Abstract
Background
Movement System Impairment (MSI) syndromes offer a structured diagnostic and treatment approach that is highly relevant to physical therapy and, by extension, to understanding human movement in various contexts, including automotive repair which requires specific physical demands.
Objectives
This masterclass aims to elucidate the fundamental concepts underpinning MSI syndromes and their treatment, providing a robust framework for understanding movement-related dysfunctions. We will also present current research findings that support the application of movement system impairment syndromes.
Results
The core principle of movement system impairment syndromes is that sustained non-optimal postures and repetitive movements in particular directions can contribute significantly to musculoskeletal conditions. The classification system for MSI syndromes, applicable across all body regions, relies on the interpretation of data from standardized alignment and movement tests. Treatment strategies are centered on correcting impaired alignment and movement patterns, alongside addressing the tissue adaptations that arise from these dysfunctional patterns. While the reliability and validity of MSI syndromes have been investigated and partially validated, treatment efficacy, primarily outside of chronic low back pain, requires further robust randomized controlled trials.
Introduction
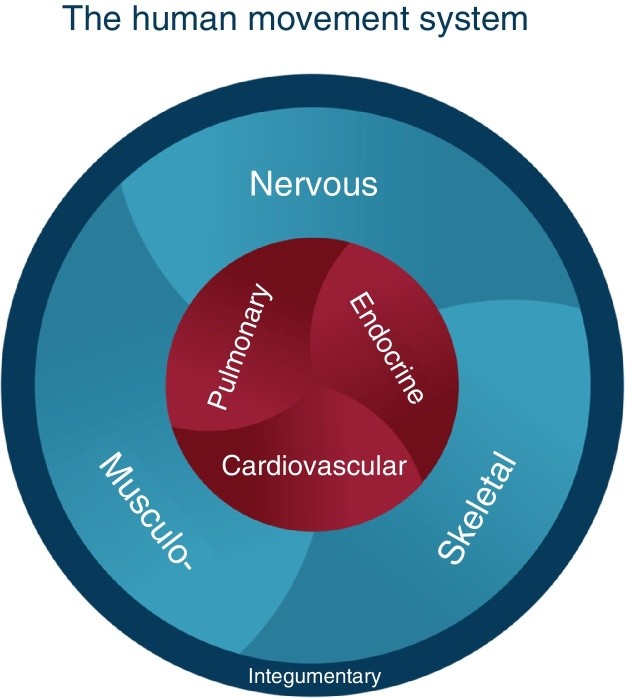
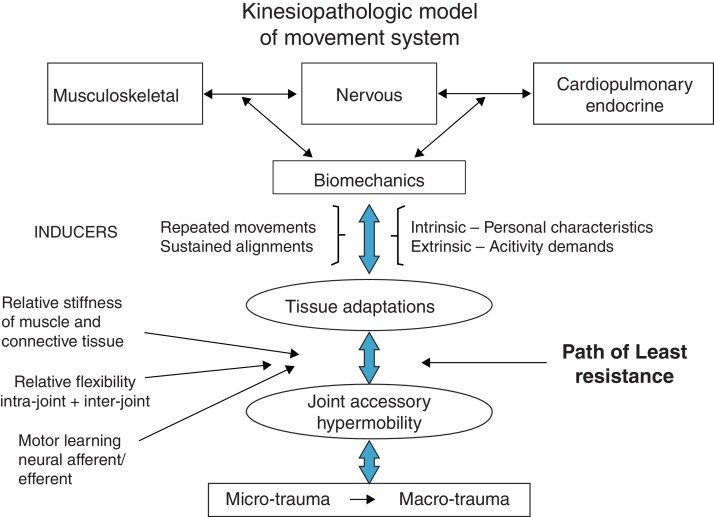
Since 1980, Shirley Sahrmann and her colleagues have pioneered the development of Movement System Impairment (MSI) syndromes. These syndromes serve as a diagnostic framework for physical therapists, guiding treatment strategies and informing prognosis. In 2013, the American Physical Therapy Association formally recognized the “movement system” as the central focus of physical therapy. Washington University defines this system as “a system of physiological organ systems that interact to produce movement of the body and its parts,” as illustrated in Fig. 1. The Kinesiopathologic Model (KPM), depicted in Fig. 2, provides the conceptual foundation for MSI syndromes. A key tenet of the KPM is that both repetitive movements and prolonged static postures can lead to pathological conditions. MSI syndromes are proposed to emerge from the consistent use of suboptimal alignments and movement patterns, which, over time, become dysfunctional and may induce pathoanatomical changes in tissues and joint structures. This model underscores the interconnected roles of: (1) the musculoskeletal system as the effector of movement, (2) the nervous system as the regulator, and (3) the cardiovascular, pulmonary, and endocrine systems as supporting systems that are also influenced by movement. For instance, metabolic syndrome is well-documented as being linked to insufficient physical activity. The prevailing theory, supported by evidence, posits that sustained postures and repetitive movements during daily activities are primary drivers of change across these systems. These changes are further modulated by individual intrinsic factors, such as personal characteristics, and extrinsic factors, including the intensity and nature of physical activity in work and leisure. The fundamental concept is that the body, at the joint level, adheres to physical laws, preferentially adopting the path of least resistance during movement, often in specific directions like flexion, extension, or rotation. This path is determined by: (1) intra- and inter-joint relative flexibility, (2) the relative stiffness of muscles and connective tissues, and (3) motor performance that evolves into motor learning. Consequently, a joint moving more readily in a particular direction can develop hypermobility of accessory motion or micro-instability over time. This micro-instability can lead to tissue microtrauma, which, with repeated stress, can escalate to macrotrauma.
