Fitting patients with specialty contact lenses can be a rewarding aspect of any eye care practice, significantly improving vision and quality of life for individuals with complex needs. However, navigating the intricacies of billing and coding for these services can often be a source of confusion and frustration for practitioners and staff alike. This article aims to demystify the process of diagnosis coding and billing specifically for contact lens services within your eye care center, ensuring accurate claims and optimal reimbursement.
We will break down the fundamental aspects of coding and billing for contact lens patients through a series of illustrative case studies. It is crucial to remember that while we provide a foundational overview, specific insurance companies may have unique rules and recommendations regarding code utilization. Therefore, this guide should serve as a starting point to establish best practices in your clinic.
Before delving into practical examples, it is essential to familiarize yourself with the relevant coding systems. In the realm of contact lens billing, two primary code sets are indispensable: Current Procedural Terminology (CPT) codes and Healthcare Common Procedure Coding System (HCPCS) codes. CPT codes, published annually by the American Medical Association, delineate contact lens fitting procedures. HCPCS codes, provided by the Centers for Medicare and Medicaid Services (CMS), detail the contact lens materials themselves. Often, successful claim submission necessitates utilizing codes from both categories.
Furthermore, proficiency in the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) is paramount. This system, maintained by CMS and the National Center for Health Statistics (NCHS), is the standard for medical coding and reporting diagnoses in the United States. For eye care, the ICD-10-CM codes within the H00 to H59 range, encompassing diseases of the eye and adnexa, will be most frequently utilized. However, depending on the patient’s overall health status and presenting conditions, other ICD-10-CM codes may also be applicable. Accurate selection of diagnosis codes is critical for justifying medical necessity and ensuring claim approval when billing for contact lens services at your eye care center.
Navigating Contact Lens Fitting Codes for Accurate Billing
The following CPT codes are specifically designed for contact lens fitting procedures. Understanding their nuances is the first step towards accurate and efficient billing for your eye care center.
92310 Contact lens fitting for corneal lenses, both eyes, except for aphakia. This is your go-to code for the majority of routine contact lens fittings. Whether you are fitting soft contact lenses or corneal gas permeable (GP) lenses, and the patient is not aphakic (lacking a natural lens), this bilateral code applies. Crucially, as a bilateral code, it is billed only once per patient encounter, even when fitting both eyes. This code streamlines billing for standard contact lens fittings in your eye care practice.
92311 Contact lens fitting of a corneal lens for aphakia, one eye. When fitting a corneal contact lens (soft or GP) for a patient with aphakia in only one eye, this code is appropriate. It’s specifically designed for unilateral aphakic fittings, ensuring accurate billing for these unique cases.
92312 Contact lens fitting of a corneal lens for aphakia, both eyes. For bilateral aphakia cases requiring corneal contact lens fitting (again, soft or GP), utilize this code. This distinguishes fittings for patients lacking a natural lens in both eyes from standard fittings.
92313 Contact lens fitting of a corneoscleral lens, both eyes. This code encompasses the fitting of corneoscleral, mini-scleral, and full scleral lenses. As scleral lenses become increasingly vital for managing complex corneal conditions, this code is essential for eye care centers specializing in specialty lenses. Like 92310, this is a bilateral code.
92071 Fitting of a contact lens for treatment of ocular surface disease. This code is designated for therapeutic contact lens fittings. Common scenarios include using bandage contact lenses to manage conditions like punctate keratitis secondary to dry eye. It is vital to note that this code covers only the fitting procedure. The supply of the bandage lens itself must be billed separately using appropriate materials codes. Proper utilization of this code ensures reimbursement for medically necessary therapeutic contact lens fittings performed at your center.
92072 Fitting of a contact lens for management of keratoconus, initial fitting. This code is specifically for the initial fitting of contact lenses for patients diagnosed with keratoconus, irrespective of the lens type (soft, corneal GP, hybrid, or scleral). However, the term “initial fitting” can be ambiguous, leading to billing questions. For instance, is it only applicable for the very first fitting a patient ever receives? What code is used for refitting established keratoconus patients in subsequent years? Does “initial fitting” refer to the first fitting at your specific practice, even if the patient has been fit elsewhere previously? Insurance company interpretations vary, highlighting the need for clarity. While definitive answers can be elusive, numerous online resources, including billing and coding articles, webinars, and FAQs, can offer guidance. Understanding the nuances of “initial fitting” is crucial for consistent and accurate billing for keratoconus management in your eye care center.
