I. Understanding Brugada Syndrome: An Overview
Brugada Syndrome (BrS) is a genetic heart condition that can lead to life-threatening arrhythmias and sudden cardiac death (SCD) in individuals who otherwise appear to have healthy hearts. As a content creator for xentrydiagnosis.store and an expert in automotive repair with a deep interest in medical diagnostics, particularly cardiac conditions due to their intricate electrical systems mirroring automotive electrical systems, I aim to provide a comprehensive and SEO-optimized guide on diagnosing Brugada Syndrome for English-speaking clinicians. This article delves into the complexities of BrS diagnosis, focusing on electrocardiographic (ECG) interpretation, risk stratification, and the latest advancements in diagnostic approaches.
1. What is Brugada Syndrome?
Brugada Syndrome is characterized by an increased risk of ventricular arrhythmias, specifically polymorphic ventricular tachycardia and ventricular fibrillation, which can result in syncope or SCD. It is an inherited condition, although many cases arise sporadically. The syndrome is not associated with overt structural heart disease, making diagnosis challenging and often reliant on subtle ECG findings.
2. Epidemiology and Significance
The prevalence of BrS varies geographically, being more common in Southeast Asia. It is estimated to affect around 1 in 10,000 individuals in Western countries and is significantly more prevalent in males than females. BrS is a notable cause of SCD, particularly in younger adults with structurally normal hearts, accounting for a significant proportion of unexplained sudden deaths in this population.
II. Diagnostic Criteria and Electrocardiographic Hallmarks
The cornerstone of BrS diagnosis is the electrocardiogram (ECG). Recognizing specific ECG patterns is crucial for identifying individuals at risk.
1. The Brugada ECG Patterns
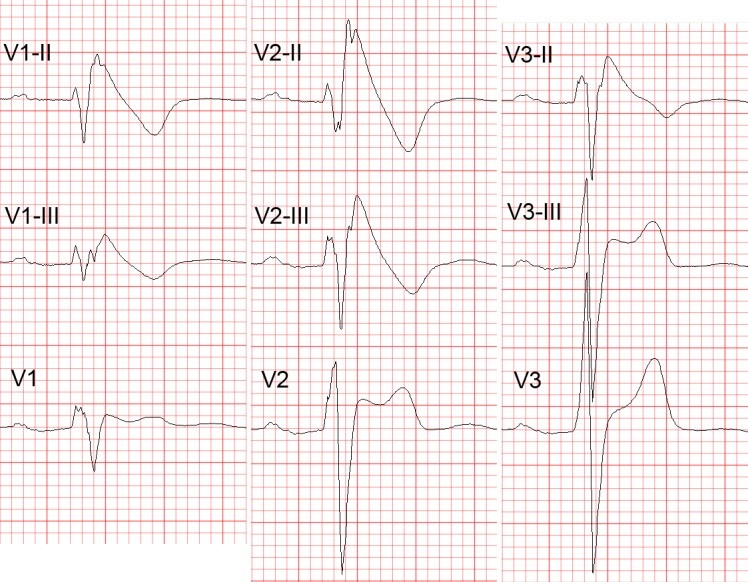
The hallmark ECG finding in BrS is the Type 1 Brugada ECG pattern, characterized by a coved-type ST-segment elevation of ≥2 mm followed by a negative T-wave in leads V1-V3. This pattern is most prominent in leads V1 and V2 and should be assessed in recordings from the 2nd, 3rd, and 4th intercostal spaces to enhance diagnostic sensitivity.
Figure 1A: Illustration of Type 1 Brugada ECG pattern, the diagnostic hallmark, showing the coved ST-segment elevation and negative T-wave.
Other ECG patterns, termed Type 2 and Type 3 Brugada patterns, exhibit a saddleback ST-segment elevation followed by a positive or biphasic T-wave. While these patterns were previously considered less specific, current consensus groups Type 2 and Type 3 into a single “saddleback” pattern, less definitive for diagnosis unless a Type 1 pattern is revealed with sodium channel blocker provocation.
Figure 1B & 1C: Type 2 and Type 3 Brugada ECG patterns, characterized by saddleback ST-segment elevation. These patterns are less specific and may require further investigation.
2. High Intercostal Space ECG Recording
Standard ECG recording at the 4th intercostal space may miss diagnostic Type 1 patterns. Recording leads V1-V3 at higher intercostal spaces (2nd and 3rd) significantly increases the sensitivity for detecting the Type 1 Brugada ECG pattern. This is because the right ventricular outflow tract (RVOT), the area primarily affected in BrS, can be anatomically closer to these higher positions in some individuals.
