INTRODUCTION
Gastroesophageal reflux (GER) and gastroesophageal reflux disease (GERD) are common challenges encountered in infants, and these conditions present unique complexities in the preterm population. While guidelines for GER and GERD in infants and children have been established by joint committees such as the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN), the application of these guidelines to preterm infants requires careful consideration and nuanced understanding. This article aims to provide an updated and practical approach to the diagnosis and management of GER and GERD specifically in preterm infants, drawing upon existing guidelines and relevant literature to standardize and improve the quality of care for this vulnerable population.
DEFINITION OF GER AND GERD IN PRETERM INFANTS
Gastroesophageal reflux (GER) is defined as the passage of gastric contents into the esophagus. This physiological process becomes gastroesophageal reflux disease (GERD) when it leads to troublesome symptoms or complications. In preterm infants, the distinction between physiological GER and pathological GERD can be particularly challenging due to their unique physiology and vulnerability. GERD in preterm infants can manifest with a spectrum of symptoms, ranging from mild to severe, impacting their overall well-being and potentially leading to significant complications. It is crucial to recognize that defining “troublesome” symptoms in preterm infants can be subjective and requires careful assessment by healthcare professionals, taking into account the infant’s gestational age, postnatal age, and clinical context.
Table 1. Symptoms and Signs Associated with GERD in Preterm Infants
| Symptoms | Signs |
|---|---|
| Regurgitation/vomiting | Esophageal mucosal complications (esophagitis, esophageal stricture, Barrett’s esophagus) |
| Feeding refusal or aversion | Recurrent/chronic desaturations or apnea |
| Irritability and inconsolable crying | Recurrent aspiration pneumonia |
| Hematemesis or guaiac-positive stools | Laryngitis or chronic cough |
| Poor weight gain or failure to thrive | Recurrent otitis media |
| Arching or back arching (Sandifer syndrome) | Abnormal posturing |
| Disturbed sleep | Dental erosions |
| Apnea, bradycardia, or ALTE/BRUE | – |
| Wheezing or respiratory distress | – |
GERD: gastro-esophageal reflux disease, ALTE: apparent life-threatening event, BRUE: brief resolved unexplained event.
It is important to note that many of these symptoms and signs are non-specific and can be associated with other conditions common in preterm infants, such as infections, necrotizing enterocolitis, and respiratory distress syndrome. Therefore, a thorough differential diagnosis is essential. The subjective interpretation of symptoms, parental anxiety, and the absence of a definitive gold standard diagnostic tool further complicate the diagnosis of GERD in preterm infants. Refractory GERD in preterm infants is defined as GERD that does not respond adequately to optimal treatment after a reasonable period, typically 2 to 4 weeks, requiring further investigation and management strategies.
SYMPTOMS AND SIGNS OF GERD IN PRETERM INFANTS
Preterm infants are particularly susceptible to GERD due to several factors, including:
- Immature Lower Esophageal Sphincter (LES): The LES, which prevents reflux of gastric contents into the esophagus, is often underdeveloped in preterm infants, leading to increased transient LES relaxations and reflux episodes.
- Delayed Gastric Emptying: Gastric emptying may be slower in preterm infants, increasing the volume of gastric contents available for reflux.
- Horizontal Body Position: Preterm infants, especially those in neonatal intensive care units (NICUs), are often nursed in a supine or horizontal position, which can facilitate reflux.
- Feeding Practices: Frequent and bolus feedings, common in preterm infants, can increase gastric volume and pressure, contributing to reflux.
- Underlying Medical Conditions: Preterm infants are more likely to have underlying medical conditions, such as chronic lung disease, bronchopulmonary dysplasia (BPD), and neurological impairment, which can increase the risk and severity of GERD.
The symptoms and signs of GERD in preterm infants can be categorized as esophageal and extra-esophageal manifestations. Esophageal symptoms include regurgitation, vomiting, irritability, feeding refusal, and esophagitis. Extra-esophageal symptoms can be more varied and may include respiratory symptoms such as chronic cough, wheezing, recurrent pneumonia, apnea, bradycardia, and apparent life-threatening events (ALTEs) or brief resolved unexplained events (BRUEs). Table 1 provides a comprehensive list of symptoms and signs associated with GERD in preterm infants.
It is crucial to differentiate GERD symptoms from “red flag” symptoms and signs that may indicate other serious underlying conditions requiring prompt investigation and management (Table 2).
