Depression is a prevalent and serious mental health condition frequently encountered in primary care settings. Effective diagnosis and management are crucial for improving patient outcomes. Recent advancements in antidepressant pharmacotherapy have introduced newer agents with improved side effect profiles, offering primary care physicians more options for treating depression. This article outlines these newer antidepressant agents, focusing on their role in the diagnosis and management of depression within primary care.
Selective serotonin reuptake inhibitors (SSRIs) have become a cornerstone in the pharmacological treatment of depression. This class includes citalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline, each approved for treating depression and other related conditions. Citalopram is specifically indicated for depression, while fluvoxamine is used for obsessive-compulsive disorder. Fluoxetine’s applications extend to depression, obsessive-compulsive disorder, and bulimia nervosa. Paroxetine is effective in treating depression, obsessive-compulsive disorder, panic disorder, and social anxiety disorder. Sertraline is indicated for depression, obsessive-compulsive disorder, panic disorder (with or without agoraphobia), and posttraumatic stress disorder. In primary care, SSRIs are often considered first-line due to their tolerability and ease of use compared to older antidepressants.
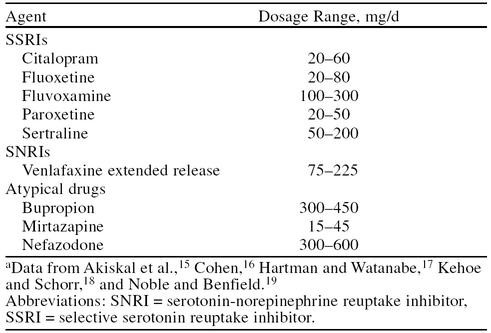 Table 5. Commonly Used Newer Antidepressant Agents with Drug Names, Doses, and Side Effects
Table 5. Commonly Used Newer Antidepressant Agents with Drug Names, Doses, and Side Effects
SSRIs are generally better tolerated than tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs). They lack cardiac liabilities, are less sedating, and are not typically associated with weight gain. Common side effects, though usually manageable, include nausea, headache, lack of coordination, sleep disturbance, sexual dysfunction, and tremor. Nausea, a common initial side effect, often subsides with continued treatment and can be mitigated by dose reduction or taking medication with food.
A significant advantage of SSRIs for primary care management is their once-daily dosing, simplifying medication adherence for patients. However, it’s important to note that SSRIs can have a delayed onset of action, sometimes taking up to 5 weeks to achieve therapeutic effects. The choice of SSRI in primary care often depends on individual patient profiles, considering differences in half-life and potential for drug-drug interactions. Most drug interactions with SSRIs arise from their inhibition of cytochrome P450 enzymes. This enzyme inhibition can interfere with the metabolism of other medications, potentially increasing the risk of adverse reactions. Therefore, careful monitoring is essential for patients in primary care who are taking multiple medications concurrently with SSRIs.
Venlafaxine extended release (XR) presents another valuable option in primary care for managing depression, particularly when anxiety is also present. Venlafaxine XR uniquely inhibits the reuptake of both serotonin and norepinephrine, with a weak dopamine reuptake inhibition. This dual action suggests it can be particularly effective for patients experiencing both anxiety and depression, a common comorbidity in primary care. Venlafaxine XR is indeed indicated for both major depressive disorder and generalized anxiety disorder (GAD). Its mechanism of action, involving the imipramine receptor, leads to antidepressant effects comparable to TCAs, but with a more favorable side effect profile as it does not significantly interact with cholinergic, histaminergic, or α-adrenergic receptors, nor does it inhibit MAO. Common side effects of venlafaxine XR include nausea, nervousness, dry mouth, constipation, fatigue, anorexia, somnolence, insomnia, dizziness, abnormal ejaculation, and headache. Importantly, most side effects are mild to moderate, tend to occur early in treatment, and often resolve with continued therapy. Starting at a lower dose and gradually increasing it can minimize nausea, the most frequently reported side effect.
Clinical studies have demonstrated that venlafaxine can show effectiveness as early as the first week of treatment. Furthermore, a positive dose-response relationship exists, meaning that increasing the dosage can improve response and remission rates. Venlafaxine also has a low protein-binding capacity and limited cytochrome P450 enzyme inhibition, reducing the likelihood of drug-drug interactions, an important consideration in managing patients with polypharmacy in primary care. When comparing cytochrome P450 inhibition potency among common antidepressants, venlafaxine exhibits a lower inhibitory potential than paroxetine, fluoxetine, sertraline, fluvoxamine, and clomipramine.
Meta-analysis data comparing venlafaxine XR to SSRIs in depression treatment have shown that venlafaxine XR can achieve significantly higher remission rates (absence of symptoms) after 8 weeks (45% vs. 35%). In direct comparisons with fluoxetine in outpatient settings, venlafaxine XR resulted in full remission (HAM-D score ≤ 7) in 37% of patients at 8 weeks, compared to 22% with fluoxetine. Both medications were generally well-tolerated, with nausea and dizziness being the most common adverse events for venlafaxine, and nausea and diarrhea for fluoxetine.
Nefazodone, an analog of trazodone, acts as an antagonist of postsynaptic serotonin receptors and presynaptic serotonergic reuptake proteins. Its efficacy in treating depression is comparable to imipramine. However, nefazodone has a short half-life, necessitating twice-daily dosing, which can be a limitation in primary care settings focused on simplified regimens. Nefazodone inhibits cytochrome P450 3A4 (CYP3A4), leading to significant interactions, particularly increased sedation and cognitive impairment when combined with alprazolam, triazolam, or midazolam. Contraindications also include concurrent use with terfenadine or cisapride due to the risk of fatal ventricular arrhythmias from QT prolongation caused by CYP3A4 inhibition. Common side effects include somnolence, dry mouth, nausea, and dizziness. Due to drug interaction profiles and the need for twice-daily dosing, nefazodone is less frequently used as a first-line agent in primary care compared to SSRIs or venlafaxine.
Bupropion is believed to exert its antidepressant effects through norepinephrine reuptake inhibition. It is an effective antidepressant, but its initial use in primary care was limited by the risk of seizures at higher doses. The development of a sustained-release formulation of bupropion has improved tolerability and reduced seizure risk, making it a more viable option. Bupropion, sometimes in combination with an SSRI, is used in primary care to manage treatment-resistant depression and SSRI-induced sexual dysfunction. Common side effects of bupropion include agitation, anxiety, insomnia, dry mouth, nausea, constipation, and tremor.
Mirtazapine is an antagonist of presynaptic α2-adrenoceptors and postsynaptic serotonin-2 and -3 receptors. Studies have shown mirtazapine to be more effective than trazodone and as effective as amitriptyline in treating moderate to severe depression. Its sedative effects are similar to amitriptyline, but weight gain is more frequently reported. Mirtazapine is metabolized by multiple cytochrome P450 enzymes, posing a risk for drug-drug interactions. Mirtazapine’s sedative properties can be beneficial for patients with insomnia alongside depression, a common presentation in primary care.
In conclusion, newer antidepressant agents like SSRIs, venlafaxine XR, bupropion, and mirtazapine offer valuable tools for the Diagnosis And Management Of Depression In Primary Care. SSRIs remain first-line for many, while venlafaxine XR is particularly useful for comorbid anxiety and depression. Bupropion and mirtazapine offer alternative mechanisms and side effect profiles that may be beneficial in specific patient populations or for treatment augmentation strategies within primary care. Primary care physicians must carefully consider individual patient factors, potential drug interactions, and side effect profiles when selecting an antidepressant to optimize treatment outcomes and improve the management of depression in their practice.