Human papillomavirus (HPV) is a common double-stranded DNA virus belonging to the papillomavirus family. It causes cytopathic effects in epithelial cells. Infections of the genital mucosa are typically persistent, multifocal, and often subclinical. Understanding the Diagnosis Of Human Papillomavirus is crucial for managing and preventing HPV-related diseases.
Over 40 types of HPV are known to be transmitted through sexual contact, primarily infecting the anogenital region.1 While some of these types lead to genital warts, persistent infection with high-risk HPV types, distinct from those causing common skin warts, can progress to precancerous lesions and eventually invasive cancers.2 Notably, HPV infection is the primary cause in the vast majority of cervical cancer cases.3 However, it’s important to remember that most HPV infections, even with high-risk types, do not result in cancer.
HPV transmission occurs through direct skin-to-skin contact. This can happen through various routes: direct contact with skin, such as plantar wart viruses entering broken skin, sexual intercourse, or oral sexual activity and kissing. Symptomatic HPV infection represents only a small portion of the overall picture, as depicted in Figure 1. Asymptomatic shedding of the virus is far more prevalent, particularly in women with HIV/AIDS, and these asymptomatic individuals are significant contributors to viral spread. Studies indicate that asymptomatic HPV/DNA shedding from the perianal region is very common, reaching 78.9% in AIDS patients with advanced disease.4
Figure 1.
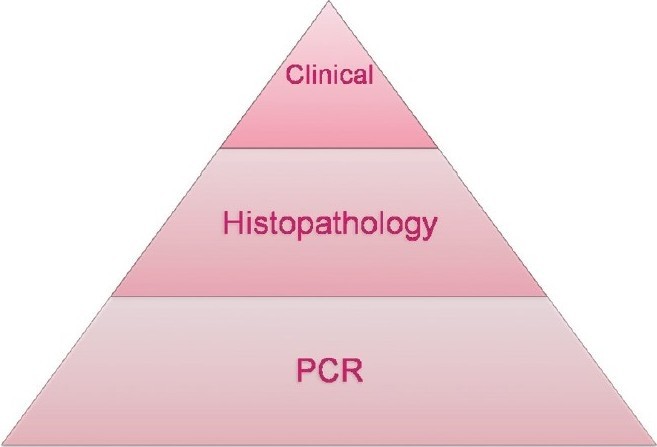 Subclinical, multifocal, and persistent nature of HPV infections
Subclinical, multifocal, and persistent nature of HPV infections
While condom use has not consistently shown to reduce the risk of HPV DNA acquisition (subclinical HPV infection), it has been associated with a decreased risk of genital warts, CIN 2-3, and invasive cervical cancer.5
Laboratory Methods for HPV Diagnosis
Traditional viral diagnostic methods like electron microscopy, cell culture, and certain immunological assays are not practical for HPV detection. HPV cannot be effectively cultured in standard cell cultures. The primary methods employed for the diagnosis of human papillomavirus infection include:
- Colposcopy and Acetic Acid Test
- Biopsy
- HPV DNA Tests (PCR, Southern Blot Hybridization, In Situ Hybridization)
- Pap Smear
Colposcopy and Acetic Acid Test in HPV Diagnosis
Colposcopy is an outpatient procedure performed by trained clinicians using a colposcope, a low-magnification microscope.6 It involves examining the cervix, vagina, and sometimes the vulva after applying an acetic acid solution. This examination is often combined with colposcopically directed biopsies of any lesions suspected of being neoplastic.7 Colposcopic findings are assessed based on the degree of acetowhite lesions, surface contour, mosaic patterns, and punctuation. Greater abnormalities in these parameters are associated with more severe lesions.
Acetic Acid Test Details
The acetic acid test is a valuable adjunct to colposcopy.
- Applying a 3–5% acetic acid-moistened gauze pad to suspicious lesions for 5-10 minutes can enhance suspicion in lesions lacking classic features.
- This method is used on suspected lesions of the penis, cervix, labia, or perianal area.
- Inconspicuous, flat genital lesions that may be difficult to visualize become more apparent as genital warts, dysplastic, and neoplastic tissues turn white (acetowhite).
- It’s crucial to note that false-positive results are common and can arise from conditions causing parakeratosis, such as candidiasis, psoriasis, lichen planus, healing epithelium, and sebaceous glands.
- Therefore, the acetic acid test is not recommended for routine screening.
- Its utility lies in visualizing subclinical genital HPV-associated lesions, identifying target lesions for biopsy, and delineating lesions during surgical treatment.8
Recommendations for Colposcopy Screening
Colposcopy screening is particularly recommended for certain high-risk groups:
- Immunosuppressed transplant recipients.
- Women who are Human Immunodeficiency Virus (HIV) positive.
- Women with a history of abnormal Pap smear results, including:
- Three consecutive inadequate Pap smear samples.
- Borderline nuclear changes in squamous cells after three tests.
- Borderline nuclear changes in endocervical cells after one test.
- Positive cervical cytology for malignant or suspicious cells with a clinically normal-looking cervix.
- Mild dyskaryosis reported in two consecutive tests.
- Moderate or severe dyskaryosis reported in one test (colposcopy within four weeks of referral).
- Possible invasion or glandular neoplasia reported in one test (urgent colposcopy within two weeks of referral).
Biopsy for Definitive HPV Lesion Diagnosis
Colposcopy enables targeted tissue sampling (biopsy) from abnormal areas. Biopsy is a critical component of colposcopy, as treatment decisions depend on the severity of abnormalities observed in the biopsy sample. If biopsy results indicate precancer (dysplasia) or cancer, treatment is recommended. Dysplasia is graded as mild, moderate, or severe.
