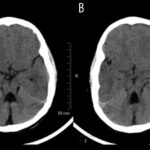
Unfortunately, a significant proportion, approximately 40%, of individuals with cirrhosis are not diagnosed until they present with severe complications. These complications often include hepatic encephalopathy, a condition affecting brain function, and ascites, the accumulation of fluid in the abdomen. The late diagnosis underscores the importance of increased awareness and earlier detection strategies for cirrhosis.
Cirrhosis Complications and Their Management
Cirrhosis is associated with several serious complications that significantly impact prognosis and survival. Hepatic encephalopathy and ascites are particularly concerning. The median survival time following the onset of hepatic encephalopathy is less than a year, at 0.92 years. Similarly, for ascites, the median survival time is also limited to approximately 1.1 years.
Ascites further predisposes patients to other life-threatening conditions. Spontaneous bacterial peritonitis, a serious infection of the ascitic fluid, occurs at an annual incidence of 11% in patients with ascites. Hepatorenal syndrome, kidney dysfunction in the setting of cirrhosis, has an annual incidence of 8% and is associated with a very poor prognosis, with a median survival of less than 2 weeks if untreated.
Hepatocellular carcinoma (HCC), liver cancer, is another significant complication. It develops in approximately 1% to 4% of patients with cirrhosis annually. Despite advancements in cancer treatment, HCC carries a poor prognosis, with a 5-year survival rate of approximately 20%. Regular surveillance for HCC is recommended in patients with cirrhosis.
Management Strategies
Effective management strategies are crucial for improving outcomes in patients with cirrhosis and its complications. For portal hypertension, a common consequence of cirrhosis that can lead to variceal bleeding, nonselective β-blockers like carvedilol or propranolol are first-line therapies. Clinical trials have demonstrated their effectiveness in reducing the risk of decompensation or death.
Ascites management typically involves a combination of aldosterone antagonists and loop diuretics. This combination has been shown to be more effective in resolving ascites compared to sequential initiation of these medications and is associated with lower rates of hyperkalemia.
Lactulose is a cornerstone in the management of hepatic encephalopathy. Meta-analyses have shown that lactulose is associated with reduced mortality and a decreased risk of recurrent overt hepatic encephalopathy.
For hepatorenal syndrome, terlipressin has demonstrated efficacy in improving the rate of reversal. Clinical trials have shown that terlipressin significantly improves kidney function in this setting.
Addressing the distressing symptoms of cirrhosis is also an important aspect of management. Hydroxyzine has shown promise in improving sleep dysfunction. Pickle brine and taurine may help reduce muscle cramps. Tadalafil can be considered for managing sexual dysfunction in men.
Conclusion
Cirrhosis remains a major health challenge in the US, with increasing mortality rates. Early diagnosis and comprehensive management are essential to improve patient outcomes. First-line therapies, including carvedilol or propranolol for preventing variceal bleeding, lactulose for hepatic encephalopathy, combination diuretics for ascites, and terlipressin for hepatorenal syndrome, are critical components of care. Furthermore, addressing symptoms such as muscle cramps, sleep disturbances, pruritus, and sexual dysfunction can significantly enhance the quality of life for individuals living with cirrhosis. Continued research and improved clinical strategies are vital to combat the rising burden of cirrhosis and its complications.