Table 2. ‘Red Flag’ Symptoms and Signs in Preterm Infants Suggesting Disorders Other Than GERD
| Symptoms | Signs |
|---|---|
| Bilious vomiting | Abdominal distension |
| Projectile vomiting | Fever or hypothermia |
| Hematemesis (significant) or melena | Lethargy or decreased responsiveness |
| Onset of regurgitation after 2 weeks of age | Bulging fontanelle or increased head circumference |
| Failure to thrive or weight loss (significant) | Seizures |
| Chronic or bloody diarrhea | Abnormal muscle tone (hypotonia or hypertonia) |
| Apnea or bradycardia requiring resuscitation | Abnormal neurological examination |
GERD: gastro-esophageal reflux disease.
The presence of red flag symptoms necessitates a thorough evaluation to rule out other diagnoses such as pyloric stenosis, intestinal obstruction, infections, metabolic disorders, and neurological conditions.
DIAGNOSTIC INVESTIGATIONS FOR GERD IN PRETERM INFANTS
The diagnostic approach to GERD in preterm infants should be tailored to the individual infant’s clinical presentation and risk factors. In many cases, a detailed history and physical examination, along with a careful assessment of feeding practices and potential contributing factors, may be sufficient to initiate empiric management. However, in cases with persistent or severe symptoms, alarm features, or diagnostic uncertainty, further investigations may be warranted.
Non-Invasive Investigations
- Upper Gastrointestinal (UGI) Series with Barium Contrast: While UGI series is not recommended for routine diagnosis of GERD, it can be helpful to rule out anatomical abnormalities such as malrotation, hiatal hernia, or pyloric stenosis, particularly in preterm infants presenting with bilious vomiting or feeding difficulties.
- Esophageal Ultrasound: Ultrasound may detect reflux episodes, but its sensitivity and specificity for GERD diagnosis are limited, and it is highly operator-dependent. It is not routinely recommended for GERD diagnosis in preterm infants.
- Gastric Scintigraphy (Milk Scan): Gastric scintigraphy can assess gastric emptying and detect pulmonary aspiration. While it can demonstrate reflux of tracer into the esophagus, its sensitivity and specificity for GERD are moderate, and it is not routinely used for GERD diagnosis in preterm infants.
Invasive Investigations
- Esophagogastroduodenoscopy (EGD) with Biopsies: EGD is not routinely indicated for GERD diagnosis in preterm infants. However, it may be considered in cases with alarm symptoms such as hematemesis, dysphagia, or failure to thrive, to evaluate for esophagitis, strictures, Barrett’s esophagus, or to rule out other conditions like eosinophilic esophagitis. Histological findings of esophagitis are not always specific for GERD and may be absent even in the presence of significant reflux.
- Esophageal pH Monitoring: Continuous esophageal pH monitoring measures esophageal acid exposure and was historically considered a key diagnostic tool. However, its role in preterm infants is limited due to challenges in interpretation and correlation with symptoms. Wireless pH monitoring may be an alternative, but impedance cannot be assessed.
- Multichannel Intraluminal Impedance (MII) with pH Monitoring (MII-pH): MII-pH is the most advanced technique to evaluate GER, allowing detection of both acid and non-acid reflux episodes and their temporal relationship with symptoms. It can be useful in preterm infants with persistent symptoms despite empiric therapy, to differentiate between GERD, reflux hypersensitivity, and functional heartburn. However, MII-pH is technically complex, requires expertise in interpretation, and normative data for preterm infants are limited.
Biomarkers and PPI Trials
- Biomarkers (e.g., Salivary Pepsin): Biomarkers like salivary pepsin have not been shown to be reliable for GERD diagnosis in infants, including preterm infants, and are not recommended for routine use.
- Proton Pump Inhibitor (PPI) Diagnostic Trial: PPI trials are not recommended as a diagnostic test for GERD in infants, including preterm infants, as studies have not demonstrated symptom improvement better than placebo in this age group.
In summary, the diagnosis of GERD in preterm infants relies primarily on clinical assessment. Diagnostic investigations are reserved for selected cases with alarm symptoms, persistent symptoms despite initial management, or when considering specific interventions like anti-reflux surgery. MII-pH is the most comprehensive diagnostic tool but is not routinely needed and should be considered in specialized centers when diagnostic uncertainty remains.
NON-PHARMACOLOGICAL TREATMENT OF GERD IN PRETERM INFANTS
Initial management of GERD in preterm infants should focus on non-pharmacological interventions, as these are often effective and avoid potential medication-related side effects.
-
Positioning: Prone positioning (infant lying on their stomach) has been shown to reduce GER in preterm infants. However, prone positioning is associated with an increased risk of sudden infant death syndrome (SIDS) in term infants and should only be considered in preterm infants in the NICU or under continuous cardiorespiratory monitoring. Supine sleeping is universally recommended to prevent SIDS, and side-lying positions are not recommended. Elevating the head of the crib is also not routinely recommended due to safety concerns.
-
Feeding Modifications:
- Smaller, More Frequent Feedings: Reducing feeding volume and increasing feeding frequency can decrease gastric distension and reflux episodes.
