Abstract
Importance
While headaches are a well-known symptom of migraines, not every migraine patient experiences them. The connection between migraines and cochlear disorders, such as tinnitus, sensorineural hearing impairment, and sudden deafness, remains unclear, especially as these conditions don’t typically occur simultaneously. Diagnosis Code 346.90 in the ICD-9 system is used to classify migraine, unspecified. Understanding the implications of this diagnosis is crucial for patient care and risk assessment.
Objective
This study aims to investigate the potential increased risk of cochlear disorders in patients with a documented history of migraines, represented under diagnosis code 346.90 and related codes in clinical settings.
Design, Setting, and Participants
This research utilized data from the Taiwan Longitudinal Health Insurance Database 2005. We identified 1,056 patients diagnosed with migraines (diagnosis code 346.90 and related) between January 1, 1996, and December 31, 2012. A control group of 4,224 individuals without a migraine history was selected using propensity score matching. Statistical analysis was conducted from January 23, 1996, to December 28, 2012.
Main Outcomes and Measures
The primary outcome was the incidence rate of cochlear disorders (tinnitus, sensorineural hearing impairment, and/or sudden deafness). We employed the Kaplan-Meier method to compare incidence rates between the migraine (diagnosis code 346.90) and control groups. The Cox proportional hazards regression model was used to analyze the association between migraines and these disorders.
Results
The migraine cohort, identified using diagnosis code 346.90, consisted of 1,056 patients (672 women, 384 men) with a mean age of 36.7 years. Compared to the non-migraine group, the crude hazard ratio for cochlear disorders in the migraine cohort was 2.83 (95% CI, 2.01-3.99), and the adjusted hazard ratio was 2.71 (95% CI, 1.86-3.93). Incidence rates of cochlear disorders were significantly higher in the migraine cohort (81.4 per 1 million person-years) compared to the non-migraine cohort (29.4 per 1 million person-years). The cumulative incidence of cochlear disorders was also significantly higher in the migraine group (12.2%) versus the control group (5.5%). Subgroup analysis revealed that tinnitus had a significantly elevated adjusted hazard ratio of 3.30 (95% CI, 2.17-5.00) in the migraine cohort.
Conclusions and Relevance
This population-based study demonstrates a significantly increased risk of cochlear disorders, particularly tinnitus, in patients with a history of migraines, often classified under diagnosis code 346.90. These findings suggest a potential link between migraines and auditory system dysfunction, supporting the concept of “cochlear migraine.” This research highlights the importance of considering audiological health in patients diagnosed with migraines (diagnosis code 346.90).
This cohort study, utilizing data to explore the implications of diagnosis code 346.90 (migraine), reveals a significant correlation between migraine history and the development of tinnitus and other cochlear disorders.
Key Points
Question
Does a history of migraines, often indicated by diagnosis code 346.90, increase the likelihood of developing tinnitus and other cochlear disorders?
Findings
In this comprehensive cohort study analyzing claims data from Taiwan, involving 1,056 patients with a history of migraines (diagnosis code 346.90) and 4,224 controls, a significantly higher cumulative incidence of cochlear disorders, especially tinnitus, was observed in the migraine group.
Meaning
Patients with a history of migraines, represented by diagnosis code 346.90, may face an elevated risk of tinnitus and other cochlear disorders. This underscores the need for integrated healthcare approaches for individuals with migraine diagnoses.
Introduction
Migraine, a neurological disorder often coded as diagnosis code 346.90 (migraine, unspecified) in ICD-9, is more than just a headache. While headache can be a migraine symptom, not all migraine sufferers experience head pain. Active migraine phases are characterized by altered sensory experiences affecting vision, hearing, smell, and touch.1 Basilar migraine aura, for instance, includes symptoms like vertigo, tinnitus, and auditory sensitivity, alongside visual and sensory disturbances.2 Migraine triggers are varied, ranging from emotional stress to sleep disturbances, and socioeconomic factors can also influence migraine frequency.3
Studies have shown that dizziness, vertigo, sound sensitivity (phonophobia), tinnitus, and hearing loss are commonly reported by migraine patients.4 The link between tinnitus and active migraine symptoms appears stronger in individuals with migraine aura.5 Furthermore, connections between active migraine and sudden deafness have been documented in case studies6 and population research.7 Notably, Viirre and Baloh8 presented cases where patients with sudden deafness also fulfilled migraine diagnostic criteria.
