Compromised shoulder movement stemming from pain, stiffness, or weakness can significantly impair daily activities and work capabilities. Shoulder pain is a prevalent issue, estimated to affect 16% to 26% of the population, making it the third most common musculoskeletal complaint in primary care settings. Annually, approximately 1% of adults consult their general practitioner for new-onset shoulder pain. Occupations involving heavy lifting, repetitive motions in awkward postures, and exposure to vibrations are linked to a higher incidence of shoulder disorders. Furthermore, psychosocial factors play a crucial role in symptom severity and disability. Recent studies indicate that chronicity and recurrence of shoulder problems are frequently observed.
The diagnostic process for common shoulder disorders is often complicated by overlapping clinical presentations, a lack of standardized diagnostic criteria, and inconsistencies in clinical assessments, which in turn can hinder effective treatment planning. This review aims to present an evidence-based, simplified approach to classifying shoulder problems, incorporating diagnostic techniques suitable for primary care consultations, and a “red flag” system to identify potentially serious underlying conditions.
Sources and Selection Criteria
This review is based on the latest consensus derived from systematic reviews and publications identified through a comprehensive literature search across Medline, CINAHL, AMED, the Cochrane Library, Clinical Evidence, Best Evidence, Embase, British Nursing Index, PEDro, Web of Science, and bmj.com. Search terms included “shoulder pain,” “rotator cuff disorder,” “rotator cuff tear,” “frozen shoulder,” and “primary care.”
The search yielded six systematic reviews on interventions for shoulder disorders and one health technology assessment systematic review focusing on diagnostic tests for shoulder pain assessment. A topic search within Clinical Evidence also provided relevant information under “Shoulder pain.” Additional key publications in peer-reviewed journals, pertinent to primary care or published after the latest systematic reviews, were identified and critically evaluated.
Summary Points
- Shoulder disorders are frequently mixed, and overly specific diagnostic categorization does not substantially alter the primarily conservative management approach in primary care.
- Self-management advice, including relative rest and addressing contributing factors from occupation, sports, or other physical activities, along with analgesics, should be the initial recommendations.
- Evidence supporting common interventions like steroid injections and physiotherapy is relatively limited.
- Physiotherapy may reduce the need for repeat primary care consultations for rotator cuff disorders, while steroid injections offer a modest short-term pain relief effect.
- Factors associated with poorer prognosis include older age, female gender, severe or recurrent symptoms at initial presentation, and concurrent neck pain.
- Surgical intervention should be considered when conservative treatments are unsuccessful.
Assessment of the Painful Shoulder
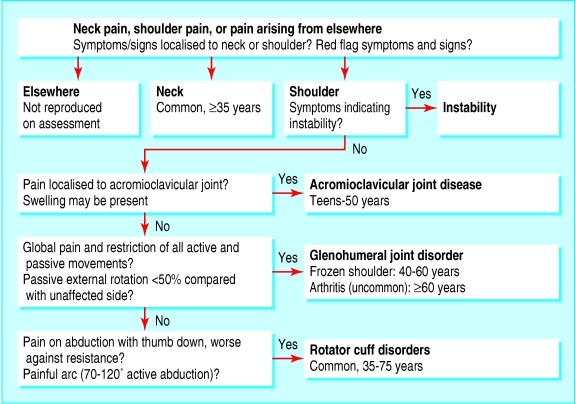
Diagnosis should be practical and grounded in clinical assessment (Box 1), categorizing patients based on common presentations in primary care (Figure 1). An excessively complex diagnostic approach is unlikely to change the initial conservative management strategies typically employed in primary care.
Figure 1. Diagnostic Algorithm for Shoulder Problems in Primary Care
Click to enlarge image
Adapted with permission from shoulder pain algorithm: www.oxfordshoulderandelbowclinic.org.uk
The four most prevalent causes of shoulder pain and disability in primary care are rotator cuff disorders, glenohumeral joint disorders, acromioclavicular joint disease, and referred pain from the neck (Box 2).
A primary care study utilizing standardized clinical tests for shoulder disorders identified rotator cuff tendinopathy in 85% of patients. Notably, 77% of patients received a clinical diagnosis of more than one shoulder problem, such as tendinosis and impingement (57%), or tendinosis, impingement, acromioclavicular disease, and adhesive capsulitis (6%). Blood tests and radiography are only indicated in the presence of “red flag” indicators, including symptoms and signs of systemic disease (weight loss, generalized joint pain, fever, lymphadenopathy, new respiratory symptoms), a history of cancer, or concerning local features like a mass lesion or bony tenderness or swelling (Box 3).
Rotator Cuff Disorders (Age 35-75)
Rotator cuff tendinopathy is the most frequent cause of shoulder pain. Occupational history may reveal factors like heavy lifting or repetitive overhead movements. While activity-related, it commonly affects the non-dominant arm and individuals in non-manual occupations. Genetic predisposition is suggested by evidence in some families. Examination may reveal muscle wasting; active and resisted movements are painful and potentially restricted, whereas passive movements are typically full, albeit painful. Although a painful arc is not a highly specific or sensitive clinical sign, its presence supports the diagnosis of a rotator cuff disorder.
A rotator cuff tear is often strongly suspected based on patient history: traumatic in younger individuals and atraumatic in older individuals (related to wear and tear from bone spurs on the acromion or intrinsic cuff degeneration). Partial tears can be challenging to distinguish from rotator cuff tendinopathy through examination alone; weakness during resisted movement can occur in both conditions. Studies suggest no direct correlation between symptoms and functional loss in cases of full-thickness supraspinatus tears. Tears of the lower rotator cuff may result in limited external rotation (beyond 20°). Furthermore, partial and full-thickness tears are commonly found in imaging studies of asymptomatic individuals. The “drop arm test” can be used to identify large or complete tears, although its specificity is high but sensitivity low in secondary care populations.
Box 1: History and Examination of the Shoulder Joint for Accurate Diagnosis
History Taking for Shoulder Pain Diagnosis
- Onset, characteristics, and functional impact of shoulder pain?
- Dominant/non-dominant hand affected?
- Is pain present at rest, during movement, or both?
- Is pain experienced at night?
- Does pain affect sleeping position?
- Presence of neck, thoracic, or other upper limb pain?
- History of acute trauma, prior shoulder pain, or instability (dislocations or subluxations)?
- Occupation and sporting activities relevant to shoulder strain?
- Involvement of other joints?
- Systemic symptoms of illness (fever, weight loss, rash, respiratory issues)?
- Significant comorbidities (diabetes, stroke, cancer, respiratory, gastrointestinal, renal disease, ischemic heart disease, psoriasis)?
- Current medications and any adverse drug reactions?
Physical Examination Techniques for Shoulder Diagnosis
- Examine neck, axilla, and chest wall to rule out referred pain or other conditions.
- Assess cervical spine range of motion to identify neck involvement.
- Inspect shoulders for swelling, muscle wasting, and deformities.
- Palpate sternoclavicular, acromioclavicular, and glenohumeral joints for tenderness, swelling, warmth, and crepitus.
- Compare strength, stability, and range of motion (active, passive, resisted) of both shoulders.
- Evaluate for painful arc (70-120° active abduction).
- Test passive external rotation to assess for restrictions.
- Perform “Drop arm test”: assess patient’s ability to slowly lower abducted arm to waist, indicating rotator cuff integrity.
Box 2: Common Causes of Shoulder Pain in Primary Care
Shoulder Pain Arising from the Shoulder Joint
- Rotator cuff disorders: tendinopathy, impingement, subacromial bursitis, rotator cuff tears
- Glenohumeral disorders: adhesive capsulitis (“frozen shoulder”), osteoarthritis
- Acromioclavicular joint disease
- Infection (rare but important to consider)
- Traumatic dislocation
Shoulder Pain Arising from Elsewhere (Referred Pain)
- Referred pain: neck pain, myocardial ischemia, diaphragmatic pain
- Polymyalgia rheumatica
- Malignancy: apical lung cancers, metastases
Box 3: Red Flag Indicators for Serious Shoulder Conditions
- History of cancer; symptoms and signs suggestive of cancer; unexplained deformity, mass, or swelling: rule out tumor.
- Red skin, fever, systemic illness: consider infection as a potential cause.
- Trauma, epileptic seizure, electric shock; loss of rotation and abnormal shoulder shape: suspect unreduced dislocation.
- Trauma, acute disabling pain and significant weakness, positive drop arm test: evaluate for acute rotator cuff tear.
- Unexplained significant sensory or motor deficit: investigate for neurological lesion.
Glenohumeral Disorders (Adhesive Capsulitis: Age 40-65, Median 50-55; Osteoarthritis: ≥60)
Adhesive capsulitis (“frozen shoulder”) and true glenohumeral arthritis often follow non-adhesive capsulitis symptoms. Both are characterized by deep joint pain and restricted activities like putting on a jacket (due to impaired external rotation). Adhesive capsulitis is more prevalent in individuals with diabetes and may occur after prolonged immobilization. Examination reveals global pain and restriction of all movements, both active and passive.
Acromioclavicular Disease (Teenage to 50)
Acromioclavicular disease typically results from trauma or osteoarthritis. Dramatic joint dislocation can occur after injury, particularly in teenagers to 30-year-olds. Pain, tenderness, and occasional swelling are localized to the acromioclavicular joint. Restriction of passive horizontal adduction (flexion) of the shoulder across the body with an extended elbow is characteristic. Acromioclavicular osteoarthritis can also contribute to subacromial impingement.
Referred Mechanical Neck Pain (Common)
Referred neck pain typically presents with pain and tenderness in the lower neck and suprascapular area, radiating to the shoulder and upper limb. Shoulder movement may be limited. Cervical spine and shoulder movements can reproduce generalized upper back, neck, and shoulder pain. Upper limb paresthesia may occur. Treatment involves relative rest, analgesia, and encouragement to return to normal activities. Physiotherapy can be beneficial.
Treatment Strategies for Shoulder Pain in Primary Care
A functional and holistic approach to shoulder pain management, including adequate pain relief, is crucial for patient motivation and rehabilitation. However, evidence supporting common primary care interventions, such as steroid injections, is relatively weak. The primary care physician should determine if the pain originates from the shoulder or is referred from elsewhere. If referred, appropriate treatment and referral should be initiated.
If the pain is shoulder-related, differentiate between rotator cuff disorders and glenohumeral joint problems. For both, analgesics (preferably paracetamol; NSAIDs as second-line if no contraindications exist and used intermittently), activity encouragement, and provision of written information (e.g., patient leaflets from arthritis organizations) are recommended.
Rotator Cuff Disorders (Including Possible Minor Tears) Management
Initial treatment for rotator cuff disorders involves relative shoulder rest. Patients should resume normal or modified work and activities as soon as possible, within pain and disability limits. Systematic reviews and recent studies suggest comparable short-term benefits for physiotherapy (including supervised exercise) and steroid injections in managing shoulder disorders. In primary care settings with undifferentiated shoulder disorders, patients receiving physiotherapy were less likely to re-consult their general practitioner compared to those treated with steroid injections alone.
A recent study indicated that subacromial xylocaine injection was as effective as steroid plus xylocaine for all disease-specific outcomes at two weeks, with follow-up at 6, 12, and 24 weeks. Some practitioners advocate larger injection volumes (up to 10 ml) for potential hydrodilatation of the subacromial bursa. However, evidence evaluating outcomes with varying injection volumes is limited. Therefore, subacromial corticosteroid injections, up to 10 ml, can be considered for short-term pain relief and to facilitate rehabilitation. If the initial response is positive, injections can be repeated up to three times at six-week intervals. Steroid injections are not proven to be beneficial or harmful in the presence of a rotator cuff tear and should be avoided if the drop arm test is positive.
Glenohumeral Disorders Management
Traditionally, frozen shoulder is believed to resolve naturally within two years, but symptoms can persist for three or more years, particularly in patients with diabetes mellitus. Intra-articular corticosteroid injections (anterior approach) may alleviate pain in the early phase. Physiotherapy alone is not consistently shown to benefit adhesive capsulitis; movement can be painful and counterproductive when the joint is severely inflamed. Intra-articular corticosteroid injections followed by physiotherapy starting a week later may offer short-term benefit. However, studies using fluoroscopy-guided intra-articular injections may have limited generalizability to primary care settings.
Acromioclavicular Disorders Management
Acromioclavicular disorders typically improve with rest and simple analgesia, unless significant traumatic dislocation is present. Persistent symptoms may benefit from local steroid injections.