Excisional biopsy is advised when colposcopic findings suggest high-grade abnormalities, low-grade colposcopic changes are associated with severe dyskaryosis or worse, or when a lesion extends into the cervical canal.
In cases of genital warts, a hallmark feature is the presence of koilocytes. Koilocytes are mature squamous cells exhibiting a clear perinuclear zone. Their nuclei may be enlarged and hyperchromatic, and binucleation is frequently observed.
HPV DNA Testing: Advanced Diagnostic Techniques
Early methods for HPV detection involved direct probe hybridization techniques like dot blot and Southern blot. However, these methods were labor-intensive, time-consuming, had limited sensitivity, and required substantial amounts of DNA from clinical samples. Amplification technologies have largely replaced them, enabling the detection of low viral copy numbers in clinical specimens. Hybridization of viral nucleic acids is now the established routine method for viral detection. Two key techniques are:
Hybrid Capture HPV DNA Test 2 (hc2)
The Hybrid Capture 2 (hc2) test, often used with the Pap test, is FDA-approved.9 It boasts sensitivity and specificity comparable to PCR-based detection methods, capable of detecting as little as 1 pg of HPV DNA/ml. The hc2 test offers advantages in terms of relatively simple handling and good result reproducibility, making it a well-standardized HPV detection method. While it doesn’t identify the exact HPV type, it categorizes HPV genotypes into “low-risk” (6, 11, 42, 43, 44) and “high-risk” (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) groups (HR HPV and LR HPV).
Polymerase Chain Reaction (PCR)
PCR is a selective target amplification assay that allows for exponential and reproducible amplification of HPV sequences present in biological samples. Theoretically, PCR can produce billions of copies from a single double-stranded DNA molecule after 30 amplification cycles.10
Indications for HPV DNA Testing
- Primary screening in conjunction with the Papanicolaou (Pap) test.
- Stand-alone screening test for women over 30 years of age.
Pap Smear (Papanicolaou Test) for Cervical Screening
The Pap smear, developed by Papanicolaou and Traut, is a screening test primarily for cervical cancer and precancerous changes. It can also detect viral infections such as HPV and Herpes. A positive Pap test necessitates further confirmatory tests, including colposcopy, cervical biopsy, and DNA tests like PCR.
Pap Smear Procedure
- The patient is positioned in the dorsal position, and the cervix is exposed using a Cusco’s speculum.
- Scrapings are taken from the squamocolumnar junction using an Ayre’s spatula, rotating it around the cervix.
- The scrapings are spread onto a glass slide and immediately fixed with 95% ethyl alcohol and ether or a fixative spray (cytospray).
- For cytological evaluation related to hormone levels, scrapings can also be taken from the upper lateral part of the vaginal wall.
ACOG Revised Recommendations for Pap Smears 11
The American College of Obstetricians and Gynecologists (ACOG) provides updated recommendations for Pap smear screening:
- Women aged 21 to 30 should be screened every two years using either standard Pap or liquid-based cytology, instead of annually.
- Women aged 30 and older with three consecutive negative cervical cytology results may be screened every three years with either Pap or liquid-based cytology.
- Women with certain risk factors require more frequent screening, including those with HIV, immunosuppression, in utero exposure to diethylstilbestrol (DES), or a history of treatment for cervical intraepithelial neoplasia (CIN) 2, CIN 3, or cervical cancer.
HPV/HIV Co-infection Considerations
Intraepithelial neoplasia (IEN) is frequently observed in HPV-infected patients with HIV/AIDS. As there are no reliable clinical markers to diagnose early IEN, biopsy and HPV genotyping are recommended for all HIV-positive patients with condylomata acuminata (genital warts) before initiating treatment.
REFERENCES
[1] Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003 Feb 6;348(6):518-27.
[2] zur Hausen H. Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer. 2002 May;2(5):342-50.
[3] Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999 Sep;189(1):12-9.
[4] Critchlow CW, Widdice LE, Holmes KK, Cone RW, Gitnick G, Band PR, et al. Asymptomatic shedding of human papillomavirus types 6, 11, 16, and 18 in men. J Natl Cancer Inst. 1992 Nov 4;84(21):1658-63.
[5] Bleeker MC, Hogewoning CJ, Voorhorst FJ, van den Brule AJ, Snijders PJ, Voorst Vader PC, et al. Condom use and risk of prevalent human papillomavirus infection and cervical intraepithelial neoplasia in young women. JAMA. 2003 Oct 15;290(10):1246-53.
[6] Singer A, Monaghan JM, Quek R, Greco C. Colposcopy and Treatment of Cervical Intraepithelial Neoplasia: A Beginner’s Manual. Wiley-Blackwell; 2011.
[7] Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013 Apr;17(5 Suppl 1):S1-27.
[8] Ferris DG, Cox JT, Miller DM, Mueller LJ, Musco SJ, Richart RM, et al. Acetic acid wash as a cervical cancer screening test. Obstet Gynecol. 2006 Feb;107(2 Pt 1):309-16.
[9] Castle PE, Schiffman M. Human papillomavirus type 16 and 18 tests and risk for cervical cancer. Obstet Gynecol. 2003 Dec;102(6):1313-7.
[10] Saiki RK, Gelfand DH, Stoffel S, Scharf SJ, Higuchi R, Horn GT, et al. Primer-directed enzymatic amplification of DNA with a thermostable DNA polymerase. Science. 1988 Jan 29;239(4839):487-91.
[11] American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 109: Cervical cytology screening. Obstet Gynecol. 2009 Dec;114(6):1409-20.