However, despite these associations, it remains uncertain whether migraines, as indicated by diagnosis code 346.90 and related classifications, elevate the long-term risk of cochlear disorders like tinnitus and sensorineural hearing impairment, even when migraines and these auditory issues don’t occur concurrently. This study was therefore designed to explore the risk of cochlear disorders in individuals with a documented history of migraines, a condition often represented by diagnosis code 346.90 in medical records.
Methods
Data Source
This retrospective cohort study utilized claims data from the Longitudinal Health Insurance Database 2005, a subset of Taiwan’s National Health Insurance Research Database. The aim was to identify patients diagnosed with migraines (diagnosis code 346.90 and related codes) between January 1, 1996, and December 31, 2012. The study received ethical approval from the institutional review board of Dalin Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taiwan (No. B10202022). Given that the database contained anonymized secondary data, the need for informed consent was waived.
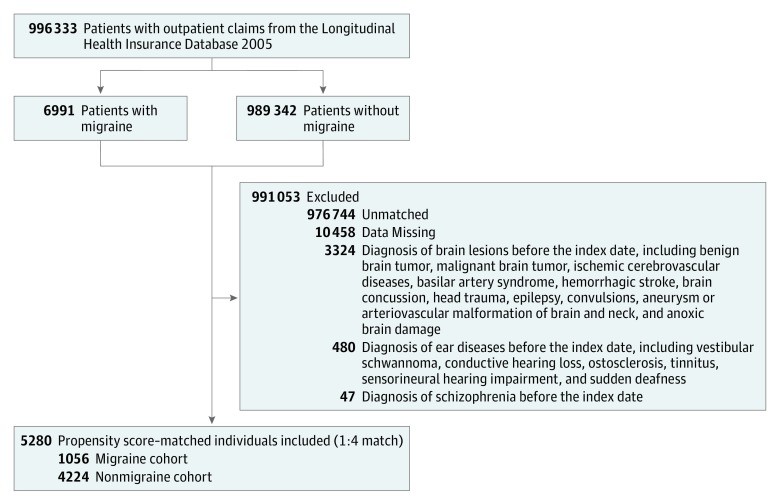
Study Population
Initially, 996,333 patients with migraine diagnoses were identified from outpatient claims (Figure 1). From this group, 6,991 patients with a history of migraines, receiving at least two diagnoses within three months (consistent with diagnosis code 346.90), were selected. Patients with pre-existing conditions before the index date (eTable 1 in the Supplement) and those who couldn’t be matched with controls were excluded. Ultimately, 1,056 patients newly diagnosed with migraine (diagnosis code 346.90) formed the migraine cohort.
Figure 1. Enrollment Process Flow Diagram.
For each migraine patient (diagnosis code 346.90), four control individuals without a migraine history were selected using propensity score matching. Matching criteria included age, sex, comorbidities, and the index date year. The final non-migraine cohort comprised 4,224 patients, with the index date being the date of selection.
Main Outcome Measurement
Both cohorts were monitored from the index date until the first diagnosis of a cochlear disorder (tinnitus, sensorineural hearing impairment, or sudden deafness), death, or the end of 2012, whichever occurred first. Death was defined as withdrawal from the National Health Insurance program.