- Thickened Feedings: Thickening formula or breast milk with commercially available thickeners (e.g., rice cereal, modified starches, or gums) can reduce visible regurgitation and vomiting. However, breast milk should not be thickened with cereal due to amylases. Commercially prepared thickened formulas are preferred. The impact of thickened feeds on other GERD symptoms like irritability or respiratory symptoms is less clear.
- Anti-Regurgitation (AR) Formulas: Commercially available AR formulas are thickened and designed to reduce regurgitation in “happy spitters.” Comfort formulas are also available, which are thickened, partially hydrolyzed, and lactose-reduced, targeting infants with regurgitation and distress.
- Extensively Hydrolyzed Formulas: In preterm infants with suspected cow’s milk protein allergy mimicking GERD symptoms, a trial of extensively hydrolyzed formula may be considered.
-
Parental Education and Support: Providing parents with education about GER and GERD, reassurance about the benign nature of physiological reflux, and practical strategies for managing symptoms can reduce parental anxiety and improve adherence to management plans.
-
Probiotics: Lactobacillus reuteri DSM 17938 has shown some promise in reducing regurgitation episodes in infants and may be considered as an adjunct therapy.
Lifestyle modifications like avoiding overfeeding are important. There is insufficient evidence to recommend other complementary therapies routinely.
PHARMACOLOGICAL TREATMENT OF GERD IN PRETERM INFANTS
Pharmacological treatment for GERD in preterm infants should be reserved for infants with persistent troublesome symptoms despite optimal non-pharmacological management, and after careful consideration of potential risks and benefits.
-
Antacids and Alginates: Antacids neutralize gastric acid and alginates form a raft on top of gastric contents, potentially reducing reflux episodes. Alginates may be considered as an adjunct to feed thickeners in breastfed infants or as a trial in infants whose symptoms persist despite conservative measures. Aluminum-containing antacids should be avoided in preterm infants, especially with renal dysfunction.
-
Proton Pump Inhibitors (PPIs): PPIs are potent inhibitors of gastric acid secretion. However, studies have not demonstrated efficacy of PPIs over placebo in reducing GERD symptoms in infants, including preterm infants. Furthermore, PPI use has been associated with potential adverse effects, including increased risk of infections (respiratory and gastrointestinal), necrotizing enterocolitis, and bone health issues, particularly in preterm infants. Therefore, routine PPI use for GERD in preterm infants is not recommended. PPIs may be considered in specific situations, such as documented erosive esophagitis or GERD-related complications refractory to other treatments, and should be prescribed by a specialist with careful monitoring for potential adverse effects.
-
Histamine-2 Receptor Antagonists (H2RAs): H2RAs reduce gastric acid secretion but are less potent than PPIs. Their efficacy in preterm infants with GERD is limited, and tachyphylaxis (reduced effectiveness with continued use) can occur. H2RAs are generally not preferred over non-pharmacological measures and are less effective than PPIs when acid suppression is indicated.
-
Prokinetics: Prokinetic agents aim to improve gastric emptying and esophageal motility. Metoclopramide and domperidone are prokinetics that have been used for GERD, but evidence for their efficacy in preterm infants is lacking, and they carry significant risks of side effects, including extrapyramidal symptoms and QT prolongation. Cisapride is associated with sudden death and is contraindicated. Baclofen may reduce transient LES relaxations but has significant side effects and is not a first-line agent. Prokinetics are generally not recommended for routine GERD management in preterm infants.
Pharmacological therapy, particularly with PPIs, should be carefully considered and individualized for preterm infants with severe GERD symptoms or complications, weighing potential benefits against risks. Non-pharmacological measures should remain the cornerstone of initial management.
SURGICAL TREATMENT OF GERD IN PRETERM INFANTS
Anti-reflux surgery, such as Nissen fundoplication, is rarely indicated in preterm infants with GERD. It may be considered in exceptional cases of severe, refractory GERD with life-threatening complications (e.g., recurrent severe aspiration pneumonia, ALTEs) that have failed maximal medical and non-medical therapy. Surgical intervention should be performed in specialized centers with expertise in neonatal surgery and only after thorough evaluation and multidisciplinary consultation. Total esophagogastric disconnection is not routinely recommended. Endoscopic treatments for GERD are not currently established for preterm infants due to equipment size limitations and lack of evidence.