Figure 1.
Figure 2.
The KPM framework suggests that identifiable signs of movement impairment can precede the onset of symptoms. Critically, it also proposes that correcting these impaired alignments and movements, along with addressing contributing factors, represents the most effective approach to treating musculoskeletal pain conditions. The KPM prioritizes addressing the root cause of tissue injury, rather than solely focusing on the pathoanatomy of the affected tissues. Diagnosis within this model begins with identifying impaired alignments and movements through a series of clinical tests. These alignments and movements are typically associated with the provocation or exacerbation of symptoms. Therapists guide patients to correct these alignments and movements to assess whether symptoms improve. Upon completion of the examination, the gathered information is used to: (1) determine the specific MSI syndrome, (2) identify contributing factors, (3) design corrective exercises, (4) define necessary corrections to alignments and movements during daily activities, and (5) educate the patient about factors contributing to their condition by practicing correct movement patterns during activities.
Consider a patient diagnosed with Supraspinatus Tendinopathy, referred for physical therapy. Tendinopathy represents the pathoanatomical diagnosis, indicating the source of pain. However, an MSI-based assessment might reveal insufficient scapular upward rotation coupled with humeral anterior glide. Further examination identifies contributing factors such as relative stiffness, muscle strength imbalances, and neuromuscular activation pattern deficits. The KPM philosophy posits that classifying the patient based on impaired alignments and movements (e.g., Scapular Insufficient Upward Rotation, Humeral Anterior Glide) provides more actionable guidance for physical therapy treatment than merely identifying a pathoanatomical diagnosis. This is because the treatment directly targets the impairments needing correction. Table 1 summarizes the key concepts underpinning the proposed MSI syndromes.
Table 1. Kinesiopathologic model: key concepts.
| Musculoskeletal pain syndromes are the result of cumulative micro-trauma from accumulation of tissue stress and irritation resulting from sustained alignments or repeated movements in a specific direction(s) associated with daily activities. |
|---|
| The joint(s) that is moving too readily in a specific direction is the site of pain generation. |
| The readiness of a joint to move in a specific direction, i.e., the micro-instability, combined with relative stiffness, the neuromuscular activation pattern and motor learning contribute to development and persistence of the path of least resistance. |
| Treatment is based on correcting the impaired alignments and movements contributing to tissue irritation as well as correcting the tissue adaptations, such as relative stiffness, muscle weakness, and neuromuscular activation patterns. |
| Training to correct impaired alignments and movements instead of training “isolated muscles” will induce appropriate neural and musculoskeletal adaptations. |
Relative Intra- and Inter-Joint Flexibility and Relative Stiffness
Relative flexibility and relative stiffness are crucial concepts within the KPM framework for understanding MSI syndromes. Relative flexibility describes the condition of a joint. Intra-joint relative flexibility refers to hypermobility of accessory motions—spin, roll, or glide. When one or more of these motions occurs too readily, it results in an excessive range of motion and increased frequency of motion. Inter-joint relative flexibility describes a scenario where motion occurs more readily at one joint compared to an adjacent joint, even when the movement should ideally be distributed across both. For instance, during forward bending, the lumbar spine might flex more readily than the hips. Stiffness, conversely, is the resistance encountered during passive elongation of muscles and connective tissues. Muscle hypertrophy and collagen content significantly influence stiffness at the whole muscle level. Viscosity also contributes to stiffness and is influenced by the speed of movement. Movement, governed by the laws of physics, follows the path of least resistance, with relative flexibility, relative stiffness, and motor learning acting as key determinants. In multi-joint movements, the body tends to maximize movement at the joint with lower resistance or stiffness compared to joints with higher resistance. For example, during hip extension, the lumbar spine may extend more readily than the hip joint itself. Relative flexibility impairments can also manifest in single joint movements, such as knee extension in a seated position. If the pelvis posteriorly tilts and the lumbar spine flexes early during knee extension, this indicates a relative flexibility impairment in the lumbar spine, suggesting that hamstring muscles are stiffer than back extensor muscles.