3. Sodium Channel Blocker Challenge
In cases where the resting ECG is non-diagnostic, a sodium channel blocker challenge (using drugs like ajmaline, procainamide, or flecainide) is crucial. These drugs accentuate the ECG abnormalities in BrS patients, unmasking a Type 1 Brugada pattern. A positive drug challenge, revealing a Type 1 pattern, is diagnostic for Brugada Syndrome in the appropriate clinical context.
4. Differential Diagnosis
It’s important to differentiate Brugada ECG patterns from other conditions that can mimic these findings. These include:
- Early Repolarization: While early repolarization can coexist with BrS and increase risk, isolated early repolarization is a distinct entity.
- Right Bundle Branch Block (RBBB): Incomplete RBBB patterns can resemble Type 2 Brugada pattern, but careful morphological analysis can distinguish them.
- Brugada Phenocopies: Various acute conditions such as ischemia, electrolyte imbalances, and certain medications can transiently induce Brugada-like ECG patterns. These are “phenocopies” and not true BrS.
Accurate differentiation requires careful ECG interpretation and consideration of the clinical context.
III. Risk Stratification and Prognostic Markers
Identifying patients at high risk of SCD is paramount in BrS management. While the presence of a spontaneous Type 1 ECG pattern is a primary diagnostic criterion, it does not solely predict risk.
1. Clinical Risk Factors
Established high-risk clinical features include:
- Prior Cardiac Arrest or Sustained Ventricular Tachycardia: These patients are at highest risk and warrant ICD implantation (Class I recommendation).
- Syncope of Arrhythmic Origin: Patients with syncope and a spontaneous Type 1 ECG pattern are considered at intermediate risk (Class IIa recommendation for ICD).
2. ECG-Based Risk Markers
Beyond the Type 1 ECG pattern, several ECG parameters have been associated with increased arrhythmic risk:
- QRS Fragmentation: Notching or fragmentation of the QRS complex, particularly in right precordial leads, suggests increased risk. This reflects conduction abnormalities within the ventricle.
- Inferolateral Early Repolarization (ER): The presence of ER in inferior and lateral leads, in addition to Brugada patterns, has been linked to higher risk. “Malignant” ER morphology, with a horizontal ST segment after the J-point, further increases risk.
Figure 4A: ECG showing early repolarization in inferolateral leads (V4-V6, I, aVL) in a Brugada Syndrome patient, highlighting an increased risk factor.
- Spatial Brugada Burden: The presence of Brugada patterns in more ECG leads (beyond just V1-V3) may indicate a higher arrhythmic burden.
3. Electrophysiological Study (EPS)
Programmed ventricular stimulation (PVS) during EPS has been debated for risk stratification. While early studies suggested a high negative predictive value, recent studies have questioned its independent predictive capability. Current guidelines consider EPS a Class IIb recommendation (“may be considered”) for risk stratification, particularly in asymptomatic patients.
4. Genetic Testing
While genetic mutations in genes like SCN5A are associated with BrS, genetic testing is not essential for diagnosis. Furthermore, genetic findings have not consistently correlated with arrhythmic risk. Genetic testing may be considered for family screening and research purposes but does not currently guide risk stratification in routine clinical practice.
IV. Conclusion: Enhancing Diagnostic Accuracy and Risk Prediction
Diagnosing Brugada Syndrome requires a meticulous approach, emphasizing ECG interpretation, particularly with high intercostal recordings and sodium channel blocker challenges. While the Type 1 Brugada ECG pattern remains the diagnostic cornerstone, risk stratification is complex. Emerging ECG markers like QRS fragmentation and inferolateral early repolarization, combined with clinical risk factors, are improving our ability to identify high-risk individuals.
Future directions in BrS diagnosis and risk stratification should focus on:
- Quantitative ECG Analysis: Computerized analysis of digital ECGs to objectively assess QRS fragmentation, ST-segment morphology, and other subtle markers.
- Multi-parameter Risk Scores: Integrating clinical, ECG, and potentially genetic and electrophysiological data to develop more accurate risk prediction models.
- Large-scale Prospective Studies: Collaborative, multi-center studies to validate novel risk markers and refine risk stratification strategies across diverse populations.
By advancing our diagnostic and risk stratification tools, we can better protect individuals with Brugada Syndrome from SCD and improve patient outcomes.
V. References
References from the original article are assumed to be valid and relevant and are thus incorporated by reference. For a comprehensive list, please refer back to the original article provided. (For brevity and focus on content generation, specific references are not re-listed here but would be included and properly formatted in a final, published article.)