PRACTICAL APPROACH TO GERD IN PRETERM INFANTS
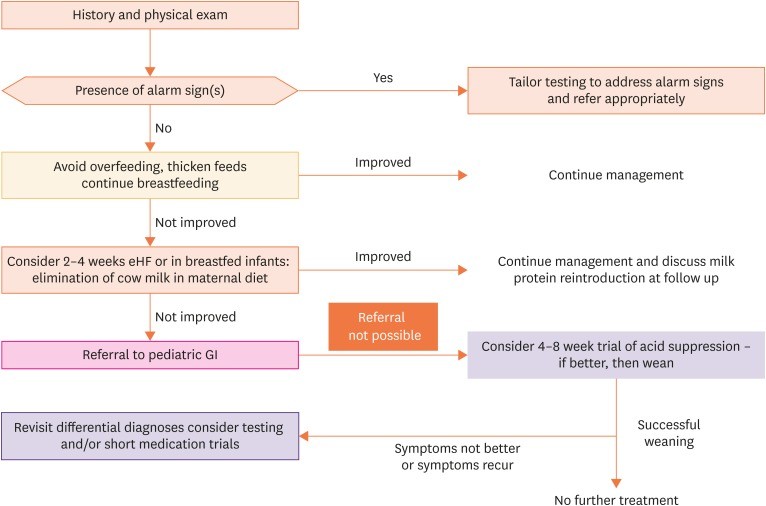
The practical approach to GERD in preterm infants involves a stepwise strategy, starting with thorough clinical assessment and non-pharmacological interventions (Figure 1).
Fig. 1. Practical Algorithm for Diagnosis and Management of Suspected GERD in Preterm Infants
GERD: gastro-esophageal reflux disease, GI: gastrointestinal.
Step 1: Clinical Assessment and History: Obtain a detailed history, including gestational age, postnatal age, feeding history, symptom characteristics, and presence of alarm symptoms. Perform a thorough physical examination to rule out other conditions.
Step 2: Non-Pharmacological Management: Initiate non-pharmacological measures as first-line therapy, including prone positioning (when monitored), smaller, more frequent thickened feedings, AR formula or extensively hydrolyzed formula trial if indicated, and parental education and support.
Step 3: Reassessment: Evaluate response to non-pharmacological measures after 1-2 weeks. If symptoms improve, continue non-pharmacological management.
Step 4: Further Investigation (Selective): If symptoms persist or worsen despite non-pharmacological measures, or if alarm symptoms are present, consider referral to a pediatric gastroenterologist and selective diagnostic investigations, such as MII-pH or EGD, based on clinical presentation and suspicion of complications.
Step 5: Pharmacological Management (Selective and Specialist-Guided): Pharmacological therapy may be considered in consultation with a pediatric gastroenterologist for infants with persistent troublesome symptoms or complications despite optimal non-pharmacological management. PPIs should be reserved for specific indications and used cautiously with monitoring for adverse effects.
Step 6: Surgical Management (Rare and Highly Selective): Anti-reflux surgery is rarely indicated and should be reserved for exceptional cases of severe, refractory GERD with life-threatening complications, after multidisciplinary consultation.
PROGNOSIS OF GERD IN PRETERM INFANTS
The prognosis of GERD in preterm infants is generally favorable. Physiological GER often improves with maturation of the LES and gastrointestinal tract, typically resolving by 12-18 months of age. However, preterm infants with GERD, especially those with underlying comorbidities like BPD or neurological impairment, may have a more prolonged course and increased risk of complications. Factors associated with potentially less favorable outcomes include early onset of GERD symptoms, presence of esophagitis, and need for acid-suppression therapy. Long-term follow-up is important to monitor for symptom resolution, growth, and potential complications.
Table 4. Factors Potentially Related to Persistence of GERD in Infants (Limited Data)
| Prognostic factor | Determinant | Results (Limited Evidence) |
|---|---|---|
| Age of onset GERD | Early onset (< 5 months) | Increased risk of persistence |
| Initial diagnosis severity | GERD with esophagitis | Increased risk of persistence |
| Treatment at diagnosis | No or only antacids | Lower risk of persistence (may reflect milder disease) |
| – | PPI or H2RAs+PPI | Increased risk of persistence (may reflect more severe disease) |
GERD: gastro-esophageal reflux disease, PPI: proton pump inhibitor, H2RA: histamine 2 receptor antagonist.
Further research is needed to better define prognostic factors and long-term outcomes of GERD in preterm infants.
CONCLUSION
The diagnosis and management of GERD in preterm infants present unique challenges. A thorough clinical assessment, judicious use of diagnostic investigations, and a stepwise approach starting with non-pharmacological interventions are essential. Pharmacological therapy, particularly PPIs, should be reserved for selected cases with careful consideration of risks and benefits. Anti-reflux surgery is rarely indicated. Management should be individualized, multidisciplinary, and focused on optimizing infant comfort, nutrition, and respiratory health while minimizing potential adverse effects of interventions. Parental education and support are integral to successful management. Continued research is needed to refine diagnostic and therapeutic strategies and improve outcomes for preterm infants with GERD.
Footnotes
Conflict of Interest: The authors declare no conflicts of interest.