Poststreptococcal glomerulonephritis (PSGN) is a condition characterized by a swift decline in kidney function. This deterioration is triggered by an inflammatory response that follows a streptococcal infection. Specifically, PSGN emerges typically in children, approximately 1 to 2 weeks after a streptococcal throat infection, or within about 6 weeks following a streptococcal skin infection. Clinically, PSGN often manifests with nephritic syndrome features, including hematuria, oliguria, hypertension, and edema. However, it’s important to note that significant proteinuria can also be a presenting sign. This article delves into the diagnosis of PSGN, covering its etiology, pathogenesis, evaluation methods, and management strategies, aiming to provide a thorough understanding for healthcare professionals.
Understanding Post Streptococcal Glomerulonephritis
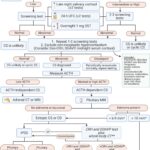
Poststreptococcal glomerulonephritis (PSGN) is marked by a rapid decline in kidney function due to an inflammatory response, specifically a type III hypersensitivity reaction, following a streptococcal infection. (See Image. Poststreptococcal glomerulonephritis). This condition arises from particular strains of group A beta-hemolytic streptococci, known as nephrogenic streptococci. PSGN affects the glomeruli and the small blood vessels within the kidneys. It commonly appears in children around 1 to 2 weeks after a streptococcal sore throat, or up to 6 weeks after a skin infection like impetigo.[1]
While PSGN incidence has decreased in developed nations, infections from non-streptococcal organisms are becoming more prevalent. Nephritis-associated plasmin receptor (NAPlr) and streptococcal pyrogenic exotoxin B (SPeB) are key antigens involved in PSGN pathogenesis. These antigens activate the alternate complement pathway, leading to hypocomplementemia, and exhibit an affinity for plasmin and glomerular proteins. PSGN’s clinical presentation can range widely from asymptomatic cases to severe renal failure requiring renal replacement therapy (RRT). [2]
Symptomatic PSGN typically presents with nephritic syndrome features like hematuria, oliguria, hypertension, and edema. In less frequent cases, it may resemble nephrotic syndrome with significant proteinuria.
Etiology of Post Streptococcal Glomerulonephritis
PSGN is preceded by an infection with nephrogenic streptococci, initially affecting the skin or oropharynx. Recent data indicates that skin infections (impetigo) are more frequently associated with PSGN compared to throat infections (pharyngitis).[3][4]
Group A Streptococcus (GAS) subtypes, categorized by surface M protein and opacity factor, are nephrogenic and known to induce PSGN. Other causes of post-infectious glomerulonephritis include bacterial infections such as endocarditis, enterocolitis, pneumonia, and intraventricular shunt infections, as well as viral infections like hepatitis B and C, HIV, cytomegalovirus, Epstein Barr virus, and parvovirus B19. Fungal infections (coccidioidomycosis, histoplasmosis) and parasitic infections (malaria, leishmania, toxoplasmosis, schistosomiasis) are also implicated.[5]
Risk factors for streptococci outbreaks, such as poor hygiene, overcrowding, and low socioeconomic status, contribute to a higher PSGN incidence in less developed countries. Genetic predisposition is suggested by family history in approximately 40% of PSGN patients, although no specific causative gene has been identified.[5]
Epidemiology of Post Streptococcal Glomerulonephritis
The incidence of PSGN has significantly decreased in developed countries over the past three decades, including the United States, UK, Central Europe, and Japan. This decline is attributed to antibiotic prophylaxis and improved hygiene. In these regions, PSGN is now more commonly observed in adults with chronic debilitating conditions.[6]
In contrast, developing countries experience a higher PSGN incidence, primarily due to increased skin infections (pyoderma). Despite the reduced incidence in developed countries, PSGN remains the most common cause of glomerulonephritis (GN) in children in the United States.[5]
PSGN is also the leading cause of kidney injury in children across the Middle East, Africa, Australia, and globally. The annual incidence in developing countries ranges from 8.5 to 28.5 new cases per 100,000 individuals.[7] Approximately 97% of reported PSGN cases are from underprivileged countries.
Clinically, PSGN is more prevalent in males than females, with a 2:1 ratio. However, subclinical PSGN incidence is nearly equal in both sexes. Racial factors do not appear to play a significant role. The disease most commonly affects children aged 3 to 12 years, with peak incidence between 5 and 6 years, and seniors over 60 years old.