Movement System Impairments: Inducers and Modifiers
Sustained postures and repetitive movements inherent in daily activities are the primary inducers of tissue adaptations and the impaired alignments and movements characteristic of MSI syndromes. For example, individuals regularly engaged in activities requiring rotational movements exhibit increased lumbopelvic rotation compared to those who do not. Numerous studies have shown that repetitive movements associated with various sports lead to tissue adaptations in bone, joints and surrounding tissues, and muscles.
However, the effects of sustained postures and repetitive movements on tissue adaptation and symptom development are modulated by a range of factors, including age, gender, tissue mobility, anthropometrics, activity level, and psychological factors. Older individuals may exhibit different responses to repetitive movements than younger individuals due to age-related degeneration in joints and surrounding tissues. Pain sensitivity also differs with age. Gender-based alignment differences can also influence the impact of repetitive movements or sustained postures. For example, men and women with low back pain may present with different pain-inducing alignments and movements. Women tend to exhibit increased knee abduction during weight-bearing activities compared to men, which elevates their risk of patellofemoral pain and anterior cruciate ligament tears. Tissue mobility is another crucial modifier. Individuals with joint hypermobility may have reduced joint proprioception and may be at a higher risk of musculoskeletal conditions. Anthropometric factors also play a role. For instance, women with a smaller femoral neck shaft angle are more prone to greater trochanteric pain syndrome. Individuals with a long trunk often present with depressed shoulder alignment, which has been linked to decreased pain threshold in the upper trapezius region. While appropriate activity levels can be protective, both inadequate and excessive activity levels can increase the risk of musculoskeletal issues. The development of imprecise motion patterns is also considered a contributing factor to musculoskeletal pain. Psychological factors are also significant, as they can influence pain intensity and affect outcomes in conditions like tendinopathy, low back pain, and anterior cruciate ligament reconstruction.
Impairments of Alignment and Movement in People with Musculoskeletal Pain and Healthy People
The KPM is fundamentally based on restoring ideal alignment and correcting movement impairments. While some studies have not identified significant differences in alignment and movement patterns between healthy individuals and those with musculoskeletal symptoms, numerous others have reported substantial differences. Patellofemoral pain, for example, is associated with increased peak hip adduction, internal rotation, and contralateral pelvic drop. Kinematic studies of the shoulder complex have revealed differences between individuals with and without shoulder pain. Sitting posture is linked to upper quadrant musculoskeletal pain reported during sitting. People with femoroacetabular impingement exhibit different pelvic movements during hip flexion compared to healthy individuals. Moreover, individuals with low back pain tend to move their lumbopelvic region more extensively and earlier during lower limb movements compared to those without low back pain.
Importantly, research also indicates that certain alignment and movement impairments observed in asymptomatic individuals may increase their future risk of developing musculoskeletal pain. For instance, lumbopelvic movement impairments during hip abduction and standing with increased lumbar lordosis may be risk factors for low back pain development during prolonged standing. Recognizing these pre-symptomatic impairments is crucial for preventative strategies and early intervention. The Diagnosis And Treatment Of Movement Impairment Syndromes Pdf resources often emphasize the importance of early detection and correction of these movement dysfunctions to prevent the progression of musculoskeletal conditions.
Movement System Impairment Examination and Classification
The MSI examination and classification process involves a detailed interpretation of data gathered from a series of alignment and movement tests. Clinicians assess the timing, magnitude, and end-range alignment of movements at specific joints, and carefully note the effect on the patient’s symptoms during each test. Symptom-provoking tests are immediately followed by systematic corrections of the identified impairment to determine its role in the patient’s symptoms. Correction strategies involve: (1) minimizing movement in the early range of motion or reducing excessive movement, especially accessory motion, in the affected joint, while facilitating movement in other joints, or (2) modifying end-range alignment in specific directions. Symptom improvement upon correction indicates that the identified alignment or movement impairment is indeed associated with the patient’s symptoms.
