INTRODUCTION
Hospital-to-hospital transfers are frequently a necessity for pediatric patients who require specialized care unavailable at their initial facility. However, a significant portion of these pediatric transfers are considered potentially avoidable, representing a healthcare process burdened with unnecessary costs and safety concerns, while offering minimal benefit to patients. These Potentially Avoidable Transfers (PATs) warrant careful examination to enhance the efficiency and safety of pediatric healthcare systems. It is crucial to understand the characteristics of these transfers, especially those resulting in early discharges, to identify areas for improvement.
Studies indicate that a considerable percentage, up to 39%, of transferred pediatric patients are discharged from the receiving hospital’s emergency department or within 24 hours of admission without undergoing significant interventions. This suggests that a substantial number of transfers might be unnecessary. Nationwide data underscores the magnitude of this issue, with an estimated ~160,000 annual pediatric transfers being potentially avoidable out of over 400,000 pediatric transfers in 2012.
Pediatric PATs are not only more expensive, costing 2–3 times more than non-transfer cases, but also expose young patients to increased risks, both direct (such as transport accidents) and indirect (like psychological distress and redundant medical testing). Ambulance crashes alone result in approximately 40 fatalities annually, alongside thousands of non-fatal injuries. Reducing PATs could lead to significant resource conservation, decreased safety risks, reduced family burdens, and alleviation of physician workload. Given the high costs and risks associated with minimal benefits, addressing pediatric PATs is a critical priority in healthcare. To effectively minimize PATs, a deeper understanding of their underlying causes and characteristics is essential. A comprehensive analysis of PAT features is necessary to develop and implement targeted strategies to refine the inter-facility transfer process.
This study aims to investigate the characteristics of inter-facility transfers of pediatric patients discharged home within 24 hours. While previous research has explored pediatric transfers to emergency departments with early discharges, this study uniquely includes both emergency department arrivals and direct inpatient unit admissions. Considering direct admissions constitute a significant portion of pediatric unscheduled hospitalizations, their inclusion is vital. Furthermore, unlike prior studies that focused on specialized procedures, this research also incorporates specialized diagnoses as a criterion for necessity of transfer. Recognizing that some conditions necessitate transfer for specialized diagnosis and management, even without requiring procedures, provides a more nuanced understanding of PATs. For instance, a patient presenting with diagnosis code E871.0, Hypo-osmolality and hyponatremia, might be transferred for specialized pediatric endocrinology consultation and monitoring, even if the immediate treatment primarily involves careful observation and fluid management, leading to a discharge with self-care instructions within 24 hours if the condition stabilizes quickly.
The study seeks to characterize patient demographics, healthcare utilization patterns, referring hospital characteristics, and principal diagnoses associated with PATs. PAT is defined here as a patient transfer resulting in discharge home within 24 hours without receiving any specialized procedure or diagnosis at the receiving hospital. A key focus is comparing PAT proportions between transfers arriving through the emergency department versus those directly admitted to inpatient units. The hypothesis is that direct admissions would exhibit lower PAT proportions compared to emergency department transfers, based on the rationale that patients with questionable transfer necessity should ideally be triaged in the emergency department to prevent unnecessary inpatient bed utilization.
MATERIALS AND METHODS
Study Design and Data Source
This study employed a cross-sectional analysis of pediatric hospitalizations, utilizing electronic medical record data from a 129-bed urban university non-freestanding children’s hospital in Northern California. The dataset encompassed inpatient and emergency department records for all discharged patients over a 12-month period, from October 2015 through 2016.
Study Population
The study population included pediatric patients aged 0 to 17 years with a transfer admission source from an acute care facility. Referring locations included emergency departments and inpatient units of external hospitals. Patients could arrive at the receiving hospital’s emergency department or be directly admitted to an inpatient unit. Early discharge was defined as discharge home alive within 24 hours from either the emergency department or inpatient unit of the receiving hospital. PAT was operationally defined as an early discharge patient who did not receive any specialized procedures or diagnoses during their stay at the receiving hospital. The rationale behind this definition is that specialized procedures or diagnoses indicated the transfer’s necessity, thus classifying it as not potentially avoidable. The 24-hour early discharge criterion was informed by prior research. While acknowledging that PATs might occasionally extend beyond 24 hours, clinical experience suggests such occurrences are rare.
Variables
Specialized procedures were identified using both the International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS) codes and Epic procedure order codes. Epic codes were included to capture a more comprehensive range of procedures, potentially beyond those represented in billing data. Specialized diagnoses were captured using The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes. For patients with early discharges, ICD-10-PCS, Epic procedure order, and ICD-10-CM codes were examined. A Pediatric Hospitalist and a professional coding analyst categorized each ICD-10-PCS and Epic procedure order code as specialized, possibly specialized, or not specialized, based on definitions and lists from previous studies. ICD-10-CM diagnosis codes that would justify a transfer without necessarily involving specialized procedure codes were also identified and categorized as specialized. This categorization acknowledged that certain specialized diagnoses requiring transfer are often managed through observation rather than procedures, particularly at facilities with advanced care levels and subspecialists. For example, diagnosis code E871.0 (Hypo-osmolality and hyponatremia), while not always requiring a procedure, could necessitate transfer to a center with pediatric endocrinology expertise for appropriate diagnosis and management, especially in complex cases.
These categorizations were refined through an iterative process involving feedback from a second Pediatric Hospitalist, a Pediatric Emergency Medicine Physician, a Pediatric Critical Care Physician, and an Orthopedic Physician. Feedback focused on re-categorizing specific codes and providing rationale for re-categorization. The primary Pediatric Hospitalist and coding analyst revised categorizations based on feedback, engaging in discussions and further feedback loops until consensus was reached, and no further modifications were recommended by the physician reviewers.
Appendix I and Appendix II provide the finalized lists of specialized procedures and diagnoses, respectively, identified among transferred patients with early discharges.
Patient demographic variables included age, gender, and insurance status. Utilization variables comprised pre-transfer location (emergency department vs. inpatient unit), mode of transport, post-transfer arrival type (emergency department vs. direct admission), and post-transfer hospital location (emergency department, non-ICU, NICU, or PICU). Pre-transfer hospital characteristics included bed size and children’s hospital status (freestanding vs. non-freestanding). Principal diagnoses were identified using ICD-10-CM codes, categorized into Clinical Classifications Software diagnostic groupings.
Analysis
Descriptive statistics were performed for each variable of interest, comparing PAT and non-PAT groups. Univariate logistic regression analysis was used for categorical variables to generate p-values based on likelihood ratio tests for variation across levels. For each level, PAT proportion was calculated as the ratio of PAT transfers to total transfers. Among PAT patients, the most common ICD-10-CM Clinical Classifications Software diagnostic groupings and the top three most frequent diagnoses within these groupings were identified. A scatterplot was generated to visualize the proportion of PATs versus the total number of transfers for each referring hospital. Data analysis was conducted using STATA 13. The study received exempt approval from the University of California Davis IRB.
RESULTS
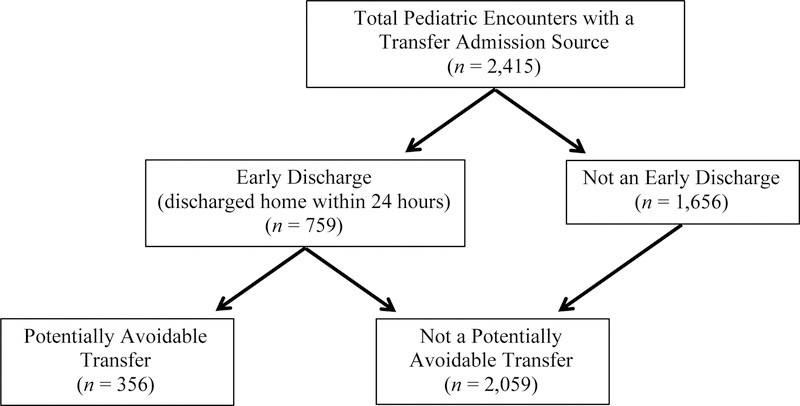
Over the 12-month study period, there were 2,415 pediatric inter-facility transfers to the study hospital from 79 referring hospitals. Of these, 1,015 (42.0%) arrived via the emergency department and 1,382 (57.2%) were direct admissions to inpatient units. Among direct admissions, 275 (19.9%) were to the NICU, 602 (43.6%) to the PICU, and 505 (36.5%) to non-ICU locations. A total of 759 transfers (31.4%) resulted in discharge home within 24 hours. Within this early discharge group, 356 patients (14.7% of all transfers) received no specialized procedure or diagnosis (Figure 1).