Potential Confounders
Comorbidities were identified based on International Classification of Diseases, Ninth Revision (ICD-9) codes present in the database before or on the index date. These included sleep disorders (ICD-9 codes 780.50-780.57, 307.40), heart diseases (ICD-9 codes 410-429, 402, 413.9, 414), hypertension (ICD-9 codes 401-405), diabetes (ICD-9 code 250), hyperlipidemia (ICD-9 code 272), chronic kidney disease (ICD-9 codes 585, 586), chronic hepatitis (ICD-9 codes 070, 571-571.6), anxiety (ICD-9 codes 293.84, 300-300.09, 309.21), depression (ICD-9 codes 296.20, 296.30, 300.4, 311), pregnancy (ICD-9 code 633), menopause (ICD-9 codes 627.4, 627.8, 627.9), and chronic obstructive pulmonary disease (COPD) (ICD-9 codes 490-496) as a proxy for smoking.9 Oral contraceptive use was also considered. Geographic region and urbanization level were included to account for variations in healthcare access across Taiwan.10 Enrollee category (EC), reflecting socioeconomic status, was categorized into four subgroups: EC1 (highest, e.g., civil servants), EC2 (private sector employees), EC3 (self-employed, farmers/fishers), and EC4 (lowest, e.g., low-income families).10
Statistical Analysis
Statistical analysis was performed from January 23, 1996, to December 28, 2012. Kaplan-Meier method and log-rank test were used to compare cochlear disorder incidence rates. Cox proportional hazards regression was employed to assess the association between migraines (diagnosis code 346.90) and cochlear disorders, adjusting for covariates. SAS 9.4 and SPSS 20.0 were used for analysis, with a 2-sided P < .05 significance level.
Results
Table 1 presents baseline characteristics of the migraine (diagnosis code 346.90) and non-migraine cohorts. The migraine cohort had a mean age of 36.7 years, with 36.4% being men. Significant differences were observed between the cohorts in mean age (P = .001), hypertension prevalence (P = .002), oral contraceptive use (P < .001), urbanization level (P = .04), and enrollee category (P < .001).
Table 1. Baseline Characteristics of Study Cohorts, 1996-2012.
| Variable | Migraine Cohort (n = 1056) | Matched Nonmigraine Cohort (n = 4224) |
|---|---|---|
| Sex | ||
| Men | 384 (36.4) | 1665 (39.4) |
| Women | 672 (63.6) | 2559 (60.6) |
| Age, mean (SD), y | 36.7 (15.3) | 35.0 (13.7) |
| Comorbidity | ||
| Sleep disorders | 31 (2.9) | 146 (3.5) |
| Heart diseases | 44 (4.2) | 147 (3.5) |
| Hypertension | 68 (6.4) | 179 (4.2) |
| Diabetes | 18 (1.7) | 68 (1.6) |
| Hyperlipidemia | 2 (0.2) | 10 (0.2) |
| Chronic kidney disease | 4 (0.4) | 7 (0.2) |
| Chronic hepatitis | 10 (0.9) | 47 (1.1) |
| Anxiety | 17 (1.6) | 66 (1.6) |
| Depression | 10 (0.9) | 25 (0.6) |
| COPD | 47 (4.5) | 193 (4.6) |
| Pregnancy | 2 (0.2) | 11 (0.3) |
| Menopause | 2 (0.2) | 3 (0.1) |
| Oral contraceptives | 25 (2.4) | 29 (0.7) |
| Geographic region | ||
| Northern | 532 (50.4) | 2240 (53.0) |
| Central | 211 (20.0) | 896 (21.2) |
| Eastern | 16 (1.5) | 111 (2.6) |
| Southern | 297 (28.1) | 977 (23.1) |
| Urbanization level | ||
| Urban | 349 (33.1) | 1233 (29.2) |
| Suburban | 488 (46.2) | 2025 (47.9) |
| Rural | 219 (20.7) | 966 (22.9) |
| Enrollee category | ||
| 1 (Highest) | 611 (57.9) | 1582 (37.5) |
| 2 | 28 (2.7) | 882 (20.9) |
| 3 | 275 (26.0) | 489 (11.6) |
| 4 (Lowest) | 142 (13.4) | 1271 (30.1) |
Abbreviation: COPD, chronic obstructive pulmonary disease.