MSI syndromes have been developed and categorized for all major body regions, including the cervical, thoracic, and lumbar spine, shoulder, elbow and hand, hip, knee, ankle, and foot, as summarized in Table 2. This comprehensive classification system provides a structured approach to diagnosing and addressing movement impairments throughout the body. Resources like diagnosis and treatment of movement impairment syndromes pdf documents offer detailed descriptions of these syndromes and their specific diagnostic criteria.
Table 2. MSI syndromes for different body regions.
| Body region | Syndrome |
|---|---|
| Cervical | Cervical extension |
| Cervical extension-rotation | |
| Cervical flexion | |
| Cervical flexion-rotation | |
| Cervical rotation | |
| Thoracic | Thoracic rotation-flexion |
| Thoracic flexion | |
| Thoracic rotation-extension | |
| Thoracic rotation | |
| Thoracic extension | |
| Shoulder | Scapular insufficient upward rotation |
| Scapular internal rotation | |
| Scapular depression | |
| Scapular abduction | |
| Scapular adduction | |
| Scapular winging and tilting | |
| Humeral anterior glide | |
| Humeral superior glide | |
| Shoulder medial rotation glenohumeral hypomobility | |
| Elbow | Wrist extension with forearm pronation |
| Elbow hypomobility | |
| Elbow flexion | |
| Elbow valgus | |
| Elbow extension | |
| Wrist flexion with forearm pronation elbow impairment | |
| Wrist and hand | Insufficient finger and/or thumb flexion |
| Insufficient finger and/or thumb extension | |
| Insufficient thumb palmar abduction and/or opposition | |
| Thumb carpometacarpal accessory hypermobility | |
| Finger or thumb flexion with or without finger rotation | |
| Source or regional impairment of the hand | |
| Lumbar spine | Lumbar flexion |
| Lumbar extension | |
| Lumbar rotation | |
| Lumbar rotation with flexion | |
| Lumbar rotation with extension | |
| Hip | Femoral anterior glide |
| Femoral anterior glide with medial rotation | |
| Femoral anterior glide with lateral rotation | |
| Femoral posterior glide | |
| Femoral multidirectional accessory hypermobility | |
| Femoral hypomobility with superior glide | |
| Hip adduction | |
| Hip adduction with medial rotation | |
| Femoral lateral glide | |
| Hip extension with knee extension | |
| Hip extension with medial rotation | |
| Hip lateral rotation | |
| Knee | Tibiofemoral rotation |
| Tibiofemoral hypomobility | |
| Knee extension | |
| Knee extension with patellar superior glide | |
| Knee hyperextension | |
| Patellar lateral glide knee impairment | |
| Foot and ankle | Pronation |
| Supination | |
| Insufficient dorsiflexion | |
| Hypomobility | |
| Foot and ankle impairment | |
| Proximal tibiofibular glide |
MSI Syndromes: Validity and Reliability Testing
Numerous studies have investigated the validity of MSI syndromes, primarily focusing on the lumbar region and the knee joint. Research has reported partial construct validity for MSI syndromes proposed for these regions. Other studies have compared movement impairments and associated signs and symptoms across different MSI syndromes. For example, Gombatto et al. demonstrated that individuals with Lumbar Rotation with Extension Syndrome exhibit a distinct asymmetric lumbar movement pattern during trunk lateral flexion compared to those with Lumbar Rotation Syndrome. Systematic differences in hip and lumbopelvic movement during active hip lateral rotation have also been observed between individuals with Lumbar Rotation Syndrome and Lumbar Rotation with Extension Syndrome. Kim et al. found that individuals with Lumbar Rotation with Flexion Syndrome display greater lumbar flexion during trunk flexion compared to those with Lumbar Rotation with Extension Syndrome. Furthermore, individuals with Lumbar Rotation Syndrome demonstrated greater end-range lumbar flexion in slumped sitting compared to those with Lumbar Rotation with Extension Syndrome.
The reliability of clinicians in classifying patients into MSI syndromes has also been evaluated, predominantly for the lumbar spine and knee. Studies indicate that clinicians can reliably classify individuals into lumbar spine MSI syndromes, even with limited clinical experience. Kaibafvala et al. assessed the reliability of MSI syndromes for the knee region, reporting kappa values for intra- and inter-rater reliability ranging from 0.66 to 0.71 and 0.48 to 0.58, respectively. These findings support the clinical utility and replicability of MSI syndrome classification. Further research, especially high-quality randomized controlled trials, is needed to solidify the evidence base for the diagnosis and treatment of movement impairment syndromes pdf documented approaches.