Pathophysiology of Post Streptococcal Glomerulonephritis
PSGN is an immunological disease, classified as a type III hypersensitivity reaction. The precise mechanism of PSGN development is not fully understood. The body’s immune response to nephrogenic streptococcal infection involves forming immune complexes of streptococcal antigens and human antibodies.[2] Theories propose that these immune complexes deposit in kidney glomeruli via circulation. Alternatively, PSGN may result from “in situ” formation of antigen-antibody complexes within the kidney glomeruli. This “in situ immune complex formation” may occur due to a reaction against streptococci antigens deposited in the glomerular basement membrane or, as other theories suggest, from an antibody reaction against glomerular components that cross-react with streptococcal antigens through molecular mimicry.[5]
Immune complex presence activates the alternate complement pathway, causing leukocyte infiltration and mesangial cell proliferation in the glomerulus. This impairs capillary perfusion and glomerular filtration rate (GFR). Reduced GFR can lead to renal failure (oliguria or anuria), acid-base imbalance, electrolyte abnormalities, volume overload, edema, and hypertension.
Histopathology in Diagnosis of Post Streptococcal Glomerulonephritis
Histopathological examination is crucial in understanding and diagnosing PSGN, although renal biopsy is not routinely recommended for typical cases.
- Light microscopy: Glomeruli display hypercellularity involving endothelial, mesangial, and inflammatory cells, which are non-specific findings.
- Electron microscopy: The hallmark is the presence of sub-epithelial humps, electron-dense deposits in the subepithelial space near the glomerular basement membrane.[8]
- Immunofluorescence microscopy: Shows IgG and C3 deposits within the first 2 to 3 weeks of the disease.
History and Physical Examination in Diagnosis of Post Streptococcal Glomerulonephritis
Around 50% of children with PSGN are asymptomatic, with diagnosis occurring incidentally through routine urine analysis. The classic glomerulonephritis triad includes hematuria, edema, and hypertension. Typically, patients report a recent streptococcal infection, such as pharyngitis, tonsillitis, or impetigo. However, PSGN can develop without apparent respiratory or skin infection symptoms, posing a diagnostic challenge.[9]
Gross hematuria is the most common presenting symptom, occurring in 30 to 50% of acute PSGN cases. Patients often describe urine as smoky, tea-colored, cola-colored, or rusty. Hematuria can be postpharyngitic, appearing weeks after infection.
Renal involvement is common and typically transient, resolving within 1-2 weeks. Oliguria occurs in less than half of patients. Severe renal involvement can lead to anuric renal failure, life-threatening acid-base imbalance, electrolyte abnormalities (hyperkalemia), and fluid overload, necessitating RRT. Hypertension affects 60-80% of patients, usually resolving within 10 days.[5]
Edema is present in 65-90% of cases. Periorbital edema, puffiness around the eyelids, is typical of nephritic syndrome, most prominent in the morning and decreasing by day’s end. Generalized edema is also common. Severe cases may involve respiratory distress from pulmonary edema. Non-specific symptoms like anorexia, malaise, nausea, and vomiting may also occur.
Evaluation and Diagnostic Approach for Post Streptococcal Glomerulonephritis
Suspect PSGN in children with hypertension and heart failure, even without hematuria or a history of preceding sore throat or pyoderma.
Laboratory investigations are paramount in PSGN diagnosis.
-
Streptococcal Infection Evidence: Assess preceding streptococcal infection by measuring anti-streptolysin O (ASO) titer and anti-nicotinamide-adenine dinucleotidase (anti-NAD), which increase after pharyngitis. Antibodies like anti-DNAse B and anti-hyaluronidase (AHase) elevate after both pharyngitis and skin infections. ASO titer is frequently used, but the streptozyme test, measuring titers of all mentioned antibodies, is most sensitive. ASO titers may be falsely low in antibiotic-treated streptococcal infections.
-
Urine Analysis: Shows macroscopic or microscopic hematuria, RBC casts, and mild proteinuria. Massive proteinuria indicating nephrotic syndrome is rare (5% of patients). White blood cell casts, hyaline, and cellular casts may be present.
-
Renal Function Tests: Blood urea nitrogen (BUN) and serum creatinine typically rise during the acute phase, usually returning to normal later.
-
NT-proBNP Levels: Elevated in PSGN patients with heart failure, alongside pulmonary congestion findings on chest x-ray.
Renal biopsy is not routinely recommended for PSGN diagnosis and is reserved for cases with suspected alternative glomerular pathologies. Indications for renal biopsy include:
- Progressive decline in renal function
- Anuric renal failure
- Absence of a latent period between acute glomerulonephritis and streptococcal infection
- Normal complement levels
- No elevation in antistreptococcal antibodies
Imaging Studies:
- Ultrasonography: Kidneys may be enlarged in some patients.
- Chest X-ray: May reveal pulmonary congestion in patients with volume overload or heart failure symptoms.
Treatment and Management Strategies for Post Streptococcal Glomerulonephritis
PSGN is typically self-limiting, requiring primarily symptomatic treatment. Supportive care focuses on managing volume overload complications like hypertension and edema, which are prominent during the acute phase.[5]
Pharmacological Therapy:
- Antimicrobials: Antibiotic therapy is indicated for patients with evidence of ongoing streptococcal infection, although it may not prevent PSGN development.