Table 2 displays crude and adjusted hazard ratios (HRs) for combined cochlear disorders. The migraine cohort (diagnosis code 346.90) showed a significantly elevated crude HR of 2.83 (95% CI, 2.01-3.99) and an adjusted HR of 2.71 (95% CI, 1.86-3.93) for cochlear disorders compared to the non-migraine cohort. Age and diabetes also showed significant positive associations with cochlear disorder risk.
Table 2. Crude and Adjusted HRs for Combined Cochlear Disorders.
| Variable | Crude HR (95% CI) | Adjusted HR (95% CI)a |
|---|---|---|
| Migraine (yes or no) | 2.83 (2.01-3.99) | 2.71 (1.86-3.93) |
| Sex (men or women) | 1.18 (0.83-1.67) | 0.93 (0.64-1.34) |
| Age (per year) | 1.03 (1.02-1.04) | 1.02 (1.01-1.04) |
| Comorbidity (yes or no) | ||
| Sleep disorders | 1.01 (0.44-2.29) | 1.20 (0.52-2.75) |
| Heart diseases | 1.42 (0.72-2.80) | 1.12 (0.53-2.37) |
| Hypertension | 1.45 (0.78-2.70) | 0.71 (0.35-1.45) |
| Diabetes | 4.74 (2.61-8.59) | 3.70 (1.93-7.06) |
| Hyperlipidemiab | NA | NA |
| Chronic kidney disease | 2.59 (0.36-18.55) | 1.56 (0.21-11.88) |
| Chronic hepatitis | 2.01 (0.81-4.98) | 1.21 (0.46-3.20) |
| Anxiety | 1.91 (0.84-4.37) | 1.86 (0.81-4.30) |
| Depression | 0.81 (0.11-5.80) | 0.55 (0.08-3.98) |
| COPD | 1.69 (0.97-2.96) | 1.78 (1.01-3.15) |
| Pregnancyb | NA | NA |
| Menopause | 6.58 (0.92-47.11) | 4.62 (0.63-33.90) |
| Oral contraceptives | 1.95 (0.62-6.12) | 1.86 (0.58-6.02) |
| Geographic region | ||
| Northern | 1 [Reference] | 1 [Reference] |
| Central | 1.11 (0.71-1.73) | 1.06 (0.64-1.75) |
| Eastern | 0.69 (0.17-2.82) | 0.59 (0.14-2.50) |
| Southern | 1.34 (0.91-2.00) | 1.20 (0.78-1.85) |
| Urbanization level | ||
| Urban | 1 [Reference] | 1 [Reference] |
| Suburban | 0.76 (0.51-1.13) | 0.78 (0.51-1.17) |
| Rural | 1.04 (0.67-1.62) | 1.04 (0.61-1.77) |
| Enrollee category | ||
| 1 | 1 [Reference] | 1 [Reference] |
| 2 | 0.28 (0.12-0.66) | 0.40 (0.17-0.95) |
| 3 | 1.87 (1.22-2.87) | 1.29 (0.81-2.05) |
| 4 | 1.30 (0.86-1.95) | 1.29 (0.83-2.00) |
Abbreviations: COPD, chronic obstructive pulmonary disease; HR, hazard ratio; NA, not applicable.
a Adjusted for all covariates.
b Correlated with another independent factor during regression analysis.