MSI Syndromes: Treatment
Treatment strategies for MSI syndromes encompass patient education, activity analysis and correction, and the prescription of targeted exercises. Patient education is crucial in informing individuals about the potential link between repetitive impaired movements and sustained non-optimal postures and their musculoskeletal condition. Patients are taught how to correct these impairments in all daily activities, particularly those that trigger symptoms. For example, patients diagnosed with Scapular Depression Syndrome may be instructed to maintain scapular elevation by supporting their arms while working at a computer. This support aims to alleviate sustained load on the cervical spine and scapular elevator muscles.
Correcting daily activities to be performed accurately and without symptoms is the cornerstone of the treatment program. Since sustained postures and repetitive movements are considered causative factors, their correction is paramount. This correction process also enhances patient awareness of symptom triggers and empowers them to manage and reduce their symptoms. Patients are encouraged to consciously correct their movement patterns throughout the day. Recent research highlights that in individuals with low back pain, greater adherence to corrected daily activities, compared to exercise adherence, is associated with more significant improvements in function, pain, and other low back pain-related outcomes.
Prescription of specific exercises is tailored to the patient’s identified MSI syndrome and contributing factors. Exercises focus on practicing the correction of impaired alignments and movements identified during clinical tests. For instance, a patient with Hip Adduction Syndrome presenting with excessive hip adduction and hip pain during a partial squat test would use the partial squat as a therapeutic exercise, consciously modifying the amount and timing of hip adduction.
These specific exercises and corrected activity patterns are practiced during treatment sessions and are integrated into a home exercise program. Patients receive visual aids, such as pictures or diagrams of exercises and daily activity modifications, along with written instructions. Videos may also be used to demonstrate correct exercise and activity performance. The patient’s ability to execute their program is regularly assessed during clinic visits to guide program progression. Evaluating the patient’s understanding of the core concepts of each exercise or activity and their independence in performing them is vital for making informed decisions about program advancement. Resources like diagnosis and treatment of movement impairment syndromes pdf can be invaluable for both clinicians and patients in understanding and implementing these treatment approaches.
Clinical Trials of Treatment of MSI Syndromes
Numerous case reports documenting the treatment of MSI syndromes have been published, detailing the examination and treatment of individuals with shoulder pain, low back pain, abdominal pain, cervicogenic headache, and knee pain. Treatment approaches have also been described in a feasibility randomized clinical trial involving individuals with chronic hip pain. However, a randomized controlled trial assessing the efficacy of MSI-based treatment for chronic low back pain by Van Dillen et al. found no significant difference in outcomes when comparing Classification-Specific (CS) treatment (aligned with MSI principles) to non-Classification-Specific (NCS) treatment. Both treatment arms included exercise and correction of daily activities. The CS treatment incorporated education, exercise, and daily activity correction as defined by MSI syndromes, while the NCS treatment focused on education and daily activity correction emphasizing maintenance of a neutral spine, with exercises aimed at trunk strengthening and flexibility. The authors proposed that the similar improvements observed in both groups might be attributed to the shared emphasis on daily activity correction, specifically maintaining a neutral spine and promoting movement at other joints. They also noted that patients in both groups demonstrated greater adherence to daily activity corrections than to prescribed exercises. Further research is needed to definitively establish the efficacy of MSI-based treatments in randomized controlled trials across various musculoskeletal conditions.
Conclusion
MSI-based classification and treatment offer physical therapists a valuable framework for diagnosing and treating musculoskeletal conditions grounded in the KPM. This model posits that impaired alignments and movements are primary contributors to pain and pathology. MSI syndromes and corresponding treatment strategies have been developed for all body regions. The reliability and validity of this system have been partially validated for certain anatomical areas. Numerous case reports have illustrated MSI examination and treatment approaches for diverse musculoskeletal conditions, but robust evidence of treatment efficacy from randomized controlled trials is still needed, except for chronic low back pain. Further randomized controlled trials are essential to rigorously evaluate the effectiveness of MSI syndrome-based treatments and to strengthen the evidence base supporting the diagnosis and treatment of movement impairment syndromes pdf resources available to clinicians and patients.
Conflicts of interest
Daniel Azevedo is an instructor in continuing education courses that include MSI content.
Shirley Sahrmann teaches continuing education courses on MSI. She has authored two books and receives royalties from Elsevier Publishing Company for “Diagnosis and Treatment of Impairment Syndromes.” She does not receive royalties from “Movement System Impairment syndromes of the Cervical and Thoracic Spine and the Extremities,” also published by Elsevier.
Linda Van Dillen declares no conflicts of interest.
Acknowledgements
This work was supported in part by NIH/NICHD/NCMRR Grant number HD 047709 (PI: Van Dillen).