Comprehensive health care services are essential for everyone, particularly for individuals with learning disabilities. These services must go beyond treating immediate health issues and focus on the overall well-being of patients, encompassing understanding, communication, involvement, counseling, and respect. Historically, health care for people with learning disabilities has often fallen short, marked by communication gaps and a lack of understanding regarding their unique needs. This article addresses these critical aspects, touching upon the significance of diagnosis codes in healthcare contexts, and while not directly related to diagnosis code P351 in audiology (which typically pertains to newborn conditions), we aim to explore the broader spectrum of health care needs, including audiological considerations, for individuals with learning disabilities.
Health Care Needs of People with Learning Disabilities
Ordinary Health Care Needs
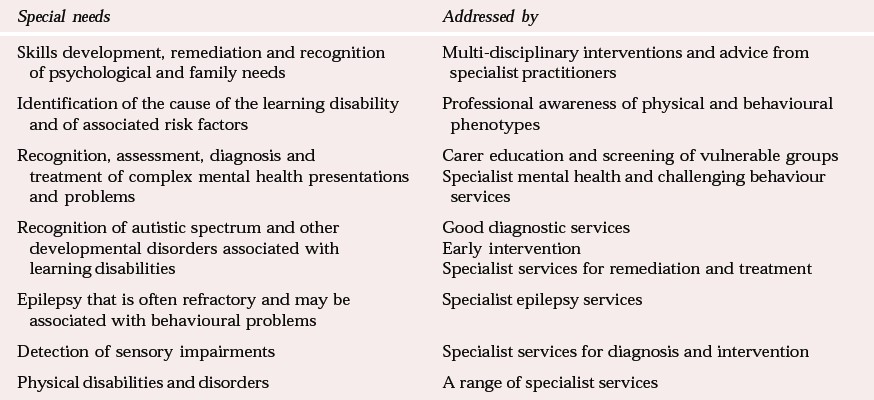
People with learning disabilities, like all individuals, have fundamental health care needs and the right to access comprehensive health services. This includes preventative care, primary health services, community health initiatives, and specialist interventions when necessary. However, significant barriers hinder their access, primarily stemming from their learning and communication difficulties, and the knowledge gaps, attitudes, and beliefs of caregivers, clinicians, and service administrators. These challenges lead to several consequences, detailed below and summarized in Table 1.
Learning and Communication Difficulties
Individuals with learning disabilities might struggle to grasp the importance of a healthy lifestyle, preventative health screenings, or identifying symptoms of illness. This can result in challenges in adhering to healthy practices or participating in crucial health checks. Furthermore, when unwell, they may not communicate their discomfort effectively due to difficulties in recognizing symptoms or expressing themselves.
To address these challenges, services should prioritize health education tailored to individuals with learning disabilities, using accessible communication methods. Resources like picture-based books can be invaluable tools for both individuals and their caregivers. Community learning disability teams have successfully employed group sessions to raise awareness of health issues.
For those with severe learning and communication difficulties, recognizing subtle signs of discomfort or pain is crucial. Caregivers need to be highly attuned to behavioral changes or shifts in well-being that could indicate underlying health problems. Regular health assessments, including dental and sensory checks, are vital for early detection of potential issues. These screenings should also encompass mental health, utilizing tools like the Psychiatric Assessment Schedule for Adults with Developmental Disabilities (PAS–ADD).
Poor Carer and Professional Awareness
Caregivers and even healthcare professionals may not fully appreciate the importance of a healthy lifestyle for individuals with learning disabilities or may misinterpret indicators of health problems. Inexperienced individuals might mistakenly attribute changes in behavior to the learning disability itself, rather than considering underlying discomfort or mental health issues. Many caregivers, both family and paid, lack adequate knowledge about health-related concerns. Therefore, accessible training opportunities are essential for caregivers, and ongoing education for all health professionals is crucial to ensure they can effectively address the ordinary and special needs of people with learning disabilities.
Discrimination
Unfortunately, people with learning disabilities can face undervaluation and discrimination from caregivers and professionals, leading to their health needs being overlooked or dismissed. In severe instances, this can result in neglect and inadequate care. More commonly, it manifests as subtle discrimination and neglect of essential health care.
