Human Papillomavirus (HPV) is a common viral infection, belonging to the papillomavirus family, characterized by its double-stranded DNA structure and its ability to induce cytopathic effects in epithelial tissues. Genital HPV infections are frequently persistent, affecting multiple sites, and often present without noticeable symptoms (subclinical).
More than 40 HPV types are known to be sexually transmitted and infect the anogenital region.1 Certain types of sexually transmitted HPV can cause genital warts. However, persistent infection with high-risk HPV types, distinct from those causing common skin warts, can lead to precancerous lesions and eventually invasive cancers.2 HPV infection is the primary cause in the vast majority of cervical cancer cases.3 Despite this serious link, most HPV infections, even with high-risk types, do not result in cancer.
HPV is transmitted through direct skin-to-skin contact. This can occur through various routes, including direct contact with skin, such as plantar wart viruses entering through broken skin, sexual intercourse, and oral sexual activities or kissing. It’s important to recognize that symptomatic HPV infection represents only a fraction of the total cases, often described as just “the tip of the iceberg” Figure 1. Asymptomatic shedding of the virus is significantly more prevalent, especially in individuals with HIV/AIDS, who are more likely to spread the virus unknowingly. High rates of asymptomatic HPV/DNA shedding from the perianal region have been observed, particularly in AIDS patients with advanced disease stages, reaching as high as 78.9%.4
Figure 1.
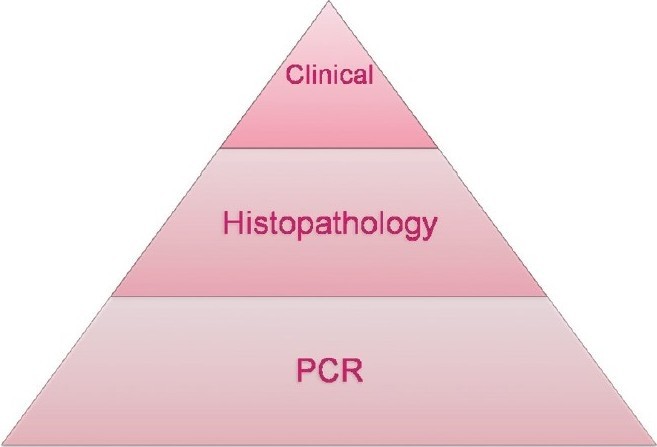 HPV infection iceberg representing subclinical, multifocal, and persistent nature
HPV infection iceberg representing subclinical, multifocal, and persistent nature
While condom use has not been consistently shown to prevent subclinical HPV infection (HPV DNA positivity), it has been associated with a reduced risk of developing genital warts, cervical intraepithelial neoplasia (CIN) 2-3, and invasive cervical cancer.5
The Crucial Role of HPV Diagnosis
Accurate and timely Diagnosis Of Hpv is paramount for several reasons. Early detection allows for the identification of high-risk HPV types that are more likely to cause precancerous changes. This early warning enables healthcare providers to implement appropriate monitoring and intervention strategies, significantly reducing the risk of progression to cervical cancer and other HPV-related cancers. For individuals, understanding their HPV status can alleviate anxiety, guide informed decisions about sexual health, and promote responsible behavior to prevent further transmission. From a public health perspective, effective HPV diagnosis strategies are essential for screening programs aimed at reducing the incidence and mortality associated with HPV-related malignancies.
Methods for HPV Diagnosis
Traditional virology methods like electron microscopy, cell culture, and standard immunological assays are not practical for HPV diagnosis. HPV is notoriously difficult to culture in laboratory settings. Therefore, current diagnostic approaches rely on a combination of clinical procedures and advanced molecular techniques. The primary methods for diagnosing HPV infection include:
- Colposcopy and Acetic Acid Test
- Biopsy
- DNA Tests (PCR, Southern Blot Hybridization, In Situ Hybridization)
- Pap Smear
Colposcopy and Acetic Acid Test: Visualizing Cervical Abnormalities
Colposcopy is a specialized outpatient procedure performed by trained clinicians using a colposcope, a low-magnification microscope.6 It involves a detailed examination of the cervix, vagina, and sometimes the vulva after applying an acetic acid solution. This technique is crucial for identifying areas that are suspicious for precancerous or cancerous changes, guiding biopsies to the most relevant sites.7 Colposcopic findings are assessed based on factors like the degree of acetowhitening, surface irregularities, mosaic patterns, and punctation. More pronounced abnormalities in these features are indicative of more severe lesions.