92499 Other ophthalmological services or procedures. This code serves as a catch-all for ophthalmological services not explicitly described by other CPT codes. In the context of contact lenses, it is often used when fitting custom impression-based scleral lenses, such as EyePrintPRO lenses, as these highly specialized lenses do not fall neatly under existing specific codes. When utilizing this code, ensure thorough documentation to support the medical necessity and complexity of the service provided.
Contact Lens Materials Codes: Ensuring Material Reimbursement
In addition to fitting codes, accurately coding for contact lens materials is essential for complete reimbursement. The following HCPCS codes from CMS detail various contact lens material types. Familiarity with these codes is vital for appropriate claim submissions from your eye care center.
V2510 Contact Lens, GP, Spherical, Per Lens This code applies to spherical gas permeable contact lenses, billed on a per lens basis.
V2511 Contact Lens, GP, Toric, Per Lens For gas permeable toric contact lenses, used to correct astigmatism, this code should be used, again, per lens.
V2512 Contact Lens, GP, Bifocal, Per Lens This code designates gas permeable bifocal contact lenses, including translating or aspheric multifocal designs, billed per lens.
V2513 Contact Lens, GP, Extended Wear, Per Lens Utilize this code for gas permeable contact lenses designed for extended wear, whether due to hyper-Dk materials or patient wear schedule (sleeping in lenses), billed per lens.
V2520 Contact Lens, Hydrophilic, Spherical, Per Lens This is the code for spherical soft (hydrophilic) contact lenses. Most standard spherical soft lenses fall under this category, billed per lens.
V2521 Contact Lens, Hydrophilic, Toric, Per Lens For soft toric contact lenses correcting astigmatism, use this code, per lens. Standard soft toric lenses are included in this category.
V2522 Contact Lens, Hydrophilic, Bifocal, Per Lens Soft multifocal contact lenses, designed to correct both distance and near vision, are billed using this code, per lens.
V2523 Contact Lens, Hydrophilic, Extended Wear, Per Lens Soft contact lenses designed for extended wear, typically made of high-Dk materials or prescribed for overnight wear, are coded with this, per lens.
V2531 Contact Lens, GP, Scleral, Per Lens This is the crucial code for all scleral lenses, encompassing corneo-scleral, mini-scleral, and full scleral designs. It is billed per lens. Avoid using V2530, which is for gas-impermeable scleral lenses; virtually all modern scleral lenses are gas permeable to maintain corneal health. PMMA scleral lenses (gas-impermeable) are exceptionally rare and only used in very specific, unusual cases like phthisical eyes.
V2599 Other Type of Contact Lens This “miscellaneous” code is used for contact lens types not specifically listed elsewhere. Hybrid contact lenses are a prime example. It can also be utilized for custom impression-based scleral lenses like EyePrintPRO, offering an alternative to 92499 for fitting in some cases, depending on payer preferences.
V2627 Scleral Cover Shell This code pertains to scleral cover shells, distinct from scleral lenses used for vision correction.
While these codes provide a framework, remember that individual insurance companies have their own specific guidelines for claim submissions. The following case studies illustrate how to apply these codes in various clinical scenarios, considering different patient conditions and vision insurance plans, to optimize billing practices within your eye care center.
Case Study 1: Herpes Simplex Keratitis and Scleral Lens Fitting
A 58-year-old woman with a history of herpes simplex keratitis over 20 years prior presented with a corneal scar in her right eye. Her best-corrected spectacle vision in that eye was 20/80. A scleral lens was fit, improving her vision to 20/25 OD. She had vision insurance through Vision Service Plan (VSP).
The ICD-10-CM diagnosis code used was:
H17.11 central corneal opacity, right eye
For VSP claims, providing detailed lens information in box 19 is essential. In this case, we documented:
Scleral, Art Optical, Ampleye
VSP mandates pre-authorization for medically necessary contact lenses. This authorization number is then required for billing both the fitting and lens materials. We used CPT code 92313 for the fitting (corneo-scleral lens fitting, bilateral code applied to one eye in this case) and HCPCS code V2531 for the scleral lens material. Accurate diagnosis coding is paramount to prevent claim rejections.