Addressing discrimination requires multifaceted approaches. Training for caregivers and professionals should include critical reflection on personal and societal attitudes and beliefs, and how these impact service delivery and responses. Direct engagement and dialogue with self-advocates and family caregivers can foster positive changes in perspectives. Organizations should implement clear anti-discrimination policies aligned with disability legislation, alongside robust ‘whistle-blowing’ procedures. Codes of conduct for professional organizations should explicitly address these issues.
Physical and Administrative Barriers
Physical and administrative obstacles can significantly impede access to health services. These include inaccessible buildings, unclear signage, inadequate support, confusing appointment information, scheduling difficulties, and unclear treatment instructions. Individuals with learning disabilities may require thorough preparation for hospital visits or admissions, including opportunities to familiarize themselves with the environment and procedures. Resources like accessible books can aid in this preparation. Consent processes must also be carefully navigated to avoid becoming another barrier to access. Services must proactively listen to the needs of people with learning disabilities and specialist learning disability services to implement necessary adaptations and ensure flexibility to accommodate diverse needs.
Social Factors
Access to health care is further complicated by insensitivity to the social, ethnic, cultural, and economic backgrounds of individuals and their families. Services must acknowledge and understand these diverse factors to provide equitable care.
Special Health Care Needs
Beyond ordinary health needs, people with learning disabilities often experience more complex and specialized health requirements compared to the general population. They exhibit higher rates of general health problems, mental health conditions, epilepsy, sensory impairments, cerebral palsy, and other physical disabilities. They require support for personal development, and numerous syndromes and genetic conditions associated with learning disabilities carry specific health risks.
To address these special needs, collaborative efforts between health, education, and social services are essential. Professionals from various disciplines can provide guidance on skill development and strategies to overcome disabilities. Physiotherapists play a key role in gross motor skill development, occupational therapists in fine motor skills and coordination, and speech and language therapists in communication skills. Mental health professionals contribute by promoting emotional well-being, self-confidence, and secure attachments. It is also crucial to recognize and support family members who may face mental health challenges while adjusting to their child’s disability and managing the demands of care.
The Cause of the Disability
Identifying the underlying cause of a learning disability is important as it can reveal specific physical or mental health risks associated with the condition. For instance, individuals with Down’s syndrome have an increased risk of congenital heart disease, sensory impairments, thyroid disorders, and early-onset dementia. Those with tuberous sclerosis are more susceptible to epilepsy, renal disorders, autistic spectrum disorders, and certain tumors. Awareness of these physical and behavioral phenotypes is crucial for healthcare professionals to proactively address potential health problems.
Mental Health Needs
Assessing, diagnosing, and treating mental health issues in people with learning disabilities demands a thorough understanding of genetic, neurological, and social factors that contribute to the elevated rates of mental illness in this population. Co-occurring developmental disorders, such as autism spectrum disorder and ADHD, must also be considered. Mental health conditions may present atypically in this population, and diagnosis can be particularly challenging for individuals with severe learning disabilities due to the reliance on self-reported symptoms in diagnostic criteria. Consequently, mental health problems are likely underreported in people with learning disabilities.
Targeted Services
The need for comprehensive mental health services tailored to people with learning disabilities is well-justified. Studies indicate a significant percentage of adults with learning disabilities also experience mental health needs arising from psychiatric and behavioral disorders. Rates of specific conditions like schizophrenia are also elevated compared to the general population. Interestingly, some research suggests that rates of anxiety and depression may be higher in community settings compared to institutional care, potentially reflecting the stresses of daily life without adequate support and attention to lifestyle factors.
Challenging behavior is often intertwined with carer stress and reactions, which can inadvertently reinforce these behaviors. The ambiguous nature of challenging behavior complicates the accurate assessment of mental health problem prevalence. While behavioral approaches and, in some cases, psychotropic medication can be effective, mental health problems in individuals with learning disabilities can manifest across all age groups, with children, adolescents, and older adults particularly vulnerable. Offending behaviors, sometimes linked to psychiatric disorders, are also overrepresented in this population.
Developmental Disorders
Many individuals with learning disabilities also have co-occurring developmental disorders like autism spectrum disorder and hyperactivity. It is crucial for all services to possess the expertise to recognize and address these conditions effectively. This requires robust diagnostic services for early detection, ideally involving child and adolescent psychiatry, pediatrics, or specialist learning disability services. Early intervention for conditions like autism spectrum disorder can lead to significant improvements. ADHD may benefit from stimulant medication under specialist supervision. Communication and coordination disorders require skilled therapeutic interventions and supportive environments.
Epilepsy
Access to specialist epilepsy services is vital, given the high prevalence of epilepsy among people with learning disabilities. They are also at greater risk of complex and treatment-resistant seizure disorders. Modern epilepsy management includes specialist referral, thorough examination, seizure monitoring, and medication management. Expert knowledge of anti-epileptic drugs and their associated risks is essential.
Sensory Impairments
Sensory impairments must be promptly identified and addressed to minimize their impact. A specialized and sensitive approach is often necessary. A significant proportion of people with learning disabilities experience sight and hearing impairments, sometimes co-occurring, leading to complex disabilities. The prevalence increases with age, and sensory issues can be mistaken for behavioral changes. Underdetection is common, despite the treatability of many sensory impairments.
Physical Disabilities
A substantial percentage of people with learning disabilities also have physical disabilities, often due to cerebral palsy. These individuals require input from a range of specialist services. Secondary health problems related to physical disabilities, such as reflux, aspiration pneumonia, joint pain, and muscle spasms, are common and can manifest as behavioral issues if pain is misdiagnosed or unmanaged. Pain management is particularly critical for those who struggle to communicate discomfort. Some individuals have highly complex needs due to multiple disabilities and require lifelong, comprehensive care, including specialized equipment and adaptations. With advances in care, children with profound disabilities are living longer, often requiring advanced medical technologies and palliative care.
Changes in Health Care Services
Previous Patterns of Service Delivery
Historically, large institutions were established for people with learning disabilities, primarily for care and segregation rather than therapeutic intervention. These hospitals often became overcrowded, leading to poor care standards and institutionalization. The UK has undergone a significant shift towards community resettlement over the past three decades, recognizing that community services can effectively support individuals even with complex health needs when agencies collaborate. Specialist community learning disability teams have become increasingly prevalent, enhancing the knowledge and skill base for more effective interventions. However, those living in the community have often faced underrecognized and undertreated health needs within mainstream health services. Specialist services play a crucial role in highlighting access barriers and addressing special needs.
Present and Future Trends
Health service provision for people with learning disabilities is evolving, moving away from institutional care towards personalized community-based support. Social care is increasingly separated from health services, emphasizing individual strengths and needs. This shift necessitates strong partnerships between organizations to ensure health care needs are not neglected. There is growing recognition that institutionalization and poor care quality can occur in any setting, requiring collaborative efforts to optimize service quality and effectiveness.
Policy reviews at government levels reflect these international and national changes, emphasizing future health care service provision.
Elements of Comprehensive Health Care Services
Comprehensive health care for people with learning disabilities requires enhancing access to mainstream services and providing specialist services when mainstream options are insufficient. Effective coordination and planning are essential for individuals with complex and long-term needs.
Access to Mainstream Services
Health promotion initiatives must be accessible and tailored to people with learning disabilities of all ages, also educating caregivers and professionals. Mental health promotion should be prioritized alongside physical health. Screening services need to be inclusive and supportive of individuals with learning disabilities. Primary health care services are crucial as both providers of care and gateways to specialist services. Health facilitators within community learning disability teams are vital in supporting access to primary and other NHS services, encompassing both physical and mental health needs. Health Action Plans, developed in partnership with primary care, are a novel approach to improving health outcomes. Access to other community health services like dental, optician, audiology, and pharmaceutical services must also be facilitated. General hospital services need to improve sensitivity and flexibility to meet special needs, addressing complaints of discriminatory attitudes. National Service Frameworks apply equally to people with learning disabilities, ensuring the same standards of care as the general population.
Access to Specialist Health Services
Children
Specialist child health services are increasingly community-focused. Community pediatricians, nurses, and children’s hospices provide long-term, holistic care valued by families. Some services incorporate psychology and mental health support, collaborating with child and adolescent psychiatric services or specialist learning disability services. Sensitive communication and counseling from the time of diagnosis are crucial for families. However, services for children and adolescents with complex mental health problems remain inadequate in many areas, hindering early intervention efforts.
Adults
Specialist mental health services for adults with learning disabilities are more established than specialist physical health services, creating a gap in addressing complex physical health needs, particularly as individuals with severe conditions live longer. Community learning disability teams often include physiotherapists and learning disability nurses with a holistic approach, but medical support may be limited. Countries like The Netherlands offer excellent specialist physical health services for adults with learning disabilities, highlighting the variability in service provision internationally.
Epilepsy
Access to epilepsy services varies, with providers including pediatricians, neurologists, and learning disability psychiatrists. Epilepsy nurse specialists play a vital role in patient education, support, and monitoring within learning disability and neurology services. Tertiary neuropsychiatric services also exist.
Old Age Services
As people with learning disabilities live longer, specialist services for older adults are increasingly necessary, requiring collaboration between learning disability and old age services.
Mainstream v. Specialist Care
Specialist mental health services for people with learning disabilities in the UK are highly regarded internationally but have also faced criticism for potential discrimination and exclusion from mainstream mental health services. While inclusion is important, mainstream services must be equipped to address special needs to avoid disadvantaging individuals. Overstretched mainstream services often lack the resources and expertise, highlighting the continued need for well-resourced specialist services. Forensic patients face even greater challenges due to a shortage of specialized in-patient and out-patient services. Local in-patient services for specialist psychiatric assessment and treatment are essential, with bed numbers dependent on effective community services. Specialist mental health services should cater to all ages and a wide range of mental health problems, also facilitating access to mainstream mental health services when appropriate.
Equal Access to Health Care
High-quality, multi-disciplinary specialist services are crucial, with community learning disability teams playing a central role. Their focus is evolving to enhance the competence of local services through direct support, training, and service development, requiring collaborative partnerships. Access to in-patient, outreach, and other specialized services is also essential. Ongoing training for health professionals in understanding the needs of people with learning disabilities is vital for equitable access. Primary health care services are increasingly responsible for health care planning and coordination, supported by specialist learning disability services. Health Action Plans and health facilitators are critical components in improving health service provision. Organizations must support these changes at all levels to ensure success.
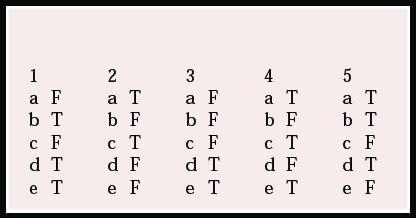
Multiple choice questions
- People with learning disabilities:
- a need separate health care services
- b often can learn to advocate for their own health
- c are less aware of pain than other people
- d often experience discrimination
- e need regular health checks.
- As regards the health of people with learning disabilities:
- a they have a much higher rate of mental health problems than the general population
- b about 50% show seriously challenging behaviour
- c about 40% have a significant hearing loss
- d they have the same rate of autistic disorders as the general population
- e about 60% have epilepsy.
- Large hospitals for people with learning disabilities in the UK:
- a were all closed by 1999
- b at one time cared for more people with learning disabilities than were left in the community
- c provided better health care than was available in the community
- d had professional staff who relocated to community teams
- e provided an institutional model of care.
- UK policy for health care services for people with learning disabilities includes:
- a specialist mental health assessment and treatment beds
- b placing all offenders in medium secure units
- c access to child and adolescent mental health services
- d exclusion from mainstream health services
- e provision of special health promotion information and programmes.
- In the future, community services for people with learning disabilities in the UK are likely to:
- a ensure availability of a health professional who will facilitate access to health care services
- b make training in disability awareness a fundamental part of professional training
- c make special provision for health care for all
- d provide Health Care Plans for all
- e stop providing specialist learning disability health care services.
MCQ answers
| 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| a | F | a | F | a |
| b | T | b | F | b |
| c | F | c | T | c |
| d | T | d | F | d |
| e | T | e | F | T |