Figure 1: Flow diagram illustrating the categorization of transferred pediatric patients, highlighting potentially avoidable transfers (PAT) defined by early discharge and absence of specialized procedures or diagnoses at the receiving hospital.
Profile of Transferred Patients
Table 1 details patient- and hospital-level characteristics, comparing PAT and non-PAT cases. The 0–1 year age group constituted the largest number of transfers (36.5%), while the 2–5 year group had the highest number of PATs (33.4%). The 2–5 year age group also exhibited the highest PAT proportion (22.2%), whereas the 12–17 year group had the lowest (10.2%).
TABLE 1: Profile of patient- and hospital-level characteristics of transferred patients
| Potentially Avoidable Transfer (PAT) [a] (n = 356) | Non-PAT (n = 2,059) | Proportion PAT, % | P [b] | |
|---|---|---|---|---|
| Patient Characteristics | ||||
| Age group | ||||
| 0–1 years | 118 | 763 | 13.4 | |
| 2–5 years | 119 | 417 | 22.2 | |
| 6–11 years | 66 | 412 | 13.8 | |
| 12–17 years | 53 | 467 | 10.2 | |
| Gender | 0.69 | |||
| Female | 155 | 873 | 15.1 | |
| Male | 201 | 1,186 | 14.5 | |
| Insurance status | 0.36 | |||
| Private | 103 | 585 | 15.0 | |
| Public | 250 | 1,468 | 14.6 | |
| Self-pay or other | 3 | 6 | 33.3 | |
| Utilization | ||||
| Pre-transfer location | ||||
| Emergency department | 343 | 1,794 | 16.0 | |
| Inpatient unit | 13 | 265 | 4.7 | |
| Mode of transport | 0.099 | |||
| Ground | 294 | 1,646 | 15.2 | |
| Air | 53 | 384 | 12.1 | |
| Unknown | 9 | 29 | 23.7 | |
| Post-transfer arrival type | ||||
| Emergency department | 97 | 918 | 9.6 | |
| Direct admission | 256 | 1,126 | 18.5 | |
| Unknown | 3 | 15 | 16.7 | |
| Post-transfer arrival location | ||||
| Emergency department | 97 | 918 | 9.6 | |
| Non-ICU | 138 | 367 | 27.3 | |
| NICU | 14 | 261 | 5.1 | |
| PICU | 104 | 498 | 17.3 | |
| Unknown | 3 | 15 | 16.7 | |
| Pre-Transfer Hospital Characteristics | ||||
| Bed size | 0.004 | |||
| 0–150 | 119 | 609 | 16.3 | |
| 151–300 | 90 | 694 | 11.5 | |
| 301 or more | 147 | 740 | 16.6 | |
| Unknown | 0 | 16 | 0.0 | |
| Children’s hospital | 0.042 | |||
| Freestanding children’s | 2 | 1 | 66.7 | |
| Non-freestanding children’s | 354 | 2,048 | 14.7 | |
| Unknown | 0 | 10 | 0.0 |
[a] PAT defined as a patient transfer with a discharge home within 24 hours without receiving any specialized procedure or diagnosis.
[b] P-values refer to comparisons between PAT and non-PAT, determined by univariate logistic regression analysis.
Patients transferred from emergency departments were 3.4 times more likely to be categorized as PAT compared to those from inpatient units. Direct admissions were 1.9 times more frequently categorized as PAT than emergency department arrivals. Among direct admissions, PAT proportions were 5.1% for NICU, 17.3% for PICU, and 27.3% for non-ICU locations.
Table 2 presents the most common discharge diagnostic groupings for PAT cases. Respiratory infections, asthma, and ill-defined conditions were the most frequent PAT diagnoses. Respiratory infections and asthma together accounted for 34.6% of all PAT diagnoses. Notably, within the “Fluid and electrolyte disorders” diagnostic grouping, diagnosis code E871.0, Hypo-osmolality and hyponatremia, was listed, demonstrating that even specific conditions like hyponatremia can sometimes lead to potentially avoidable transfers followed by early discharge and home self-care.
TABLE 2: Most common principal diagnosis ICD-10 codes for the most common diagnostic groupings among potentially avoidable transfers
| Diagnostic Grouping (n) | ICD-10-CM code, description (n) |
|---|---|
| Respiratory infections (n = 70) | 1) J05.0, Acute obstructive laryngitis [croup] (n = 19) |
| 2) J21.9, Acute bronchiolitis, unspecified (n = 17) | |
| 3) J06.9, Acute upper respiratory infection, unspecified (n = 14) | |
| 4) J18.9, Pneumonia, unspecified organism (n = 10) [a] | |
| Asthma (n = 53) | 1) J45.901, Unspecified asthma with (acute) exacerbation (n = 21) |
| 2) J45.902, Unspecified asthma with status asthmaticus (n = 14) | |
| 3) J45.31, Mild persistent asthma with (acute) exacerbation (n = 6) | |
| Symptoms; signs; and ill-defined conditions (n = 28) | 1) R50.9, Fever, unspecified (n = 4) |
| 1) R10.31, Right lower quadrant pain (n = 4) | |
| 3) I88.0, Nonspecific mesenteric lymphadenitis (n = 3) | |
| 3) R10.9, Unspecified abdominal pain (n = 3) | |
| 3) R11.2, Nausea with vomiting, unspecified (n = 3) | |
| Epilepsy, convulsions (n = 24) | 1) R56.01, Complex febrile convulsions (n = 6) |
| 2) G40.909, Epilepsy, unspecified, not intractable, without status epilepticus (n = 5) | |
| 3) G40.901, Epilepsy, unspecified, not intractable, with status epilepticus (n = 4) | |
| 3) R56.9, Unspecified convulsions (n = 4) | |
| Fractures (n = 22) | 1) S52.531A, Colles’ fracture of right radius (n = 2) |
| Intracranial injury (n = 19) | 1) S06.0X0A, Concussion without loss of consciousness (n = 10) |
| 2) S06.0X1A, Concussion with loss of consciousness of 30 minutes or less (n = 4) | |
| 3) S06.0X9A, Concussion with loss of consciousness of unspecified duration (n = 2) | |
| Other perinatal conditions (n = 18) | 1) R68.13, Apparent life threatening event in infant (ALTE) (n = 7) |
| 2) P78.83, Newborn esophageal reflux (n = 2) | |
| 2) P92.09, Other vomiting of newborn (n = 2) | |
| Intestinal infection (n = 16) | 1) A08.4, Viral intestinal infection, unspecified (n = 12) |
| 2) A09, Infectious gastroenteritis and colitis, unspecified (n = 3) | |
| Fluid and electrolyte disorders (n = 12) | 1) E860, Dehydration (n = 8) |
| 2) E871, Hypo-osmolality and hyponatremia (n = 2) | |
| Skin and subcutaneous infections (n = 9) | 1) L03.115, Cellulitis of right lower limb (n = 2) |
| 1) L02.31, Cutaneous abscess of buttock (n = 2) |
[a] Pneumonia (J18.9) included as it was among the top 10 most common individual ICD-10-CM diagnoses.
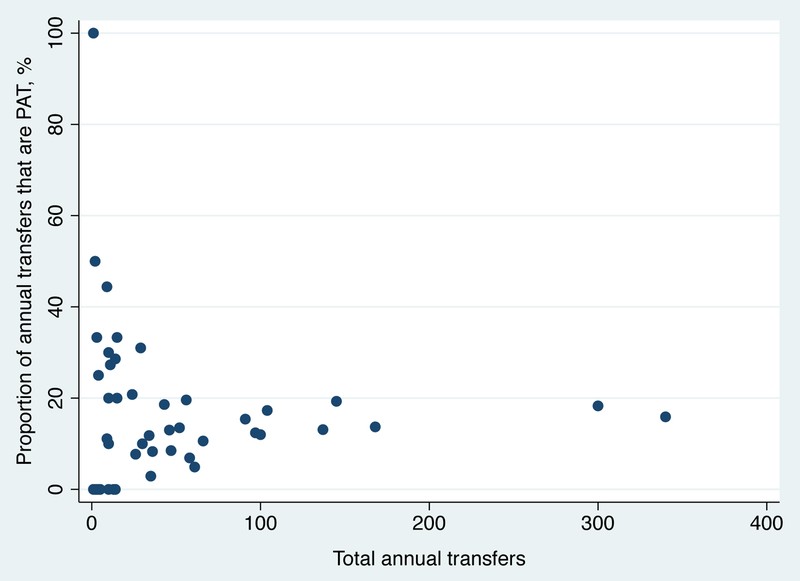
Figure 2 shows a scatterplot of PAT proportion and total transfers per hospital. It indicates no strong correlation between transfer volume and PAT proportion. Hospitals with low transfer volumes showed extreme PAT variations due to chance. For hospitals with over 75 transfers, PAT proportions generally ranged from 10–20%.
Figure 2: Scatterplot illustrating the relationship between potentially avoidable transfers (PAT) proportion and total transfers across different referring hospitals, indicating no strong correlation between transfer volume and PAT rate.
DISCUSSION
This study revealed that 31% of pediatric inter-facility transfers resulted in discharge within 24 hours, and 15% were classified as potentially avoidable, defined by early discharge and absence of specialized procedures or diagnoses. A key strength of this study lies in its comprehensive PAT definition, incorporating both specialized procedures and diagnoses. Furthermore, it uniquely analyzed both emergency department arrivals and direct inpatient admissions, highlighting the significance of direct admissions, which comprised over half of the transfers in this study. The finding that direct admissions were 1.9 times more likely to be PAT than emergency department arrivals suggests potential areas for improvement in triage and decision-making for direct admissions.
Previous studies, which primarily focused on specialized procedures and emergency department transfers, reported higher PAT frequencies (20% to 39%). The lower PAT rate in this study (15%) may be attributed to a more conservative PAT definition that includes specialized diagnoses. By considering specialized diagnoses, such as diagnosis code E871.0 (Hypo-osmolality and hyponatremia), which might require specialized pediatric endocrine expertise for management without necessarily involving procedures, this study provides a more refined and potentially more accurate estimate of PAT prevalence. Prior studies might have overestimated PAT rates by not accounting for these diagnostically driven necessary transfers.
Establishing a consistent and validated definition for PAT is crucial for future research, enabling cross-study comparisons and providing a practical, cost-effective metric for assessing interventions and hospital performance using electronic medical record data.
National data indicates that 25% of all non-elective pediatric hospitalizations are direct admissions. In this study, direct admissions constituted 57% of transfers, suggesting that inter-facility transfers are more frequently direct admissions compared to non-transfer hospitalizations. This might reflect a practice of directly admitting transferred patients to expedite care and bypass emergency department congestion, especially when referring hospitals seek specialist pediatric care.
However, the study’s finding that PATs were more common among direct admissions than emergency department arrivals raises concerns about triage and admission appropriateness for direct transfers. This aligns with nationwide perceptions among pediatric physicians about challenges in determining appropriate direct admissions. A potential solution may involve directing more transferred patients to the emergency department for triage to prevent unnecessary inpatient bed utilization. Further research comparing outcomes of PAT direct admissions versus PAT emergency department arrivals is needed to determine optimal system designs.
The 27% PAT rate among non-ICU direct admissions is particularly noteworthy, suggesting that quality improvement efforts should prioritize non-ICU transfers. However, the 17% PAT rate in PICU direct admissions also warrants attention, indicating that even critical care transfers are not immune to potential avoidability. Given the single-center nature of this study, multi-center studies are needed to confirm if these PAT patterns are consistent across different hospitals and regions.
Respiratory infections were identified as the most common diagnoses among PATs, which is consistent with their prevalence as common transfer diagnoses. The increasing concentration of pediatric hospital care, even for common conditions, might contribute to PATs as referral centers are increasingly utilized for conditions previously managed at local hospitals. For conditions like bronchiolitis and asthma, interventions to reduce PATs should focus on empowering referring hospitals with resources to manage these common conditions definitively, potentially through telemedicine.
Telemedicine has demonstrated potential to reduce transfer rates by up to 50% by providing specialist consultation and identifying patients who do not require transfer. Telemedicine offers advantages over standard telephone consultations by enabling virtual face-to-face assessments and enhancing care quality, family-centeredness, and accessibility. Referring physicians also perceive telemedicine consultations as educational and anxiety-reducing in managing acute pediatric cases. For instance, in cases presenting with potential diagnosis code E871.0 (Hypo-osmolality and hyponatremia), telemedicine consultations with pediatric endocrinologists could help referring physicians determine if transfer is truly necessary or if initial management and monitoring can be effectively initiated at the local hospital, potentially avoiding a PAT.
This study has limitations, including generalizability due to its single-center design. Transfer practices are likely influenced by hospital-specific agreements. Lack of pre-transfer hospital medical records limits the depth of PAT categorization. Furthermore, the study does not capture the treating physicians’ decision-making processes behind transfers. The PAT definition, while refined through an iterative physician review process and based on prior literature, has not been formally validated.
CONCLUSION
Pediatric PATs constitute a significant proportion of inter-facility transfers, occurring in over 1 in 7 cases. PAT rates are higher among direct admissions and non-critically ill patients. Further research is essential to examine PAT outcomes and develop strategies to improve inter-facility transfer practices, potentially focusing on optimizing direct admission pathways, enhancing triage processes, and leveraging telemedicine to support referring hospitals in managing common pediatric conditions, thus reducing potentially avoidable transfers and improving the overall efficiency and safety of pediatric healthcare.
Acknowledgments
Source of Funding: This research was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1TR001860 and linked award KL2TR001859. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
APPENDIX I: Specialized Procedures
Specialized procedures received among pediatric patients with a transfer admission source and an early discharge.
| ICD-10-PCS Procedure Code | ICD-10-PCS Procedure Name |
|---|---|
| 009U3ZX | Drainage of Spinal Canal, Percutaneous Approach, Diagnostic |
| 009U3ZZ | Drainage of Spinal Canal, Percutaneous Approach |
| 00B20ZZ | Excision of Dura Mater, Open Approach |
| 00U20JZ | Supplement Dura Mater with Synth Sub, Open Approach |
| 01Q30ZZ | Repair Brachial Plexus, Open Approach |
| 02583ZZ | Destruction of Conduction Mechanism, Percutaneous Approach |
| 02HV33Z | Insertion of Infusion Dev into Sup Vena Cava, Perc Approach |
| 02K83ZZ | Map Conduction Mechanism, Percutaneous Approach |
| 03LB0ZZ | Occlusion of Right Radial Artery, Open Approach |
| 03Q80ZZ | Repair Left Brachial Artery, Open Approach |
| 03QC0ZZ | Repair Left Radial Artery, Open Approach |
| 04L20ZZ | Occlusion of Gastric Artery, Open Approach |
| 05BC0ZZ | Excision of Left Basilic Vein, Open Approach |
| 05SC0ZZ | Reposition Left Basilic Vein, Open Approach |
| 06H033Z | Insertion of Infusion Dev into Inf Vena Cava, Perc Approach |
| 06L20ZZ | Occlusion of Gastric Vein, Open Approach |
| 07BB4ZX | Excision of Mesenteric Lymphatic, Perc Endo Approach, Diagn |
| 087X0DZ | Dilation of R Lacrml Duct with Intralum Dev, Open Approach |
| 087Y7DZ | Dilation of L Lacrml Duct with Intralum Dev, Via Opening |
| 08NQ0ZZ | Release Right Lower Eyelid, Open Approach |
| 08Q1XZZ | Repair Left Eye, External Approach |
| 08Q33ZZ | Repair Left Anterior Chamber, Percutaneous Approach |
| 08QN0ZZ | Repair Right Upper Eyelid, Open Approach |
| 08QNXZZ | Repair Right Upper Eyelid, External Approach |
| 08QPXZZ | Repair Left Upper Eyelid, External Approach |
| 08QQ0ZZ | Repair Right Lower Eyelid, Open Approach |
| 08QQXZZ | Repair Right Lower Eyelid, External Approach |
| 08QR0ZZ | Repair Left Lower Eyelid, Open Approach |
| 08QRXZZ | Repair Left Lower Eyelid, External Approach |
| 08QY0ZZ | Repair Left Lacrimal Duct, Open Approach |
| 09BQ4ZX | Excision of Right Maxillary Sinus, Perc Endo Approach, Diagn |
| 09BQ4ZZ | Excision of Right Maxillary Sinus, Perc Endo Approach |
| 0BC38ZZ | Extirpation of Matter from Right Main Bronchus, Endo |
| 0BC78ZZ | Extirpation of Matter from Left Main Bronchus, Endo |
| 0BH18EZ | Insertion of Endotracheal Airway into Trachea, Endo |
| 0BJ08ZZ | Inspection of Tracheobronchial Tree, Endo |
| 0C5Q0ZZ | Destruction of Adenoids, Open Approach |
| 0C7S8ZZ | Dilation of Larynx, Endo |
| 0C950ZZ | Drainage of Upper Gingiva, Open Approach |
| 0C9P0ZZ | Drainage of Tonsils, Open Approach |
| 0CBP0ZZ | Excision of Tonsils, Open Approach |
| 0CJS8ZZ | Inspection of Larynx, Endo |
| 0CJY8ZZ | Inspection of Mouth and Throat, Endo |
| 0CQ30ZZ | Repair Soft Palate, Open Approach |
| 0D774ZZ | Dilation of Stomach, Pylorus, Perc Endo Approach |
| 0D874ZZ | Division of Stomach, Pylorus, Perc Endo Approach |
| 0D878ZZ | Division of Stomach, Pylorus, Endo |
| 0D9W4ZZ | Drainage of Peritoneum, Percutaneous Endoscopic Approach |
| 0DB58ZX | Excision of Esophagus, Endo, Diagn |
| 0DB68ZX | Excision of Stomach, Endo, Diagn |
| 0DB98ZX | Excision of Duodenum, Endo, Diagn |
| 0DBH4ZX | Excision of Cecum, Percutaneous Endoscopic Approach, Diagn |
| 0DC18ZZ | Extirpation of Matter from Upper Esophagus, Endo |
| 0DC38ZZ | Extirpation of Matter from Lower Esophagus, Endo |
| 0DC58ZZ | Extirpation of Matter from Esophagus, Endo |
| 0DC68ZZ | Extirpation of Matter from Stomach, Endo |
| 0DCK8ZZ | Extirpation of Matter from Ascending Colon, Endo |
| 0DH63UZ | Insertion of Feeding Device into Stomach, Perc Approach |
| 0DJ08ZZ | Inspection of Upper Intestinal Tract, Endo |
| 0DSB7ZZ | Reposition Ileum, Via Natural or Artificial Opening |
| 0DSL7ZZ | Reposition Transverse Colon, Via Opening |
| 0DSPXZZ | Reposition Rectum, External Approach |
| 0DTJ0ZZ | Resection of Appendix, Open Approach |
| 0DTJ4ZZ | Resection of Appendix, Percutaneous Endoscopic Approach |
| 0DTJ8ZZ | Resection of Appendix, Endo |
| 0F798ZZ | Dilation of Common Bile Duct, Endo |
| 0F998ZZ | Drainage of Common Bile Duct, Endo |
| 0H89XZZ | Division of Perineum Skin, External Approach |
| 0J9L3ZZ | Drainage of R Up Leg Subcu/Fascia, Perc Approach |
| 0JBC0ZZ | Excision of Pelvic Subcu/Fascia, Open Approach |
| 0JQ10ZZ | Repair Face Subcutaneous Tissue and Fascia, Open Approach |
| 0JQG0ZZ | Repair R Low Arm Subcu/Fascia, Open Approach |
| 0JQH0ZZ | Repair L Low Arm Subcu/Fascia, Open Approach |
| 0JQJ3ZZ | Repair R Hand Subcu/Fascia, Perc Approach |
| 0JWS0JZ | Revise Synth Sub in Head & Neck Subcu/Fascia, Open |
| 0KQ10ZZ | Repair Facial Muscle, Open Approach |
| 0KQ80ZZ | Repair Left Upper Arm Muscle, Open Approach |
| 0LB40ZZ | Excision of Left Upper Arm Tendon, Open Approach |
| 0LQ40ZZ | Repair Left Upper Arm Tendon, Open Approach |
| 0MBN0ZZ | Excision of Right Knee Bursa and Ligament, Open Approach |
| 0NHS04Z | Insertion of Int Fix into L Maxilla, Open Approach |
| 0NHV04Z | Insertion of Int Fix into L Mandible, Open Approach |
| 0NSM04Z | Reposition Right Zygomatic Bone with Int Fix, Open Approach |
| 0NSP04Z | Reposition Right Orbit with Int Fix, Open Approach |
| 0NST04Z | Reposition Right Mandible with Int Fix, Open Approach |
| 0NSV04Z | Reposition Left Mandible with Int Fix, Open Approach |
| 0PCH0ZZ | Extirpation of Matter from Right Radius, Open Approach |
| 0PSC04Z | Reposition Right Humeral Head with Int Fix, Open Approach |
| 0PSC34Z | Reposition Right Humeral Head with Int Fix, Perc Approach |
| 0PSD04Z | Reposition Left Humeral Head with Int Fix, Open Approach |
| 0PSD34Z | Reposition Left Humeral Head with Int Fix, Perc Approach |
| 0PSD44Z | Reposition L Humeral Head with Int Fix, Perc Endo Approach |
| 0PSF04Z | Reposition Right Humeral Shaft with Int Fix, Open Approach |
| 0PSF34Z | Reposition Right Humeral Shaft with Int Fix, Perc Approach |
| 0PSF35Z | Reposition Right Humeral Shaft with Ext Fix, Perc Approach |
| 0PSF44Z | Reposition R Humeral Shaft with Int Fix, Perc Endo Approach |
| 0PSG04Z | Reposition Left Humeral Shaft with Int Fix, Open Approach |
| 0PSG06Z | Reposition L Humeral Shaft with Intramed Fix, Open Approach |
| 0PSG34Z | Reposition Left Humeral Shaft with Int Fix, Perc Approach |
| 0PSG35Z | Reposition Left Humeral Shaft with Ext Fix, Perc Approach |
| 0PSH04Z | Reposition Right Radius with Int Fix, Open Approach |
| 0PSH06Z | Reposition Right Radius with Intramed Fix, Open Approach |
| 0PSH34Z | Reposition Right Radius with Int Fix, Perc Approach |
| 0PSH36Z | Reposition Right Radius with Intramed Fix, Perc Approach |
| 0PSJ04Z | Reposition Left Radius with Int Fix, Open Approach |
| 0PSJ06Z | Reposition Left Radius with Intramed Fix, Open Approach |
| 0PSJ34Z | Reposition Left Radius with Int Fix, Perc Approach |
| 0PSJ3ZZ | Reposition Left Radius, Percutaneous Approach |
| 0PSK04Z | Reposition Right Ulna with Int Fix, Open Approach |
| 0PSK06Z | Reposition Right Ulna with Intramed Fix, Open Approach |
| 0PSK36Z | Reposition Right Ulna with Intramed Fix, Perc Approach |
| 0PSL06Z | Reposition Left Ulna with Intramed Fix, Open Approach |
| 0QH634Z | Insertion of Int Fix into R Up Femur, Perc Approach |
| 0QS734Z | Reposition Left Upper Femur with Int Fix, Perc Approach |
| 0QS806Z | Reposition R Femur Shaft with Intramed Fix, Open Approach |
| 0QS904Z | Reposition Left Femoral Shaft with Int Fix, Open Approach |
| 0QS906Z | Reposition L Femur Shaft with Intramed Fix, Open Approach |
| 0QS93ZZ | Reposition Left Femoral Shaft, Percutaneous Approach |
| 0QSG34Z | Reposition Right Tibia with Int Fix, Perc Approach |
| 0QSH04Z | Reposition Left Tibia with Int Fix, Open Approach |
| 0RSL04Z | Reposition Right Elbow Joint with Int Fix, Open Approach |
| 0RSM34Z | Reposition Left Elbow Joint with Int Fix, Perc Approach |
| 0RSV0ZZ | Reposition Left Metacarpophalangeal Joint, Open Approach |
| 0SSF04Z | Reposition Right Ankle Joint with Int Fix, Open Approach |
| 0TJD8ZZ | Inspection of Urethra, Endo |
| 0U9K7ZZ | Drainage of Hymen, Via Natural or Artificial Opening |
| 0VJ80ZZ | Inspection of Scrotum and Tunica Vaginalis, Open Approach |
| 0VQS0ZZ | Repair Penis, Open Approach |
| 0VS90ZZ | Reposition Right Testis, Open Approach |
| 0VSB0ZZ | Reposition Left Testis, Open Approach |
| 0VSC0ZZ | Reposition Bilateral Testes, Open Approach |
| 0VT90ZZ | Resection of Right Testis, Open Approach |
| 0VTB0ZZ | Resection of Left Testis, Open Approach |
| 0W3P7ZZ | Control Bleeding in Gastrointestinal Tract, Via Opening |
| 0WJP4ZZ | Inspection of Gastrointestinal Tract, Perc Endo Approach |
| 0WQ20ZZ | Repair Face, Open Approach |
| 0WQF0ZZ | Repair Abdominal Wall, Open Approach |
| 0WQF4ZZ | Repair Abdominal Wall, Percutaneous Endoscopic Approach |
| 0WQNXZZ | Repair Female Perineum, External Approach |
| 0YJ64ZZ | Inspection of Left Inguinal Region, Perc Endo Approach |
| 0YQ50ZZ | Repair Right Inguinal Region, Open Approach |
| 0YQ54ZZ | Repair Right Inguinal Region, Perc Endo Approach |
| 3E04305 | Introduce Oth Antineoplastic in Central Vein, Perc |
| 3E0R3TZ | Introduction of Destr Agent into Spinal Canal, Perc Approach |
| 3E0S3GC | Introduce Oth Therap Subst in Epidural Space, Perc |
| 3E1M39Z | Irrigation of Periton Cav using Dialysate, Perc Approach |
| 4A00X4Z | Measure of Central Nervous Electr Activity, Extern Approach |
| 4A133R1 | Monitoring of Arterial Saturation, Peripheral, Perc Approach |
| 5A09357 | Assistance with Respiratory Ventilation, |
| 5A0935Z | Assistance with Respiratory Ventilation, |
| 5A15223 | Extracorporeal Membrane Oxygenation, Continuous |
| 5A1935Z | Respiratory Ventilation, Less than 24 Consecutive Hours |
| 5A1945Z | Respiratory Ventilation, 24–96 Consecutive Hours |
| 6A4Z0ZZ | Hypothermia, Single |
| B030Y0Z | MRI of Brain using Oth Contrast, Unenh, Enhance |
| B030YZZ | Magnetic Resonance Imaging (MRI) of Brain using Oth Contrast |
| B030ZZZ | Magnetic Resonance Imaging (MRI) of Brain |
| B03BYZZ | MRI of Spinal Cord using Oth Contrast |
| B03BZZZ | Magnetic Resonance Imaging (MRI) of Spinal Cord |
| B246ZZZ | Ultrasonography of Right and Left Heart |
| B24DZZZ | Ultrasonography of Pediatric Heart |
| B31H1ZZ | Fluoroscopy of R Up Extrem Art using L Osm Contrast |
| BD11YZZ | Fluoroscopy of Esophagus using Other Contrast |
| BD13ZZZ | Fluoroscopy of Small Bowel |
| BF111ZZ | Fluoroscopy of Bili/Pancr Duct using L Osm Contrast |
| BP1AZZZ | Fluoroscopy of Right Humerus |
| BP1H1ZZ | Fluoroscopy of Left Elbow using Low Osmolar Contrast |
| BP39ZZZ | Magnetic Resonance Imaging (MRI) of Left Shoulder |
| BQ13ZZZ | Fluoroscopy of Right Femur |
| BQ1DZZZ | Fluoroscopy of Right Lower Leg |
| BQ33YZZ | MRI of R Femur using Oth Contrast |
| BQ3DY0Z | MRI of R Low Leg using Oth Contrast, Unenh, Enhance |
| BR30YZZ | MRI of Cerv Spine using Oth Contrast |
| BR30ZZZ | Magnetic Resonance Imaging (MRI) of Cervical Spine |
| BR39YZZ | MRI of Lumbar Spine using Oth Contrast |
| BT1D1ZZ | Fluoroscopy Kidney, Ureter, Bladder, R w L Osm Contrast |
| BW38ZZZ | Magnetic Resonance Imaging (MRI) of Head |
| CD171ZZ | Planar Nucl Med Imag of GI Tract using Technetium 99m |
| Epic Procedure Order Code | Epic Procedure Order Name |
|---|---|
| AMBREF0201 | PEDIATRIC PULMONARY REFERRAL |
| APHER000001 | THERAPEUTIC PLASMA EXCHANGE |
| BBKBB00005 | ABO/RH BLOOD TYPE |
| BBKBB00040 | BLOOD TYPE VERIFICATION |
| BBKBB00057 | DIRECT COOMBS TEST (POLY) |
| BBKBB00058 | DIRECT COOMBS TEST/IGG |
| BBKBB00086 | TYPE AND SCREEN |
| BBKBP00002 | FRESH FROZEN PLASMA |
| BBKBP00004 | RED BLOOD CELLS |
| BBKBP00006 | PLATELETPHERESIS |
| BBKBP00008 | RED BLOOD CELLS PEDI/NEONATE |
| CARD00023 | PEDIATRIC ECHOCARDIOGRAM COMPLETE |
| CARD00048 | PEDS ELECTROPHYSIOLOGY STUDY/ABLATION |
| NEURO00002 | ROUTINE ELECTROENCEPHALOGRAM |
| NEURO00003 | CONTINUOUS ELECTROENCEPHALOGRAM |
| NEURO00010 | EEG ELECTROENCEPHALOGRAM, ROUTINE |
| PCORESP00010 | EXTUBATE |
| PTHSP00001 | SURGICAL PATHOLOGY |
| RADCT00905 | CT PELVIS WITHOUT CONTRAST |
| RADCT00910 | CT ANGIO LOWER EXTREMITY |
| RADCT00911 | CT ANGIO UPPER EXTREMITY |
| RADCT00912 | CT LOWER EXTREMITY WITHOUT CONTRAST |
| RADCT00913 | CT UPPER EXTREMITY WITHOUT CONTRAST |
| RADCT00921 | CT CHEST WITH CONTRAST |
| RADCT00923 | CT ANGIO HEAD |
| RADCT00924 | CT ANGIO NECK |
| RADCT00925 | CT SINUS / FACIAL WITHOUT CONTRAST |
| RADCT00926 | CT SINUS / FACIAL WITH CONTRAST |
| RADCT00928 | CT C-SPINE WITHOUT CONTRAST |
| RADCT00931 | CT HEAD WITHOUT CONTRAST |
| RADCT00932 | CT HEAD WITH CONTRAST |
| RADCT00934 | CT L-SPINE WITHOUT CONTRAST |
| RADCT00938 | CT NECK WITH CONTRAST |
| RADCT00943 | CT T-SPINE WITHOUT CONTRAST |
| RADCT00955 | CT ABDOMEN + PELVIS WITH CONTRAST |
| RADCT00967 | CT 3-D RECONSTRUCTION |
| RADCT00989 | CT TEMPORAL BONES WITH CONTRAST |
| RADCT01030 | CT ABDOMEN + PELVIS UROGRAM |
| RADCT01048 | CT L-SPINE (2D RECONS L-SPINE FROM ABD/PELVIS) |
| RADCT01049 | CT T-SPINE (2D RECONS T-SPINE FROM CHEST) |
| RADCT01052 | 2DRECON TRAUMA C-SPINE (ED/RAD ONLY) |
| RADDX01051 | FLUOROSCOPY 60+ MINUTES WITHOUT RADIOLOGIST |
| RADDX01052 | FLUOROSCOPY UNDER 60 MINUTES WITHOUT RADIOLOGIST |
| RADDX01066 | BONE SURVEY, >12 MONTHS OLD, COMPLETE |
| RADDX01074 | BARIUM ENEMA |
| RADDX01075 | BARIUM ENEMA WITH AIR |
| RADDX01079 | ESOPHOGRAM |
| RADDX01086 | UPPER GI SINGLE CONTRAST |
| RADDX01089 | DX IVP PEDIATRIC |
| RADDX01093 | BONE SURVEY, |
| RADIR01177 | IR JEJUNOSTOMY TUBE CHANGE |
| RADMR00901 | MR ABDOMEN WITHOUT CONTRAST |
| RADMR00905 | MR PELVIS WO CONTRAST |
| RADMR00909 | MR ANGIO UPPER EXTREMITY, WITH OR WITHOUT CONTRAST |
| RADMR00934 | MR BRAIN WITHOUT CONTRAST |
| RADMR00936 | MR BRAIN WITH / WITHOUT CONTRAST |
| RADMR00937 | MR C-SPINE WITHOUT CONTRAST |
| RADMR00940 | MR L-SPINE WITHOUT CONTRAST |
| RADMR00946 | MR T-SPINE WITHOUT CONTRAST |
| RADMR00958 | MR BRAIN + MR ANGIO BRAIN + MR ANGIO NECK |
| RADMR00960 | MR C-SPINE + MR T-SPINE + MR L-SPINE |
| RADMR00962 | MR BRAIN + MR ANGIO BRAIN |
| RADMR00963 | MR BRAIN WITH AND WITHOUT CONTRAST + MR ANGIO BRAIN |
| RADMR00981 | MR SPECTROSCOPY BRAIN |
| RADMR01022 | MR UPPER EXTREMITY JOINT, LEFT WITHOUT CONTRAST |
| RADMR01033 | MR LOWER EXTREMITY JOINT, RIGHT WITH CONTRAST |
| RADMR01037 | MR LOWER EXTREMITY, RIGHT WITH / WITHOUT CONTRAST |
| RADMR01048 | MR FETAL |
| RADNM00935 | NM BOWEL IMAGING (MECKELS) |
| RT00017 | HIGH FLOW NASAL CANULA |
| SLEEP00001 | SLEEP STUDY |
APPENDIX II: Specialized Diagnoses
Specialized diagnoses among pediatric patients with a transfer admission source and an early discharge.
| Diagnostic grouping | ICD-10-CM Diagnosis Code | ICD-10-CM Diagnosis Name |
|---|---|---|
| Alcohol-related disorders | F10.129 | Alcohol abuse with intoxication, unspecified |
| Anemia | D57.00 | Hb-SS disease with crisis, unspecified |
| D61.818 | Other pancytopenia | |
| Bacterial infection | A41.9 | Sepsis, unspecified organism |
| Burns | T20.26XA | Burn of second degree of forehead and cheek, init encntr |
| T21.25XA | Burn of second degree of buttock, initial encounter | |
| T26.41XA | Burn of right eye and adnexa, part unspecified, init encntr | |
| T27.1XXA | Burn involving larynx and trachea with lung, init encntr | |
| T31.11 | Burns of 10–19% of body surface w 10–19% third degree burns | |
| Central nervous system infection | A87.8 | Other viral meningitis |
| Cerebrovascular disease | G45.9 | Transient cerebral ischemic attack, unspecified |
| Coagulation and hemorrhagic disorders | D65 | Disseminated intravascular coagulation |
| Coma; stupor; and brain damage | R40.243 | Glasgow coma scale score 3–8 |
| Complications | G97.1 | Other reaction to spinal and lumbar puncture |
| K94.22 | Gastrostomy infection | |
| K94.23 | Gastrostomy malfunction | |
| T85.09XA | Mech compl of ventricular intracranial shunt, init | |
| T88.3XXA | Malignant hyperthermia due to anesthesia, initial encounter | |
| T88.6XXA | Anaphyl reaction due to advrs eff drug/med prop admin, init | |
| Complications mainly related to pregnancy | O14.93 | Unspecified pre-eclampsia, third trimester |
| Crushing injury or internal injury | S27.0XXA | Traumatic pneumothorax, initial encounter |
| S36.114A | Minor laceration of liver, initial encounter | |
| S37.042A | Minor laceration of left kidney, initial encounter | |
| S37.061A | Major laceration of right kidney, initial encounter | |
| Diabetes mellitus with complications | E101.0 | Type 1 diabetes mellitus with ketoacidosis without coma |
| E106.49 | Type 1 diabetes mellitus with hypoglycemia without coma | |
| E131.0 | Oth diabetes mellitus with ketoacidosis without coma | |
| Digestive congenital anomalies | Q40.0 | Congenital hypertrophic pyloric stenosis |
| Diseases of male genital organs | N44.00 | Torsion of testis, unspecified |
| Diseases of the heart | I46.9 | Cardiac arrest, cause unspecified |
| I47.2 | Ventricular tachycardia | |
| Diseases of the urinary system | N01.9 | Rapidly progr nephritic syndrome w unsp morphologic changes |
| N04.1 | Nephrotic syndrome w focal and segmental glomerular lesions | |
| N12 | Tubulo-interstitial nephritis, not spcf as acute or chronic | |
| N17.9 | Acute kidney failure, unspecified | |
| Epilepsy; convulsions | G40.501 | Epileptic seiz rel to extrn causes, not ntrct, w stat epi |
| G40.901 | Epilepsy, unsp, not intractable, with status epilepticus | |
| G40.911 | Epilepsy, unspecified, intractable, with status epilepticus | |
| R56.01 | Complex febrile convulsions | |
| Factors influencing health care | Z03.6 | Encntr for obs for susp toxic eff from ingest sub ruled out |
| Fractures | S02.0XXA | Fracture of vault of skull, init encntr for closed fracture |
| S02.119A | Unsp fracture of occiput, init encntr for closed fracture | |
| S02.19XA | Oth fracture of base of skull, init for clos fx | |
| S02.3XXA | Fracture of orbital floor, init encntr for closed fracture | |
| S72.332A | Displaced oblique fracture of shaft of left femur, init | |
| S72.342A | Displaced spiral fracture of shaft of left femur, init | |
| Gastrointestinal hemorrhage | K92.0 | Hematemesis |
| K92.1 | Melena | |
| K92.2 | Gastrointestinal hemorrhage, unspecified | |
| Intracranial injury | S06.1X9A | Traumatic cerebral edema w LOC of unsp duration, init |
| S06.2X7A | Diffuse TBI w LOC w death due to brain injury bf consc, init | |
| S06.4X0A | Epidural hemorrhage w/o loss of consciousness, init encntr | |
| S06.4X9A | Epidural hemorrhage w LOC of unsp duration, init | |
| S06.5X0A | Traum subdr hem w/o loss of consciousness, init | |
| S06.5X1A | Traum subdr hem w LOC of 30 minutes or less, init | |
| S06.6X0A | Traum subrac hem w/o loss of consciousness, init | |
| S06.6X2A | Traum subrac hem w loss of consciousness of 31–59 min, init | |
| S06.6X9A | Traum subrac hem w LOC of unsp duration, init | |
| Joint disorders and dislocations; trauma-related | S13.130A | Subluxation of C2/C3 cervical vertebrae, initial encounter |
| Lower gastrointestinal disorders | K35.2 | Acute appendicitis with generalized peritonitis |
| K35.3 | Acute appendicitis with localized peritonitis | |
| K35.80 | Unspecified acute appendicitis | |
| K37 | Unspecified appendicitis | |
| K56.1 | Intussusception | |
| K56.2 | Volvulus | |
| K56.60 | Unspecified intestinal obstruction | |
| K56.69 | Other intestinal obstruction | |
| Miscellaneous mental disorders | F44.5 | Conversion disorder with seizures or convulsions |
| Other connective tissue disease | M60.009 | Infective myositis, unspecified site |
| M62.82 | Rhabdomyolysis | |
| Other endocrine disorders | E162 | Hypoglycemia, unspecified |
| Other injuries and conditions due to external causes | T17.910A | Gastric contents in resp tract, part unsp cause asphyx, init |
| T71.111A | Asphyx due to smothering under pillow, accidental, init | |
| T75.1XXA | Unsp effects of drowning and nonfatal submersion, init | |
| T75.1XXS | Unsp effects of drowning and nonfatal submersion, sequela | |
| T76.12XA | Child physical abuse, suspected, initial encounter | |
| T79.7XXA | Traumatic subcutaneous emphysema, initial encounter | |
| Other lower respiratory disease | J81.0 | Acute pulmonary edema |
| R06.81 | Apnea, not elsewhere classified | |
| Other nervous system disorders | G08 | Intracranial and intraspinal phlebitis and thrombophlebitis |
| G93.6 | Cerebral edema | |
| Other perinatal conditions | R68.13 | Apparent life threatening event in infant (ALTE) |
| Other upper respiratory disease | J38.5 | Laryngeal spasm |
| Pancreatic disorders (not diabetes) | K85.9 | Acute pancreatitis, unspecified |
| Pleurisy; pneumothorax; pulmonary collapse | J98.2 | Interstitial emphysema |
| Poisoning | T36.6X1A | Poisoning by rifampicins, accidental (unintentional), init |
| T38.3X1A | Poisoning by insulin and oral hypoglycemic drugs, acc, init | |
| T39.1X1A | Poisoning by 4-Aminophenol derivatives, accidental, init | |
| T40.2X1A | Poisoning by oth opioids, accidental (unintentional), init | |
| T41.291A | Poisoning by oth general anesthetics, accidental, init | |
| T42.4X1A | Poisoning by benzodiazepines, accidental, init | |
| T42.71XA | Poisn by unsp antieplptc and sed-hypntc drugs, acc, init | |
| T42.8X1A | Poisn by antiparkns drug/centr musc-tone depr, acc, init | |
| T43.211A | Poisn by slctv seroton/norepineph reup inhibtr, acc, init | |
| T43.291A | Poisoning by oth antidepressants, accidental, init | |
| T43.591A | Poisoning by oth antipsychot/neurolept, accidental, init | |
| T43.621A | Poisoning by amphetamines, accidental (unintentional), init | |
| T45.0X1A | Poisoning by antiallerg/antiemetic, accidental, init | |
| T46.2X1A | Poisoning by oth antidysrhythmic drugs, accidental, init | |
| T46.5X1A | Poisoning by oth antihypertn drugs, accidental, init | |
| T48.3X1A | Poisoning by antitussives, accidental (unintentional), init | |
| T51.0X1A | Toxic effect of ethanol, accidental (unintentional), init | |
| T53.0X1A | Toxic effect of carbon tetrachloride, accidental, init | |
| T54.91XA | Toxic effect of unsp corrosive substance, accidental, init | |
| T63.441A | Toxic effect of venom of bees, accidental, init | |
| Respiratory failure; insufficiency; arrest (adult) | J80 | Acute respiratory distress syndrome |
| Respiratory infections | J05.10 | Acute epiglottitis without obstruction |
| J36 | Peritonsillar abscess | |
| Skin and subcutaneous tissue infections | L03.115 | Cellulitis of right lower limb |
| L03.116 | Cellulitis of left lower limb | |
| L03.211 | Cellulitis of face | |
| L03.311 | Cellulitis of abdominal wall | |
| L03.317 | Cellulitis of buttock | |
| L08.82 | Omphalitis not of newborn | |
| Spinal cord injury | S14.135A | Anterior cord syndrome at C5, init |
| S14.136A | Anterior cord syndrome at C6, init | |
| S14.137A | Anterior cord syndrome at C7, init | |
| Substance-related disorders | P96.2 | Withdrawal symptoms from therapeutic use of drugs in newborn |
| T40.7X1A | Poisoning by cannabis (derivatives), accidental, init | |
| Suicide and intentional self-inflicted injury | T39.012A | Poisoning by aspirin, intentional self-harm, init encntr |
| T39.1X2A | Poisoning by 4-Aminophenol derivatives, self-harm, init | |
| T39.312A | Poisoning by propionic acid derivatives, self-harm, init | |
| T40.2X2A | Poisoning by oth opioids, intentional self-harm, init encntr | |
| T42.4X2A | Poisoning by benzodiazepines, intentional self-harm, init | |
| T43.222A | Poisn by slctv serotonin reuptake inhibtr, self-harm, init | |
| T43.292A | Poisoning by oth antidepressants, self-harm, init | |
| T43.592A | Poisoning by oth antipsychot/neurolept, self-harm, init | |
| T45.0X2A | Poisoning by antiallerg/antiemetic, self-harm, init | |
| T45.4X2A | Poisoning by iron and its compounds, self-harm, init | |
| T48.3X2A | Poisoning by antitussives, intentional self-harm, init | |
| T48.4X2A | Poisoning by expectorants, intentional self-harm, init | |
| T56.892A | Toxic effect of oth metals, intentional self-harm, init | |
| Symptoms; signs; and ill-defined conditions | R57.0 | Cardiogenic shock |
| R57.9 | Shock, unspecified | |
| T78.01XA | Anaphylactic reaction due to peanuts, initial encounter | |
| T78.05XA | Anaphylactic reaction due to tree nuts and seeds, init | |
| T78.1XXA | Oth adverse food reactions, not elsewhere classified, init | |
| T78.2XXA | Anaphylactic shock, unspecified, initial encounter | |
| Systemic lupus erythematosus and connective tissue disorders | M30.3 | Mucocutaneous lymph node syndrome [Kawasaki] |
| Unclassified | W65.XXXA | Accidental drowning and submersion while in bath-tub, init |
| W67.XXXA | Accidental drown while in swimming-pool, init |
References
[1] Gaski AL, Hickam DH, Sharp VL. The effect of trauma center designation on outcome of pediatric patients injured in motor vehicle collisions. Arch Pediatr Adolesc Med. 2000 Dec;154(12):1211-7. doi: 10.1001/archpedi.154.12.1211. PMID: 11115326.
[2] Cimpello LB, Khare RK, Shah MI, et al. Variation in access to pediatric subspecialty care in US emergency departments. Acad Emerg Med. 2013 Jun;20(6):594-601. doi: 10.1111/acem.12147. PMID: 23750625; PMCID: PMC3784870.
[3] Seigel TA, Patel HI, Swanson JW, Steiner JP, Myers SR. Pediatric hospital medicine workforce trends and the implications for training programs. J Hosp Med. 2014 Dec;9(12):812-6. doi: 10.1002/jhm.2255. PMID: 25384456.
[4] Mohr NM, Harland KK, Ebel BE, Shapiro RA, Rider AC, Guise JM. Potentially avoidable interfacility transfers of pediatric patients. Acad Emerg Med. 2016 Feb;23(2):178-87. doi: 10.1111/acem.12872. PMID: 26686449.
[5] Li J, Brown JB, Gestring ML, et al. Potentially preventable interhospital transfers in trauma patients: a retrospective multicenter study. J Trauma. 2008 Sep;65(3):628-35; discussion 635-7. doi: 10.1097/TA.0b013e318181414a. PMID: 18784579.
[6] Gattu R, Song L, Schamel J, Raykov N, Evans DC, Shapiro M. Avoidable pediatric trauma transfers: an opportunity for regionalized quality improvement. J Pediatr Surg. 2014 Dec;49(12):1803-7. doi: 10.1016/j.jpedsurg.2014.07.016. PMID: 25499030.
[7] Peebles R, Wagner J, Werner A, et al. Avoidable transfers to a tertiary children’s hospital. Pediatr Emerg Care. 2013 Jul;29(7):791-6. doi: 10.1097/PEC.0b013e3182994e15. PMID: 23807149.
[8] Kahn CA, Pirrallo RG, Steele TD, et al. The epidemiology of EMS-ambulance crashes in the United States. Prehosp Emerg Care. 2001 Oct-Dec;5(4):417-23. doi: 10.1080/10903120190940893. PMID: 11693457.
[9] Custalow CB, Gravitz CS. EMS ambulance crashes: characteristics and outcomes. Prehosp Emerg Care. 2004 Jul-Sep;8(3):261-71. doi: 10.1080/10903120490449830. PMID: 15248783.
[10] National Highway Traffic Safety Administration. Ambulance crashes: an examination of crash factors, injury outcomes, and injury prevention strategies. Washington, DC: National Highway Traffic Safety Administration; 2003.
[11] Committee on Hospital Care and Emergency Medical Services Section, American Academy of Pediatrics. Guidelines for air and ground transport of pediatric patients. Pediatrics. 2017 Mar;139(3):e20163876. doi: 10.1542/peds.2016-3876. PMID: 28242832.
[12] Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization for children in the United States with medical complexity. J Pediatr. 2011 Dec;159(6):E32-40. doi: 10.1016/j.jpeds.2011.07.008. PMID: 21855837.
[13] DeCamp LR, Byczkowski TL, Lesher SJ, et al. Racial and ethnic differences in emergency department utilization for asthma. J Pediatr. 2014 Dec;165(6):1161-7.e1. doi: 10.1016/j.jpeds.2014.08.050. PMID: 25262506; PMCID: PMC4254758.
[14] Goyal MK, Kuppermann N, Tancredi DJ, et al. Racial and ethnic disparities in rates of hospitalizations for bronchiolitis in US children. Pediatrics. 2014 Dec;134(6):1047-53. doi: 10.1542/peds.2014-1621. PMID: 25489052; PMCID: PMC4254757.
[15] Alansari SF, Lugtenberg M, Burgers JS, et al. Systematic review of factors associated with emergency department visits for childhood asthma. Allergy Asthma Clin Immunol. 2016 Aug 10;12:42. doi: 10.1186/s13223-016-0149-7. PMID: 27525109; PMCID: PMC4980433.
[16] Goodman DC, Chang AM, Clancy CM. Explaining variations in hospital admission rates. Health Aff (Millwood). 2005;Suppl Variation:W5-25-39. doi: 10.1377/hlthaffw5.25. PMID: 15590647.
[17] Weissman JS, Stern R, Fielding J, Epstein AM. Delayed access to primary care: risk factors and the impact on hospitalization. Ann Intern Med. 1991 Dec 15;115(12):895-901. doi: 10.7326/0003-4819-115-12-895. PMID: 1952476.
[18] Agrawal RK, Steiner JP, Myers SR, Miller GJ, Seigel TA. Hospital transfer patterns of pediatric patients in the United States. J Hosp Med. 2016 Sep;11(9):626-32. doi: 10.1002/jhm.2601. PMID: 27322129.
[19] Stranges S, Tigbe W, Warnakula S, Gulliford MC, Chaturvedi N, Donahue RP. Socioeconomic status, ethnicity, and the relationship between age and mortality: the Whitehall II study. Am J Public Health. 2006 Jul;96(7):1254-60. doi: 10.2105/AJPH.2005.071394. PMID: 16735718; PMCID: PMC1483962.
[20] Agency for Healthcare Research and Quality (AHRQ). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2014. Clinical Classifications Software (CCS) for ICD-9-CM.
[21] StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013.
[22] Hall DE, Kenny MK, Kuo DZ, et al. Hospital-to-hospital transfers for children with complex chronic conditions. Pediatrics. 2014 Oct;134(4):e1023-31. doi: 10.1542/peds.2014-0763. PMID: 25225432; PMCID: PMC4177512.
[23] Johnson TJ, Patel KM, King M, Evans D, Carraccio C. Direct admission processes for children: a national survey of pediatric hospitalists. J Hosp Med. 2016 Sep;11(9):633-9. doi: 10.1002/jhm.2602. PMID: 27322128.
[24]ൃത്തBorsky AJ, Cosgrove LA, Emanuel EJ, Navathe AS. Hospital care for common medical conditions is becoming more concentrated, 2002-11. Health Aff (Millwood). 2016 Mar 1;35(3):486-93. doi: 10.1377/hlthaff.2015.1013. PMID: 26957528; PMCID: PMC5070466.
[25] Marcin JP, Shaikh S, Steinhorn RH. Use of telemedicine to reduce hospitalizations for bronchiolitis in rural children. Pediatrics. 2004 Dec;114(6):1607-11. doi: 10.1542/peds.2004-0324. PMID: 15579669.
[26] Marcin JP, Cole SL, Traylor R, et al. Telemedicine reduces the transfer of critically ill infants and children in rural California. Pediatr Crit Care Med. 2001 Jul;2(3):214-8. doi: 10.1097/00130478-200107000-00008. PMID: 12003513.
[27] Marcin JP, McVey T, Cuevas D, et al. Decreasing unnecessary transfers of infants and children by using telemedicine: a prospective clinical trial. J Perinatol. 2007 Dec;27(12):743-8. doi: 10.1038/sj.jp.7211830. PMID: 17975554.
[28] Meyer K, Nataraja RM, Reichert P, Knops J, Heusch A, Goepel W. Telemedicine in neonatal care: experiences from a German tele-NICU network. Klin Padiatr. 2011 Mar;223(2):105-9. doi: 10.1055/s-0030-1262647. PMID: 21351153.
[29] Nelson EL, Lindemann EA, Freeman WL, et al. Telemedicine for pediatric critical care: a systematic review and meta-analysis. Pediatr Crit Care Med. 2017 Jan;18(1):8-18. doi: 10.1097/PCC.0000000000000965. PMID: 27662300.
[30] American Academy of Pediatrics Council on Child Health Care Financing and Committee on Telehealth. Telehealth: policy statement. Pediatrics. 2015 Jan;135(1):183-91. doi: 10.1542/peds.2014-3668. PMID: 25512588.
[31] Brokamp C, Wicklund C, Ebeling M, Marcin JP. Current status of telemedicine in pediatric critical care. World J Crit Care Med. 2016 Feb 4;5(1):47-58. doi: 10.5492/wjccm.v5.i1.47. PMID: 26866089; PMCID: PMC4741187.
[32] Marcin JP, Nesbitt TS. Clinical applications of telemedicine in the care of children. Pediatrics. 2017 Jan;139(1):e20163527. doi: 10.1542/peds.2016-3527. PMID: 27940781.
[33] Swanson JO, Chuo J, Graham DA, Leslie DL, Marcin JP. Impact of telemedicine consultation on care in rural emergency departments: a qualitative study. Telemed J E Health. 2014 Dec;20(12):1115-20. doi: 10.1089/tmj.2014.0049. PMID: 25347646; PMCID: PMC4262812.
Footnotes
Conflicts of Interest: Regarding conflicts of interest, none were declared.