While VSP guidelines may suggest billing the comprehensive eye exam (92004 or 92014) concurrently with the medically necessary contact lens fitting and materials, our experience indicates that billing the eye examination separately before seeking authorization for medically necessary contact lenses often reduces billing complexities and confusion. VSP’s reimbursement structure for medically necessary contact lenses typically bundles the fitting, dispensing, and associated follow-up care. Therefore, it is crucial to avoid billing the patient’s vision or medical insurance separately for any other services or products directly related to these contact lenses within the designated global period.
Case Study 2: Pellucid Marginal Degeneration and Custom Scleral Lenses
A 28-year-old male with pellucid marginal degeneration (PMD) sought consultation for custom impression-based scleral lenses (EyePrintPRO). He had previously attempted corneal GP lenses but experienced significant discomfort and lens instability.
After discussing all options, he elected to proceed with EyePrintPRO lenses. Ocular surface impressions were taken of both eyes, followed by diagnostic scleral lens fitting. Diagnostic lenses provided 20/20 vision in both eyes. The impressions and diagnostic lens data were sent to the lab for fabrication of the custom prosthetic devices. He has successfully worn these lenses for three years.
The coding utilized for this case included:
92499 Eyeprint PRO prescribing $ _________ (Note: Practices should establish their fee schedule for this code)
V2599-RT Eyeprint PRO impression and lens for right eye $_________ (Again, practice-specific fees apply)
V2599-LT Eyeprint PRO impression and lens for left eye $__________ (Practice-specific fees)
H18.463 peripheral corneal degeneration OU
Given that most insurance companies do not cover EyePrintPRO lenses, an Advanced Beneficiary Notice (ABN) is mandatory for patients choosing this option. A comprehensive written contract detailing fees, global period, and other pertinent details should also be executed with the patient before proceeding. Clear financial communication is key when offering advanced, often non-covered, specialty lens options in your eye care center.
Case Study 3: Irregular Cornea, Keratoconus, and Scleral Lens Refitting
A 42-year-old male with a history of keratoconus and prior intrastromal corneal ring segments in his left eye (2014) presented for a comprehensive eye exam and contact lens fitting. His primary complaint was discomfort with his current scleral lenses.
Examination revealed best-corrected visual acuity of 20/20 in both eyes with scleral lenses. His existing lenses were fitting tightly at the limbus, likely contributing to corneal neovascularization in the left eye.
Diagnoses included:
H52.13 myopia
H52.213 irregular astigmatism
H18.613 stable keratoconus
H16.402 corneal neovascularization
Anterior segment photography was performed to document and monitor the corneal neovascularization.
The patient desired new scleral lenses but was concerned about out-of-pocket expenses. Our office contacted his insurance to pre-verify coverage using a “Pre-Determination of Coverage” (PDC) form. This form is invaluable for staff to gather coverage details from insurance representatives and for patient communication regarding costs. It documents the representative contacted, coverage verification for procedure codes, and material coverage inquiries.
While material coverage is often denied initially, skilled staff can often clarify the medical necessity of these devices, sometimes finding coverage within durable medical equipment or “other devices” sections of the plan benefits.
The PDC form also lists potential additional tests (topography, anterior segment photography, OCT, pachymetry) and follow-up visits that may incur patient costs, promoting financial transparency.
In this case, the patient had a remaining deductible of approximately $350 and coverage for fitting and materials after deductible fulfillment.
The initial visit was coded and billed to his health insurance as:
92004 (comprehensive eye exam, new), H18.613 (keratoconus)
92015-22 (refraction, complex), H52.13 (Myopia) (The -22 modifier indicates increased complexity, requiring additional documentation)
98225 (anterior segment imaging), H16.402 (corneal neovascularization)
After insurance communication, the patient returned for lens fitting. Topography was performed, and scleral lenses were fit and designed. He paid the remaining deductible at this visit.
The subsequent claim to medical insurance included:
92072 (bilateral code) (Initial fitting of contact lenses for keratoconus), H18.613
V2531 (2 units) (scleral gas permeable contact lenses), H18.613
92025 (Corneal topography), H18.613
Follow-up visits were billed as office visits with appropriate Evaluation and Management (E&M) codes and diagnosis codes, submitted to medical insurance.
This case exemplifies straightforward insurance utilization. The PDC form promotes transparency and manages patient expectations regarding costs in your eye care center. The -22 modifier on complex refractions or procedures requiring extra time can be submitted with a letter explaining the complexity (e.g., irregular corneas) to potentially receive 150% of the contracted rate, although increased payment is not guaranteed.
Case Study 4: Post-Penetrating Keratoplasty Scleral Lens Refit and Corneal Edema
A 71-year-old woman with a history of keratoconus and corneal transplants over 20 years prior presented for a scleral lens refitting. She reported fogging vision in her left eye after a few hours of wear with her current lenses.
Examination revealed microcystic edema and corneal bullae in the left eye, despite a well-fitting scleral lens. This was attributed to endothelial cell loss in her aging corneal transplant. Instead of a new contact lens fitting, she was referred back to her corneal surgeon for endothelial transplant evaluation.
This initial visit was billed as:
Office visit, level 3
99213, Z94.7 (corneal transplant status), H18.22 (corneal edema, due to contact lens, OS)
92132 (anterior segment OCT imaging), H18.212 (corneal edema, due to contact lens, OS
Four months post-endothelial transplant surgery, she returned for scleral lens fitting. Topography was performed. As her corneal surgeon had recently performed an endothelial cell count, it was not repeated in our office, but a baseline count would have been appropriate at this stage if not recently available.
The scleral lens fitting was then billed as:
92313 (bilateral code) (fitting of contact lens, with medical supervision), Z94.7
92025 (corneal topography), Z94.7
V2531 (2 units) (scleral contact lenses), Z94.7
Similar to Case 3, office visits were billed to medical insurance until the fitting was initiated. This case underscores the importance of addressing underlying ocular health issues before proceeding with contact lens fitting. Prioritizing ocular health ensures a more successful and comfortable lens wearing experience.
Case Study 5: Bilateral Aphakia and GP Lens Fitting
A 33-year-old woman presented for a contact lens update, as her current GP lenses were three years old. She reported blurry vision, haloes at night, and reduced wearing time (12 hours due to itchiness). She had a history of congenital cataracts and cataract surgery in childhood (right eye at age 2, left eye at age 4), resulting in bilateral aphakia.
Her refraction was OD +11.75 –0.50 x 177, 20/25 DVA, 20/25 NVA and OS +11.75, Add +2.75, 20/25 DVA, 20/25 NVA. Keratometry readings were OD 45.83/46.58 @ 65 and OS 45.67/46.04 @ 125.
Overall eye health was good. Peripheral iridotomies (PIs) were patent in both eyes.
She was successfully fit with lenticulated GP lenses (Figure 2). Parameters: OD +14.00D / 7.46mm / 9.5mm, Optimum comfort (Contamac), 20/30 DVA and OS +12.00D / 7.34mm / 9.4mm, Optimum comfort, 20/30 DVA.
For billing aphakia with VSP, the codes were:
H27.03 (aphakia, both eyes)
92312 (corneal lens for aphakia – both eyes)
V2510 (contact lens, gas permeable, spherical, per lens – 2 units)
In box 19, we included:
Essilor contact lenses, spherical GP contact lenses
Figure 3 shows the coding summary for this case. Remember, thorough documentation of contact lens evaluations, fittings, and follow-ups is crucial to support billed diagnoses and prevent claim denials for Visually Necessary Contact Lenses. Payment denials can be avoided when clinical findings in the patient record substantiate the billed diagnosis.
Case Study 6: Keratoconus and Scleral Lens Fitting Under Vision Insurance
A 39-year-old woman was referred for contact lens evaluation after being deemed unsuitable for LASIK due to keratoconus. She was wearing spectacles and had unsuccessfully trialed GP and hybrid lenses previously.
Unaided visual acuity was OD CF at two feet, Pinhole 20/50 and OS CF at one foot, Pinhole 20/50. Manifest refraction: OD –6.50 –5.25 x 110, 20/50 VA and OS –7.50 –4.50 x 080, 20/40 VA. Keratometry: OD 45.19 / 54.87 @ 22 (apical 62.47D) and OS 42.18 / 56.25 @ 154 (apical 58.22D). Topography is shown in Figure 4.
Slit lamp examination revealed mild inferior corneal scarring in both eyes, otherwise healthy anterior segments. Pachymetry: OD 425 microns and OS 418 microns.
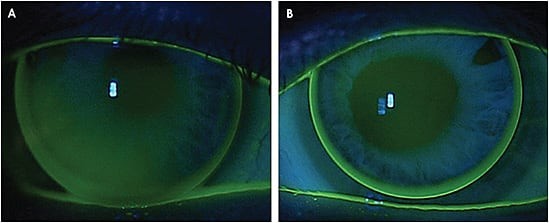
She was successfully fit with scleral lenses (Figure 5). Parameters: OD –19.75D / 6.19mm / 15.2mm, Insight scleral (Metro Optics), 20/25 DVA and OS –20.62D / 6.0mm / 15.2mm, Insight scleral (Metro Optics) 20/25 DVA.
VSP typically covers contact lenses in full for keratoconus patients eligible for materials benefits on the service date. Coverage is limited and may require specific claim handling. Examination and material copays may apply. Bill scleral lenses with HCPCS V2530 or V2531. Hybrid lenses are not considered scleral lenses by VSP and should be billed as V2599.
When billing V2530 or V2531 to VSP, box 19 must include:
Type of lens – Scleral
Scleral lens manufacturer/brand
Missing or incomplete information may result in reimbursement at the lower V2599 rate.
In this case, billing codes were (Figure 6):
92072 (fitting of contact lens for management of keratoconus, initial fitting)
H18.603 (bilateral stable keratoconus)
V2531 (scleral GP contact lens, 2 units)
Box 19 contained:
Insight scleral lens, gas permeable scleral lens, Metro Optics (laboratory)
Eyemed plans often include contact lens benefits when vision is not correctable to 20/25 in one or both eyes with standard spectacles, particularly for keratoconus. Eyemed defines two keratoconus tiers:
- Emerging/Mild: Criteria include multiple spectacle remakes, unstable topography, glare, Fleischer’s ring, Vogt’s striae, scissors reflex, no scarring, steep K < 53D, corneal thickness > 475 microns. Covered lenses include scleral, semi-scleral, and hybrid.
- Moderate/Severe: Includes all emerging/mild symptoms plus mild/no scarring or some scarring, steep K ≥ 53D, corneal thickness up to 475 microns, unmeasurable refraction. Covered lenses also include scleral, semi-scleral, and hybrid.
For this patient, the claim was filed in hard copy with a medically necessary form. Procedure code 92072AD (advanced stage) was used due to mild scarring, topographies steeper than 53D, and thin corneas. Diagnosis code H18.621 and materials code V2531 were billed.
Case Study 7: Addressing Dry Eye in Contact Lens Wearers
Happy contact lens patients are practice assets, demonstrating loyalty and referrals. However, subtle issues like reduced wearing time due to dry eye can be overlooked. Proactive questioning about comfort and wearing habits is crucial.
A 27-year-old successful soft lens wearer presented for a routine yearly exam under vision coverage. Upon questioning, she admitted to end-of-day dryness exacerbated by computer use, removing lenses earlier, and wearing spectacles more often.
Slit lamp examination revealed meibomian gland dysfunction (MGD) with obstruction. She was refitted from monthly lenses to Bausch + Lomb Biotrue Oneday daily disposables. A separate dry eye evaluation visit was scheduled, explaining that medical insurance would cover the examination, but advanced testing would have a separate fee.
Vision insurance was billed for the comprehensive exam (92014), and an annual lens supply was ordered.
Two weeks later, a dry eye evaluation was performed, including meibography, non-invasive tear breakup time, tear meniscus height, redness index, lipid layer thickness, and blink assessment. Findings were reviewed, and the chronic, progressive nature of MGD and dry eye was explained, linking it to her contact lens issues. A conservative treatment plan was outlined.
Medical insurance was billed for a level 3 office visit (99213). Advanced dry eye testing, not covered by her insurance, was billed out-of-pocket, with an ABN signed beforehand.
Treatment, ranging from omega-3 supplements to prescription products, was recommended and dispensed in-office, enhancing patient convenience, compliance, and practice revenue. Addressing dry eye proactively is essential for retaining contact lens patients and supporting overall eye health in your eye care center.