- Diuretics: Loop diuretics (furosemide) are preferred over thiazides (hydrochlorothiazide or chlorthalidone) due to better efficacy when GFR is reduced.
- Antihypertensive medications: Manage blood pressure with salt and fluid restriction and diuretics. Calcium channel blockers are recommended for uncontrolled hypertension. ACE inhibitors and ARBs are suitable for patients with stable GFR and near-normal potassium levels.
- Immunosuppressive therapy: Not generally indicated for PSGN.[10] Corticosteroids may be considered in cases of progressive renal failure or crescent formation on renal biopsy.[11]
Dialysis:
Dialysis is used to manage acid-base balance, electrolyte abnormalities (especially hyperkalemia), and fluid overload.
General Measures:
- Salt and water restriction to manage edema.
- Bed rest and immobilization during the initial days.
- Throat cultures for patient and family members.
- Treatment of affected family members with penicillin or erythromycin.
Differential Diagnosis of Post Streptococcal Glomerulonephritis
Accurate diagnosis of PSGN requires differentiation from other conditions presenting with similar symptoms:
- IgA Nephropathy: Occurs post-upper respiratory or gastrointestinal infection, but with a shorter latency period than PSGN. Synpharyngitic hematuria (hematuria coinciding with infection) is characteristic.
- Membranoproliferative glomerulonephritis: Presents with nephritic syndrome and hypocomplementemia post-respiratory infection. Complement levels take longer to normalize than in PSGN, or C3 levels remain persistently low.
- Lupus nephritis: Can mimic PSGN. Antibody testing specific to each disease aids differentiation. Lupus nephritis is indicated by positive ANA, ds-DNA, cytopenia, and multi-organ involvement.
- Nephrotic syndrome: Characterized by >3.5 g/day proteinuria, hypoalbuminemia, edema, hypogammaglobulinemia, and increased thrombosis risk.
- Henoch Schonlein purpura (HSP): Presents with palpable purpura, renal failure, gastrointestinal, and musculoskeletal symptoms. Complement levels are typically normal.
- Hemolytic uremic syndrome (HUS): Labs show hemolysis (schistocytes, elevated LDH, reticulocyte count, indirect bilirubin), bloody diarrhea, thrombocytopenia, and positive stool culture for Escherichia coli O157:H7.
- ANCA-associated vasculitis: Normal complement levels.
- Goodpasture disease: Involves lungs and kidneys, with anti-glomerular basement antibody and normal complement levels.
Prognosis of Post Streptococcal Glomerulonephritis
PSGN prognosis is generally excellent, particularly in children, with complete recovery within 6 to 8 weeks. Adults may experience persistent reduced renal function, hypertension, or proteinuria in about 50% of cases.[12][13]
Adult mortality is often due to heart failure and renal dysfunction. Long-term studies indicate some patients may continue to have urine abnormalities, proteinuria, and hypertension.
Mortality during the acute phase is estimated between 2 and 12 percent. Renal changes in survivors are presumed similar to those in fatal cases, although direct evidence is limited.[14]
Complications of Post Streptococcal Glomerulonephritis
Acute phase complications include congestive heart failure and azotemia, which can be life-threatening. Delayed complications involve chronic kidney disease and nephrotic syndrome.
Consultations for Post Streptococcal Glomerulonephritis
- Nephrology consultation is essential for managing PSGN.
Deterrence and Patient Education for Post Streptococcal Glomerulonephritis
Preventive measures include avoiding overcrowding and maintaining personal hygiene to reduce streptococcal infection risk.
Patients with throat or skin infections should seek prompt medical advice and antibiotic therapy if bacterial infection is confirmed.
Enhancing Healthcare Team Outcomes in Post Streptococcal Glomerulonephritis Management
Effective PSGN management requires interprofessional collaboration between internists, nephrologists, infectious disease specialists, pharmacists, and nursing staff. Careful monitoring of fluid and salt intake, and urine output is crucial. Pharmacists ensure patients avoid nephrotoxic medications and emphasize medication adherence for hypertension. Nurses should encourage throat swabs for close contacts and family members and monitor for worsening edema. Renal function and potassium levels require close monitoring.
Nephrology consultation, particularly with a pediatric nephrologist for children, is necessary for complex cases. Regular monitoring of fluid and electrolyte status is needed. Effective communication among team members is vital for optimal outcomes. [Level 5]
Prognosis in children is excellent, but adults may have a prolonged course with 30 to 50% developing renal dysfunction and hypertension.[15][16] [Level 5]
Review Questions
Figure
Poststreptococcal Glomerulonephritis
References
[List of references as in the original article]
Disclosures: