Tinea pedis, commonly known as athlete’s foot, is a prevalent fungal infection affecting the skin of the feet. Accurate diagnosis and coding are crucial for effective healthcare management and billing processes. In the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), the Diagnosis Code For Tinea Pedis is B35.3. This article provides a detailed overview of the ICD-10-CM code B35.3, its clinical application, and essential information about tinea pedis for healthcare professionals and anyone seeking to understand this common condition.
Understanding ICD-10-CM Code B35.3 for Tinea Pedis
The ICD-10-CM is a standardized system used to classify and code diagnoses for medical billing, epidemiology, and health management. Code B35.3 specifically designates Tinea pedis, making it a billable and specific code for reimbursement purposes. This code became effective in the American ICD-10-CM version in October 2015, with the latest edition being the 2025 version, effective from October 1, 2024. It’s important to note that while B35.3 is consistent in the American version, international versions of ICD-10 B35.3 may have variations.
This code is applicable when the diagnosis is:
- Athlete’s foot: The common term for tinea pedis, highlighting its association with athletes due to damp environments like locker rooms and gyms.
- Dermatophytosis of foot: This is a broader medical term indicating a fungal infection of the skin on the foot, caused by dermatophytes.
- Foot ringworm: Another term referring to tinea pedis, although it’s important to clarify that ringworm is not caused by worms but by fungi.
Clinical Insights into Tinea Pedis (Athlete’s Foot)
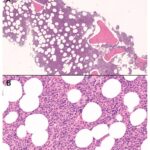
Tinea pedis is a fungal infection primarily caused by dermatophytes, including Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum. These fungi thrive in warm, moist environments, making areas like between the toes, showers, swimming pools, and locker rooms common places for transmission.
Symptoms of Athlete’s Foot
The hallmark symptoms of tinea pedis include:
- Itching and burning: Often intense, especially between the toes and on the soles of the feet.
- Cracked, scaly skin: Particularly between the toes, but can also extend to the soles and sides of the feet.
- Redness: Inflammation of the affected skin.
- Blisters: In some cases, small blisters may form, which can be itchy and painful.
- Dryness and peeling: Chronic athlete’s foot can present as dry, flaky skin resembling eczema.
Prevention Strategies for Tinea Pedis
Preventing athlete’s foot involves maintaining foot hygiene and avoiding environments conducive to fungal growth:
- Keep feet clean and dry: Wash feet daily with soap and water, and dry thoroughly, especially between the toes.
- Wear clean socks: Change socks daily, and more often if feet become sweaty. Opt for breathable materials like cotton or moisture-wicking fabrics.
- Avoid walking barefoot in public areas: Wear flip-flops or sandals in communal showers, locker rooms, and around swimming pools.
- Keep toenails clean and short: Regular nail trimming and cleaning can help prevent fungal buildup.
- Allow shoes to air out: Don’t wear the same pair of shoes every day. Allow them to dry completely between wearings.
Treatment Options for Tinea Pedis
Most cases of athlete’s foot can be effectively treated with over-the-counter (OTC) antifungal medications. These come in various forms such as creams, sprays, and powders containing ingredients like:
- Clotrimazole
- Miconazole
- Terbinafine
- Tolnaftate
For more severe or persistent infections, prescription antifungal medications may be necessary. These can include stronger topical treatments or oral antifungal medications. It’s important to complete the full course of treatment, even if symptoms improve, to ensure complete eradication of the fungus and prevent recurrence.
When to Seek Medical Advice
While many cases of athlete’s foot resolve with OTC treatments, it’s advisable to consult a healthcare professional if:
- Symptoms worsen or do not improve after two weeks of OTC treatment.
- The infection spreads to other parts of the body, such as the nails (onychomycosis).
- There are signs of secondary bacterial infection, such as increased pain, swelling, pus, or fever.
- You have underlying conditions like diabetes or a weakened immune system.
ICD-10-CM B35.3 Code History
The ICD-10-CM code B35.3 has remained consistent since its introduction into the classification system. The code history confirms:
- 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM)
- 2017 through 2025 (effective 10/1/2016 – 10/1/2024): No change
This stability indicates the established and consistent recognition of Tinea pedis as a distinct diagnostic entity within the ICD-10-CM framework.
Context within ICD-10-CM: Codes Adjacent to B35.3
Understanding the surrounding codes can provide a broader context within the ICD-10-CM classification. Codes adjacent to B35.3 include other dermatophytoses and related conditions:
- B35 Dermatophytosis: This is the parent category for fungal infections of the skin caused by dermatophytes.
- B35.0 Tinea barbae and tinea capitis: Fungal infections of the beard and scalp, respectively.
- B35.1 Tinea unguium: Also known as onychomycosis, fungal infection of the nails.
- B35.2 Tinea manuum: Fungal infection of the hand.
- B35.4 Tinea corporis: Ringworm of the body.
- B35.6 Tinea cruris: Jock itch, fungal infection of the groin.
- B36 Other superficial mycoses: This category includes other superficial fungal infections, further differentiating tinea pedis from other types of fungal skin conditions.
Conclusion
Accurate use of the diagnosis code B35.3 is essential for properly classifying and documenting cases of tinea pedis. This code not only facilitates correct medical billing and reimbursement but also contributes to epidemiological tracking and public health management of this common fungal infection. For individuals experiencing symptoms of athlete’s foot, understanding prevention and treatment options is key, and seeking professional medical advice is recommended for persistent or severe cases.