Acetic Acid Test: Enhancing Lesion Visibility
The acetic acid test is a simple yet effective adjunct to colposcopy. Applying a 3–5% acetic acid solution, typically using a moistened gauze pad for 5-10 minutes, to suspected lesions on the penis, cervix, labia, or perianal area can significantly improve lesion detection. Subtle, flat lesions that might be difficult to see under normal conditions become more apparent as genital warts, dysplastic tissues, and neoplastic tissues turn white (acetowhite).
It is important to note that the acetic acid test is not specific to HPV and can produce false-positive results. Any condition causing parakeratosis, such as candidiasis, psoriasis, lichen planus, healing epithelium, and even sebaceous glands, can lead to acetowhitening. Therefore, the acetic acid test is not recommended for routine screening. Its primary utility lies in visualizing subclinical HPV-related lesions, aiding in targeted biopsies, and delineating lesion margins during surgical treatments.8
Guidelines for Colposcopy Screening
Colposcopy screening is particularly recommended for specific high-risk populations, including:
- Immunosuppressed transplant recipients
- Women who are HIV-positive
- Women with persistently unclear Pap smear results: specifically, those with three consecutive inadequate samples, or those with a borderline nuclear change in squamous cells after three tests, or a borderline nuclear change in endocervical cells after one test.
- Women with cervical cytology indicating malignant or suspicious cells but a clinically normal-looking cervix.
- Women with persistent mild dyskaryosis (requiring referral after two such test results).
- Women with moderate or severe dyskaryosis (requiring urgent referral, ideally within four weeks).
- Women with cytology suggesting possible invasion or glandular neoplasia (requiring urgent referral, ideally within two weeks).
Biopsy: Histopathological Confirmation
Colposcopy enables targeted tissue sampling (biopsy) from abnormal areas identified during the visual examination. Biopsy is a critical component of HPV diagnosis as it provides a definitive histopathological assessment of the tissue. Treatment decisions are largely based on the severity of abnormalities found in the biopsy sample. Biopsy results can reveal precancerous changes (dysplasia), which are graded as mild, moderate, or severe, or confirm the presence of cancer.
Excisional biopsy is recommended in scenarios where colposcopic findings suggest a high-grade abnormality, when low-grade colposcopic changes are associated with severe dyskaryosis or worse, or when a lesion extends into the cervical canal.
In cases of genital warts, a hallmark microscopic feature is the presence of koilocytes. These are mature squamous cells exhibiting a characteristic clear perinuclear halo. The nuclei of koilocytes may be enlarged, hyperchromatic, and often binucleated.
DNA Techniques: Detecting Viral Genetic Material
Early HPV detection methods relied on direct probe hybridization techniques like dot blot and Southern blot. However, these methods were labor-intensive, time-consuming, lacked sensitivity, and required substantial amounts of DNA from clinical samples. Amplification technologies, particularly Polymerase Chain Reaction (PCR), have largely replaced these earlier methods due to their ability to detect even minute quantities of viral DNA in clinical specimens. Hybridization of viral nucleic acids remains a cornerstone of HPV detection, with two primary techniques widely used:
Hybrid Capture HPV DNA Test 2 (hc2)
The Hybrid Capture 2 (hc2) test, often used in conjunction with the Pap test, is FDA-approved for HPV detection.9 HC2 boasts high sensitivity and specificity, comparable to PCR-based methods, capable of detecting as little as 1 pg of HPV DNA/ml. Its advantages include relatively straightforward handling and reliable reproducibility, making it a well-standardized HPV detection method. While HC2 does not identify the exact HPV type, it can differentiate between “low-risk” (types 6, 11, 42, 43, 44) and “high-risk” (types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) HPV genotype groups (HR HPV and LR HPV).
Polymerase Chain Reaction (PCR)
PCR is a highly sensitive target amplification assay that allows for the exponential and reproducible amplification of HPV DNA sequences present in biological samples. The amplification process is remarkably efficient; theoretically, a billion copies can be generated from a single double-stranded DNA molecule after just 30 amplification cycles.10
Indications for HPV DNA Testing
HPV DNA testing, using methods like HC2 or PCR, is primarily indicated for:
- Primary screening for cervical cancer in conjunction with the Papanicolaou (Pap) test or as a stand-alone test, particularly for women over 30 years of age.
