Renal Tubular Acidosis (RTA) refers to a group of disorders characterized by metabolic acidosis resulting from defects in renal tubular function. Accurate diagnosis of RTA is crucial for effective management and hinges on a series of confirmatory tests that assess the kidney’s ability to regulate acid-base balance. These tests primarily involve the urinary measurement of indices related to acid and bicarbonate secretion. To effectively interpret these diagnostic approaches, a thorough understanding of the fundamental acid-base disturbances in different RTA types is essential. This knowledge guides clinicians in selecting the most appropriate provocation tests to confirm the diagnosis.
Understanding the pathophysiology of each RTA type is paramount for targeted diagnosis. Distal RTA is marked by a defect in the distal tubules, impairing the excretion of hydrogen ions (H+). Proximal RTA, conversely, involves an issue with bicarbonate (HCO3−) reabsorption in the proximal tubules, leading to decreased serum HCO3− and pH. Hyperkalemic RTA, often associated with hypoaldosteronism, arises from reduced aldosterone activity, whether due to insufficient aldosterone secretion (primary or secondary adrenal insufficiency) or renal resistance to aldosterone. Hyperkalemic RTA is diagnosed when this aldosterone deficiency disrupts acid-base balance, resulting in a normal anion gap metabolic acidosis. This acidosis is believed to be exacerbated by hyperkalemia, which hinders urinary ammonium (NH4+) excretion.5,10,11
Differentiating hyperkalemic RTA from distal and proximal RTA is generally straightforward. Hyperkalemic RTA is readily identified by the presence of hyperkalemia and serum aldosterone measurements, particularly when the glomerular filtration rate (GFR) is near normal. Serum aldosterone levels can be variable, either high or low, depending on the underlying cause of hypoaldosteronism. However, distinguishing between proximal and distal RTA necessitates specific diagnostic methodologies.
Diagnostic Tests for Proximal RTA
The bicarbonate (HCO3−) loading test (see sidebar below) is a key diagnostic tool for confirming proximal RTA.12,13 This test is predicated on the principle that in patients with acidemia, characterized by low plasma HCO3− concentration, and normal proximal tubular function, the administration of HCO3− should not significantly alter urine HCO3− levels. This is because the HCO3− will be efficiently reabsorbed from the urine. In contrast, patients with proximal RTA exhibit impaired HCO3− reabsorption, leading to a noticeable rise in urinary HCO3− concentration following HCO3− infusion.
In cases where patients present with markedly low serum HCO3− and metabolic acidosis, a single urinary measurement of the fractional excretion of HCO3− can sometimes be sufficient to diagnose proximal RTA, obviating the need for a formal HCO3− loading test. Under normal physiological conditions, when serum HCO3− is low, the kidneys are expected to exhibit vigorous urinary HCO3− reabsorption, resulting in a very low fractional excretion of HCO3− (typically <3%). However, in proximal RTA, this fractional excretion will be inappropriately elevated (often >15%). Despite its utility, it’s important to note that the HCO3− loading test remains the gold standard for definitive diagnosis of proximal RTA when clinical suspicion is high but initial tests are inconclusive.
Diagnostic Tests for Distal RTA
For the definitive diagnosis of distal RTA, the ammonium chloride (NH4Cl) loading test (see sidebar below) is considered the gold standard.14,15 Administering an acid load in the form of NH4Cl to a healthy individual with normal kidney function should result in urine acidification as the kidneys work to buffer blood pH. In patients with distal RTA, who have impaired urinary H+ and NH4+ secretion, urinary pH will not decrease to the expected acidic levels following NH4Cl administration.
Unlike the HCO3− loading test for proximal RTA, direct measurement of NH4+ concentration in urine is not clinically feasible. Therefore, the urine anion gap (UAG) serves as a valuable surrogate marker for NH4+ secretion.
The UAG is typically positive in healthy individuals, mirroring the serum anion gap. It is calculated by subtracting urine chloride (Cl−), an anion, from the sum of urinary cations, specifically sodium (Na+) and potassium (K+): UAG = (Na+ + K+) – Cl−. The normal UAG range is approximately 20-90 mEq/L. Kidneys acidify urine by secreting NH4+, which is often secreted alongside Cl−. Thus, urinary Cl− provides an indirect measure of NH4+ excretion. In individuals with properly functioning nephrons, the UAG becomes less positive and can even become negative after NH4Cl administration due to increased NH4+ secretion accompanied by increased urinary Cl− excretion. Conversely, patients with impaired NH4+ excretion in distal RTA will maintain an inappropriately positive UAG, even after acid loading.
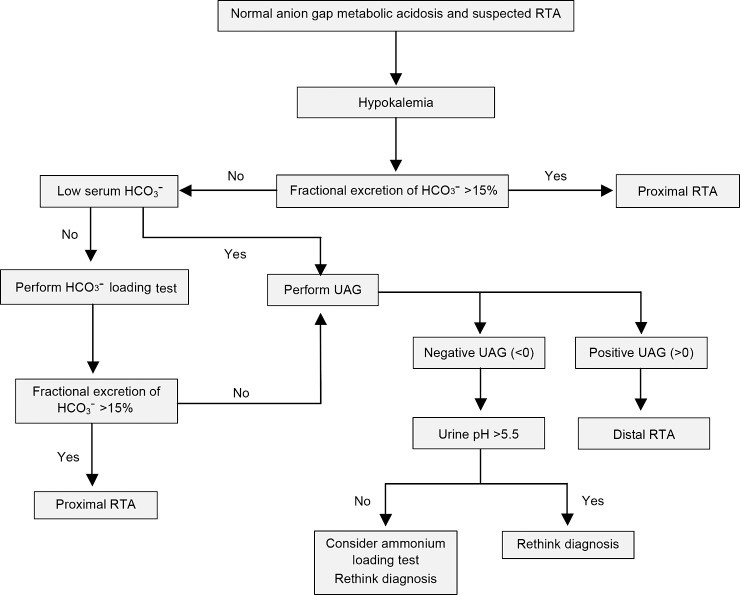
While the NH4+ loading test remains the definitive diagnostic test for distal RTA, it can sometimes be bypassed in patients presenting with clear hyperchloremic metabolic acidosis and an inappropriately high urine pH. In such instances, a single UAG measurement might be sufficient to confirm distal RTA (Figure 1).16 It is crucial to remember that the NH4+ loading test aims to induce acidosis; therefore, it is unnecessary and potentially risky in patients who are already acidemic. The test must be conducted cautiously due to potential adverse effects such as nausea, vomiting, or cardiac dysrhythmias.
Figure 1.
Figure 1: Suggested algorithm for suspected renal tubular acidosis (RTA) in patients with non–anion gap metabolic acidosis and hypokalemia. HCO3−, bicarbonate; UAG, urine anion gap. This algorithm outlines a diagnostic approach starting with initial blood and urine tests, guiding clinicians through steps to differentiate RTA types and reach a definitive diagnosis.
Differentiating Distal RTA from Diarrhea
The UAG also plays a crucial role in distinguishing between distal RTA and diarrhea as causes of hyperchloremic metabolic acidosis. Patients experiencing diarrhea with intact urinary acidification mechanisms are expected to exhibit a negative UAG. However, interpretation of UAG results must be cautious in patients with volume depletion. Hypovolemia, often associated with diarrhea, can lead to increased sodium (Na+) reabsorption in the proximal tubules. This, in turn, reduces Na+ delivery to the distal nephron and consequently diminishes distal Na+-dependent negative potential difference, impairing distal hydrogen and ammonium excretion and may falsely elevate the UAG.17
In conclusion, the Diagnosis Of Renal Tubular Acidosis requires a systematic approach, utilizing specific loading tests and urinary indices like the urine anion gap. Understanding the underlying pathophysiology of each RTA type and carefully interpreting test results in the clinical context is essential for accurate diagnosis and appropriate patient management.