Encephalitis, an inflammation of the brain, requires prompt and accurate diagnosis to ensure timely and effective treatment. If you or a loved one are experiencing symptoms suggestive of encephalitis, understanding the diagnostic process is crucial. This article, based on expert medical guidelines, will detail the methods healthcare professionals use to diagnose encephalitis, paving the way for appropriate care and recovery.
Diagnostic Procedures for Encephalitis
Diagnosing encephalitis involves a comprehensive approach, beginning with a thorough physical examination and review of your medical history by a healthcare professional. Following this initial assessment, several diagnostic tests may be recommended to confirm encephalitis and identify its underlying cause.
Neurological Exam and Medical History
The first step in diagnosing encephalitis is a neurological exam. This assessment evaluates various aspects of neurological function, including:
- Mental Status: Assessing awareness, alertness, and cognitive abilities.
- Motor Function: Checking muscle strength, coordination, and reflexes.
- Sensory Function: Testing the ability to feel touch, pain, temperature, and vibration.
- Cranial Nerves: Evaluating the function of nerves directly connected to the brain, affecting vision, hearing, taste, smell, facial movements, and swallowing.
- Balance and Coordination: Observing gait and posture.
Alongside the neurological exam, a detailed medical history is essential. Your healthcare provider will ask about:
- Symptom Onset and Progression: When did the symptoms start and how have they evolved?
- Recent Illnesses: Have you recently had a cold, flu, or any other infections?
- Travel History: Have you traveled to areas where specific infections are prevalent?
- Exposure to Vectors: Have you been bitten by mosquitoes or ticks recently?
- Vaccination Status: Are you up-to-date with your vaccinations?
- Underlying Conditions: Do you have any pre-existing conditions that might weaken your immune system or increase susceptibility to infections?
- Medications: Are you currently taking any medications, especially new ones?
- Exposure to Toxins or Animals: Have you been exposed to any wild animals or potential toxins?
This comprehensive evaluation helps healthcare professionals narrow down the possible causes and determine the most appropriate diagnostic tests.
Brain Imaging: MRI and CT Scans
Brain imaging plays a vital role in diagnosing encephalitis. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are commonly used to visualize the brain and identify abnormalities.
- MRI (Magnetic Resonance Imaging): MRI is often the preferred imaging technique for encephalitis diagnosis. It provides detailed images of the brain’s soft tissues, allowing for the detection of:
- Inflammation and Swelling: MRI can reveal areas of brain swelling (edema) and inflammation, characteristic of encephalitis.
- Lesions: It can identify lesions or abnormalities in specific brain regions affected by the inflammation.
- Underlying Conditions: MRI can help rule out other conditions that might mimic encephalitis symptoms, such as brain tumors or strokes.
Alt text: Brain MRI scan displaying areas of inflammation indicative of encephalitis, highlighting the diagnostic capabilities of neuroimaging.
- CT Scan (Computed Tomography): CT scans are quicker and more readily available than MRIs. While CT scans are less sensitive in detecting subtle changes of encephalitis in its early stages, they are valuable for:
- Initial Assessment: CT scans can be used for a rapid initial assessment, especially in emergency situations.
- Ruling out other conditions: CT scans are effective in excluding other conditions like hemorrhage or tumors that may present with similar symptoms.
- Detecting complications: In some cases, CT scans can identify complications of encephalitis, such as hydrocephalus (fluid buildup in the brain).
Lumbar Puncture (Spinal Tap): Cerebrospinal Fluid Analysis
A lumbar puncture, also known as a spinal tap, is a crucial diagnostic procedure for encephalitis. This procedure involves inserting a needle into the lower back to collect a sample of cerebrospinal fluid (CSF), the fluid that surrounds and protects the brain and spinal cord. Analyzing CSF provides vital information about the condition of the central nervous system.
- Identifying Infection and Inflammation: CSF analysis can detect signs of infection and inflammation within the brain and meninges (membranes surrounding the brain and spinal cord), confirming encephalitis.
- Determining the Cause: CSF samples can be tested to identify the specific cause of encephalitis, including:
- Viral Infections: Detecting viral genetic material (DNA or RNA) through PCR (polymerase chain reaction) tests.
- Bacterial Infections: Identifying bacteria through culture and other tests.
- Fungal Infections: Detecting fungi through culture and microscopic examination.
- Autoimmune Encephalitis Markers: Identifying antibodies associated with autoimmune encephalitis, where the body’s immune system mistakenly attacks the brain.
Alt text: Illustration of a lumbar puncture procedure being performed to collect cerebrospinal fluid for encephalitis diagnosis, emphasizing the technique and sample collection.
Blood, Urine, and Throat Swab Tests
In addition to CSF analysis, blood, urine, and throat swab samples may be collected for laboratory testing to identify infectious agents or other markers related to encephalitis.
- Blood Tests: Blood samples can be analyzed for:
- Viral Antibodies: Detecting antibodies against specific viruses, indicating a recent or past infection.
- Inflammatory Markers: Measuring levels of inflammatory markers, which can be elevated in encephalitis.
- Autoimmune Antibodies: Identifying specific antibodies associated with autoimmune encephalitis.
- Urine Tests: Urine samples may be tested for:
- Viral Shedding: Detecting the presence of certain viruses being shed in the urine.
- Infections: Ruling out other systemic infections that might contribute to neurological symptoms.
- Throat Swabs: Throat swabs can be used to:
- Detect Respiratory Viruses: Identifying viruses that may have spread to the brain, causing encephalitis.
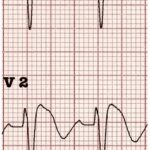
Electroencephalogram (EEG): Monitoring Brain Electrical Activity
An Electroencephalogram (EEG) is a non-invasive test that measures the brain’s electrical activity using electrodes attached to the scalp. EEG is helpful in diagnosing encephalitis and assessing its severity.
- Detecting Abnormal Brain Activity: EEG can identify abnormal brain wave patterns that are common in encephalitis, such as:
- Slowing of Brain Waves: Generalized or focal slowing of brain activity, indicating brain dysfunction.
- Seizure Activity: Identifying seizure discharges, as seizures are a common complication of encephalitis.
- Triphasic Waves: Certain EEG patterns, like triphasic waves, can be suggestive of specific types of encephalitis.
Alt text: Image of an EEG procedure in progress, demonstrating the placement of electrodes on the scalp to monitor brain electrical activity for encephalitis diagnosis.
Body Imaging for Autoimmune Encephalitis
In cases where autoimmune encephalitis is suspected, body imaging may be recommended to search for underlying tumors that can trigger an autoimmune response. These tumors, whether cancerous or noncancerous, can sometimes cause the immune system to attack the brain.
- Ultrasound, CT, MRI, and PET-CT Scans: Various imaging techniques may be used to scan the:
- Chest: To look for lung tumors or thymomas.
- Abdomen and Pelvis: To identify tumors in the ovaries, testes, or other organs.
If a tumor is detected, a biopsy (removing a small tissue sample for examination) may be performed to determine its nature and guide treatment.
Brain Biopsy: A Rare Diagnostic Procedure
Brain biopsy, the surgical removal of a small sample of brain tissue for laboratory analysis, is rarely needed for encephalitis diagnosis. It is typically considered only in specific circumstances:
- Worsening Symptoms Despite Treatment: If encephalitis symptoms worsen despite initial treatments, a brain biopsy might be considered to obtain a definitive diagnosis and guide further management.
- Unclear Diagnosis: When other diagnostic tests are inconclusive, and the cause of encephalitis remains uncertain, a brain biopsy may be necessary to identify the underlying pathology.
Treatment Strategies Following Diagnosis
Once encephalitis is diagnosed and the underlying cause is identified, treatment can be tailored to address the specific condition. Treatment strategies vary depending on the type of encephalitis and its severity.
-
Treatment for Mild Encephalitis: Mild cases often resolve with supportive care, including:
- Bed Rest: Allowing the body to recover.
- Fluid Intake: Maintaining hydration.
- Over-the-counter pain relievers: Such as acetaminophen or ibuprofen, to manage headache and fever.
-
Antiviral Medications for Viral Encephalitis: Encephalitis caused by certain viruses, like herpes simplex virus (HSV), requires antiviral treatment. Common antiviral medications include acyclovir, ganciclovir, and foscarnet.
-
Immunomodulatory Therapies for Autoimmune Encephalitis: Autoimmune encephalitis is treated by modulating the immune system to reduce the attack on the brain. Treatments may include corticosteroids, intravenous immunoglobulin (IVIG), plasma exchange, and immunosuppressant medications for long-term management.
-
Supportive Care for Severe Encephalitis: Hospitalized patients with severe encephalitis may require:
- Breathing assistance: Ventilator support if breathing is compromised.
- Intravenous fluids and electrolytes: To maintain hydration and electrolyte balance.
- Anti-seizure medications: To prevent or treat seizures.
- Anti-inflammatory medications: Like corticosteroids, to reduce brain swelling and pressure.
-
Follow-up Rehabilitation: Recovery from encephalitis may involve various therapies to address neurological deficits:
- Brain rehabilitation: To improve cognitive function and memory.
- Physical therapy: To regain strength, balance, and motor skills.
- Occupational therapy: To relearn daily living skills.
- Speech therapy: To improve speech and swallowing.
- Psychotherapy: To address emotional and behavioral changes.
Conclusion
Accurate and timely diagnosis is paramount in managing encephalitis effectively. Utilizing a combination of neurological exams, medical history, brain imaging, CSF analysis, EEG, and other laboratory tests, healthcare professionals can diagnose encephalitis and determine its cause. This precise diagnosis is the first step towards initiating appropriate treatment and supportive care, ultimately improving patient outcomes and facilitating recovery. If you suspect encephalitis, seek immediate medical attention to begin the diagnostic process and receive the necessary care.