Biopsychosocial and Complementary Interventions
Psychosocial factors like passive coping, fear of movement, and psychological distress can increase the risk of chronic symptoms in back and neck pain. Similar interventions targeting these and occupational factors have been suggested for shoulder disorders. However, a systematic review found limited evidence that multidisciplinary biopsychosocial rehabilitation is superior to “usual care” for shoulder problems in working-age adults.
Acupuncture is the most studied complementary therapy. Systematic reviews of small and methodologically diverse studies provide limited evidence to support or refute acupuncture for shoulder disorders. Some studies suggest acupuncture may improve pain and function in the short term (two to four weeks).
Further Investigation and Imaging
Ultrasound and MRI are reported as valuable diagnostic tools in secondary care, potentially enhancing diagnostic specificity. However, early access to these investigations is unlikely to improve the management of heterogeneous shoulder disorders typically managed conservatively. Surgical intervention, guided by advanced imaging, is rarely necessary. Structural abnormalities can be present in asymptomatic patients, and early imaging may paradoxically increase specialist referrals.
Referral Criteria to Orthopedic Specialist
Referral to an orthopedic specialist is recommended in the following scenarios:
- Persistent pain and significant disability lasting over six months despite conservative management, including addressing occupational/sporting factors, physiotherapy, and steroid injections if indicated.
- History of shoulder instability (“Has your shoulder ever dislocated?” “Are you concerned about shoulder slippage during movements?”) or acute, severe post-traumatic acromioclavicular pain.
- Diagnostic uncertainty or presence of red flag criteria (Box 3).
Patient’s Perspective
“My right shoulder problem began about six months ago, possibly after an awkward position while caring for my father. The pain gradually worsened, disrupting my sleep and limiting arm elevation and reaching behind my back. Dressing became challenging, and everyday tasks like brushing teeth and eating were painful and slow. Driving, especially checking over my right shoulder and putting on the seatbelt, was painful. I hesitated to go out in icy conditions due to fear of falling and instinctively using my right arm. Computer work became uncomfortable due to mouse use. I had experienced frozen shoulder before in the other arm, but this time was more painful. I opted for physiotherapy, receiving acupuncture, soft tissue, and joint mobilization techniques, along with exercises. The pain has lessened, and although movement is still limited, I am optimistic about recovery.”
F, a 50-year-old woman with shoulder pain
Future Developments and Surgical Interventions
Surgery is indicated for emergencies like unreduced dislocation, infection, and traumatic acute rotator cuff tears. Its role in frozen shoulder is less defined, with some surgeons advocating manipulation under anesthesia and arthroscopic release. Recent studies suggest comparable outcomes for supervised physiotherapy and arthroscopic decompression for rotator cuff disease. For significant persistent disability due to impingement and rotator cuff tears unresponsive to conservative treatment, surgery may effectively relieve pain and restore function. However, studies often involve small participant numbers and limited long-term follow-up. The management of mildly symptomatic small rotator cuff tears remains controversial. For resistant acromioclavicular joint pain, arthroscopic distal clavicle excision is an effective low-risk procedure. Surgery remains the primary treatment for recurrent shoulder instability. Osteoarthritis and rheumatoid arthritis management has improved, with joint replacement providing pain relief for end-stage disease.
Conclusions for Primary Care Diagnosis of Shoulder Problems
Shoulder pain is a common and significant musculoskeletal issue in primary care. Management should be multidisciplinary, encompassing self-help advice, analgesics, relative rest, and access to physiotherapy. Steroid injections offer limited short-term pain relief.
Poorer prognosis is associated with older age, female gender, severe/recurrent symptoms at presentation, and neck pain. Mild trauma or overuse before pain onset, early presentation, and acute onset are linked to a more favorable prognosis. Early orthopedic intervention does not improve prognosis for most rotator cuff or glenohumeral disorders. Surgery should be considered when conservative approaches fail.
Supplementary Material
[extra: Extra references]
bmj_331_7525_1124__index.html (2.3KB, html)
Extra references w1-12 are available on bmj.com
Contributors: CM, AA, and EH conceived the article idea. CM reviewed the literature. All authors contributed to writing. CM is the guarantor.
Competing interests: None declared.
References
Associated Data
Supplementary Materials
[extra: Extra references]
bmj_331_7525_1124__index.html (2.3KB, html)