Case Study 8: Managing Dry Eye with Bandage Contact Lenses
Dry eye and MGD are increasingly prevalent, making management of moderate-to-severe cases common and challenging.
A 68-year-old longtime dry eye patient, under care for two years, was managing well with thermal pulsation for MGD, omega-3s, hypochlorous acid lid hygiene, and lubricating drops. Lipid layer thickness was marginal, but meibum expression was adequate. Tear instability and rapid breakup time with corneal staining were present. No contributing systemic health history.
ICD-10-CM codes for billing related visits:
H04.123 (dry eye syndrome-bilateral)
H02.89 (other unspecified disorders of the eyelid including MGD) (Alternatively, MGD can be coded as blepharitis H01.00x, but may require more specific eye/lid notation).
Typically, level 2 and 3 E&M codes (99212, 99213) are used for billing.
Additional dry eye testing (lid debridement, thermal pulsation) may not be covered and require ABNs and informed consent.
At a recent visit, she reported significantly worsened symptoms with discomfort and light sensitivity. Slit lamp exam showed bilateral wide vertical linear corneal staining, slightly elevated lesions resembling Thygeson’s superficial punctate keratitis (TSPK), though TSPK lesions are typically more diffuse. Upper lid examination was unremarkable. A cryopreserved amniotic membrane graft was attempted in the worse eye but discontinued due to discomfort.
For immediate relief, Alcon Dailies Total1 daily disposable lenses were fit as bandage lenses for continuous 3-day wear. Off-label use and risks were discussed and documented. Initial relief was significant. However, at follow-up, both lenses were absent, and lesions recurred, though less symptomatic. Corneal topography revealed unexpectedly flat curvatures. Lenses were changed to flatter-fitting Acuvue Oasys (Johnson & Johnson Vision). This highlighted the importance of basic fitting principles, even with bandage lenses. Bandage lenses have been effective, with the patient asymptomatic and corneal lesions resolving.
Bandage lens fitting is billed using:
92071 fitting of contact lens for treating ocular surface disease
Bandage lens use, especially with soft lenses and extended wear, carries infection risks. Off-label extended wear of daily disposables increases this risk. However, in severe cases, benefits can outweigh risks. Informed consent and emergency access address medicolegal concerns. Careful monitoring and patient education are crucial when utilizing bandage contact lenses in your eye care center.
Summary: Mastering Diagnosis Codes for Contact Lens Billing in Your Eye Care Center
Successful specialty contact lens practice relies on both fitting expertise and accurate billing and coding. This article has provided practical case studies and coding examples to guide your eye care center. By understanding diagnosis codes, CPT codes, and HCPCS codes, and implementing robust pre-determination and documentation practices, you can optimize reimbursement and ensure the financial health of your specialty lens services. Accurate coding not only maximizes revenue but also ensures compliance and reduces claim denials, allowing your practice to focus on providing excellent patient care.
Dr. Woo owns Havasu Eye Center, Parker Vision Care, and Blythe Vision Care. She is the vice president of the Scleral Lens Education Society and a GPLI Advisory Board member. She consults or advises Alcon, Blanchard, Bio-Tissue, B+L, Essilor, and X-Cel.
Dr. Messer practices in Minneapolis, focusing on specialty contact lenses in private optometry. She consults with Precilens and CooperVision.
Dr. Achong-Coan completed her residency in cornea and contact lenses at Pacific University College of Optometry and is a clinical adjunct assistant professor there. She is a Fellow of the American Academy of Optometry and the International Academy of Orthokeratology. She has consulted and researched for CooperVision and received honoraria from X-Cel.
Dr. Epstein is internationally recognized for expertise in complex contact lens management, medical contact lens complications, dry eye, and anterior segment disease. He co-founded Phoenix Eye Care and The Dry Eye Center of Arizona and directs Cornea – External Disease. Dr. Epstein also heads Ophthalmic Research Consultants of Arizona. He is a stock shareholder of NovaBay Pharmaceuticals and has received honoraria for consulting, research, speaking, and/or writing from Alcon, B+L, Bio-Tissue, Essilor, EyeEco, Oculus, PRN, NovaBay, Novartis, Sight Sciences, Shire, TearLab, and TearScience.