Pap Smear or Pap Test: Cytological Screening
The Pap smear, also known as the Pap test, is a cytological screening test pioneered by Papanicolaou and Traut. It is designed to detect premalignant and malignant cellular changes in the cervix. In addition to cancer screening, the Pap smear can also identify viral infections such as HPV and Herpes. A positive Pap test necessitates further confirmatory investigations, including colposcopy, cervical biopsy, and DNA tests like PCR.
Pap Smear Procedure
During a Pap smear, the patient is positioned in the dorsal position, and the cervix is visualized using a Cusco’s speculum. Cells are gently scraped from the squamocolumnar junction of the cervix using an Ayre’s spatula, rotating it around the circumference. The collected scrapings are then smeared onto a glass slide and immediately fixed with a fixative solution, such as 95% ethyl alcohol and ether, or a fixative spray (cytospray), to preserve cellular morphology. For general cytological evaluation, scrapings may also be taken from the upper lateral part of the vaginal wall.
Revised ACOG Recommendations for Pap Smear Screening11
The American College of Obstetricians and Gynecologists (ACOG) has revised its recommendations for Pap smear screening to optimize effectiveness and reduce over-screening:
- For women aged 21 to 30, screening is recommended every three years instead of every two, using either standard Pap cytology or liquid-based cytology.
- Women aged 30 and older who have had three consecutive negative cervical cytology results may be screened every five years using either Pap cytology or liquid-based cytology combined with HPV testing (co-testing). Alternatively, they can continue screening every three years with cytology alone.
- Women with specific risk factors may require more frequent screening. These risk factors include HIV infection, immunosuppression, in utero exposure to diethylstilbestrol (DES), and a history of treatment for cervical intraepithelial neoplasia (CIN) 2, CIN 3, or cervical cancer.
HPV/HIV Co-infection: Diagnostic Considerations
Intraepithelial neoplasia (IEN) is particularly common in HPV-infected individuals who are also living with HIV/AIDS. Due to the increased risk and often atypical presentation of lesions in this population, clinical markers alone are insufficient for early IEN diagnosis. Therefore, it is crucial to perform biopsies and HPV genotyping on all HIV-positive patients presenting with condylomata acuminata (genital warts) before initiating treatment to guide management and ensure appropriate follow-up.
REFERENCES
[1] Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, et al. International Agency for Research on Cancer Multicentric Cervical Cancer Study Group. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003 Feb 6;348(6):518-27.
[2] zur Hausen H. Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer. 2002 Sep;2(5):342-50.
[3] Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999 Sep;189(1):12-9.
[4] Critchlow CW, Holmes KK, Wølner-Hanssen P, Kiviat NB, Koutsky LA, Stevens CE, et al. Risk factors for human papillomavirus infection and cervical intraepithelial neoplasia in young women. Am J Obstet Gynecol. 1995 Dec;173(6):1703-10.
[5] Bleeker MC, van den Broek IV, van der Sande MA, Voorhoeve M, Berkhof J, Coupé VM, et al. Condom use promotes regression of human papillomavirus-associated penile lesions in men and prevents new infections in their female partners. Sex Transm Infect. 2003 Dec;79(6):447-50.
[6] Ferris DG, Lawhead RA, Wright TC Jr, Kulasingam SL, Kahn JA, Fife K, et al. Colposcopic accuracy in women referred with atypical squamous cells of undetermined significance. Obstet Gynecol. 2000 Dec;96(6):915-20.
[7] Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013 Apr;17(5 Suppl 1):S1-S27.
[8] Shafi MI, Luesley DM. Acetic acid and colposcopy. Best Pract Res Clin Obstet Gynaecol. 2011 Jun;25(3):301-12.
[9] Castle PE, Wright TC Jr, Lorey T, Sharma A, Hurteau J, Mattu R, et al. Two-year persistence of oncogenic human papillomavirus (HPV) types among women with initially negative HPV and Pap test results. J Infect Dis. 2005 Nov 1;192(9):1424-30.
[10] Saiki RK, Gelfand DH, Stoffel S, Scharf SJ, Higuchi R, Horn GT, et al. Primer-directed enzymatic amplification of DNA with a thermostable DNA polymerase. Science. 1988 Jan 29;239(4839):487-91.
[11] American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 514: Cervical cancer screening. Obstet Gynecol. 2011 Dec;118(6):1490-2.