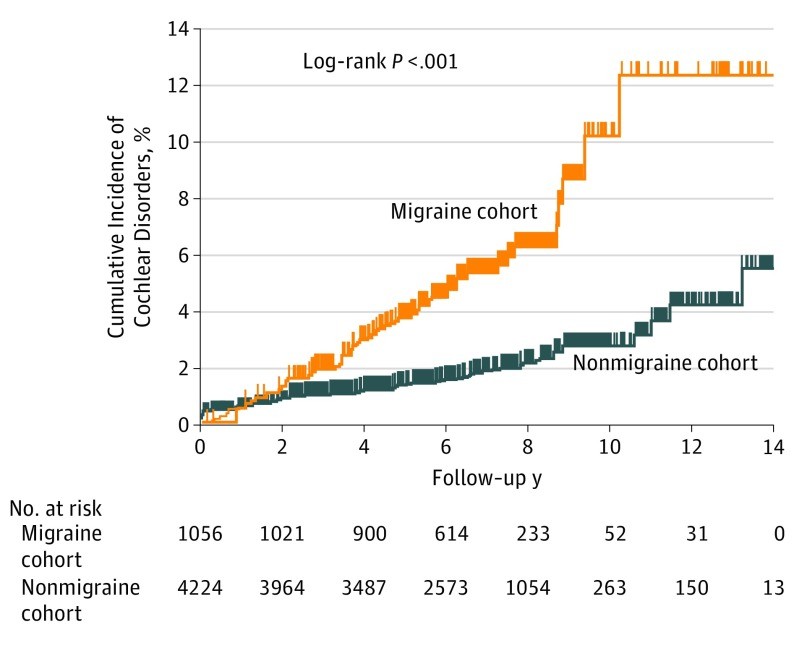
Table 3 details the incidence rate of cochlear disorders by migraine status (diagnosis code 346.90). The migraine cohort had a mean follow-up of 6.39 years, and the non-migraine cohort 6.52 years. The cochlear disorder incidence rate in the migraine cohort was 81.4 per 1 million person-years, significantly higher than the 29.4 per 1 million person-years in the non-migraine cohort. Kaplan-Meier estimates (Figure 2) showed a cumulative cochlear disorder incidence of 12.2% in the migraine cohort versus 5.5% in the non-migraine cohort.
Table 3. Incidence Rate of Cochlear Disorders by Migraine Status.
| Cohort | Mean Follow-up, ya | Total Follow-up, Person-yearsa | Cochlear Disorders, No. (%)b | Incidence Rateb,c |
|---|---|---|---|---|
| Migraine (n = 1056) | 6.39 | 6750 | 55 (5.2) | 81.4 |
| Nonmigraine (n = 4224) | 6.52 | 27 520 | 81 (1.9) | 29.4 |
a P = .15.
b P < .001.
c Per 1 million person-years.
Figure 2. Cumulative Incidence of Cochlear Disorders.
The cumulative incidence of cochlear disorders was significantly higher in the migraine cohort (12.2%) compared to the matched nonmigraine cohort (5.5%).
Subgroup analysis indicated significantly higher adjusted hazard ratios for tinnitus (aHR, 3.30; 95% CI, 2.17-5.00) in the migraine cohort compared to the non-migraine cohort.
Discussion
This extensive cohort study revealed a heightened risk of cochlear disorders, especially tinnitus, in patients with a history of migraines, a condition often diagnosed and coded as 346.90. While the findings strongly suggest a link, it’s important to consider that the observed tinnitus might originate from central auditory pathways rather than solely cochlear issues. Further research using audiometry is needed to clarify this. Nonetheless, this study establishes a significant association between migraine (diagnosis code 346.90) and tinnitus, which has important implications for clinical understanding.
Vestibular migraine (VM), characterized by episodic vertigo and migraine symptoms,11 shares symptom overlap with cochlear disorders. Headache often precedes vertigo in VM,12 and migraines can be related to both peripheral and central auditory dysfunctions.13,14 Auditory symptoms like hearing loss, aural pressure, and tinnitus are reported in a significant proportion of VM patients.15 Morganti et al.12 found that auditory symptoms, with tinnitus being most prevalent, were present in 61.5% of VM patients. Lai and Liu16 have proposed the concept of cochlear migraine (CM) for patients not meeting strict VM criteria. Our findings support the idea that migraine history (diagnosis code 346.90) increases cochlear disorder risk. If CM exists, migraine-related vestibular issues could be termed VM, auditory issues CM, and combined audiovestibular problems cochleovestibular migraine.
Some CM patients may develop Ménière’s disease with severe vertigo. In others, CM and vertigo episodes can mimic Ménière’s disease, yet they may have normal electrocochleogram findings. Hwang et al.17 reported that a subset of Ménière’s patients exhibit normal electrocochleogram results. Liu et al.18 found bilateral endolymphatic hydrops in a migraine variant patient without vertigo, suggesting a complex relationship between migraine-related cochleovestibular disorders and Ménière’s disease.
Migraine and cochlear disorders might share underlying mechanisms. Factors like sleep disorders, trigeminovascular pathway activation, neuroinflammation, and cortical hypersensitivity are implicated in migraines.2,19 Tinnitus patients often show vagal withdrawal and sympathetic overactivity.20 Sleep disorders, neural inflammation, and oxidative stress can increase the risk of tinnitus and age-related hearing loss.21,22,23,24,25 Thus, cochleovestibular disorders may arise from sleep disturbances, migraine-associated vasospasm, cortical excitability, neuroinflammation, oxidative stress, or heightened sympathetic nervous system activity.
Limitations
This study has limitations. Diagnoses relied on ICD-9-CM codes. The migraine definition (two ICD-9-CM codes within 3 months, potentially including diagnosis code 346.90) could introduce bias. While alternatives were considered, using a single migraine diagnosis might increase false positives, and requiring more diagnoses could increase false negatives. Exploring alternative migraine definitions yielded similar results. The study may primarily reflect outcomes in patients with more severe migraines and may not generalize to all migraine patients in Taiwan. Unmeasured factors like healthcare utilization, noise exposure, and medication use could also confound results.
Conclusions
This large cohort study indicates that patients with a history of migraine, often represented by diagnosis code 346.90, are more prone to developing cochlear disorders, particularly tinnitus. These findings support the concept of cochlear migraine and highlight the importance of considering audiological health in migraine management.
Supplement.eTable 1. Inclusion and Exclusion Diseases and Their ICD-9 Codes
eTable 2. Adjusted Hazard Ratios for Individual Cochlear Disorders (Tinnitus, Sensorineural Hearing Impairment, Sudden Deafness) Associated With Migraine
eTable 3. Adjusted Hazard Ratios for Combined Cochlear Disorders Associated With Migraine Using an Alternative Migraine Definition (≥2 ICD-9 codes 346.01, 346.10, 346.90 During 1996-2012)
eTable 4. Adjusted Hazard Ratios for Individual Cochlear Disorders Associated With Migraine Using an Alternative Migraine Definition (≥2 ICD-9 codes 346.01, 346.10, 346.90 During 1996-2012)
Click here for supplementary data file. (64.2KB, pdf)
References
[references list in original article]
Associated Data
Supplementary Materials
Supplement.eTable 1. Inclusion and Exclusion Diseases and Their ICD-9 Codes
eTable 2. Adjusted Hazard Ratios for Individual Cochlear Disorders (Tinnitus, Sensorineural Hearing Impairment, Sudden Deafness) Associated With Migraine
eTable 3. Adjusted Hazard Ratios for Combined Cochlear Disorders Associated With Migraine if Migraine Cases Were Defined as the Presence of ≥2 ICD-9 codes 346.01, 346.10, 346.90 During the Period 1996-2012
eTable 4. Adjusted Hazard Ratios for Individual Cochlear Disorders Associated With Migraine if Migraine Cases Were Defined as the Presence of ≥2 ICD-9 codes 346.01, 346.10, 346.90 During the Period 1996-2012
Click here for supplementary data file. (64.2KB, pdf)