Pneumonia, an infection that inflames the air sacs in one or both lungs, can range in severity from mild to life-threatening. Accurate and timely Diagnosis Pneumonia is crucial for effective treatment and management of the condition. If you suspect you or a loved one may have pneumonia, understanding the diagnostic process can help alleviate concerns and ensure prompt medical attention. This article will guide you through the common methods and procedures used in diagnosis pneumonia.
Initial Steps in Pneumonia Diagnosis
The journey to diagnosis pneumonia often begins with a visit to your doctor. They will initiate the diagnostic process through a combination of methods focusing on your symptoms and lung condition.
Medical History and Physical Examination
Your doctor will start by gathering essential information about your health. This includes:
- Medical History: They will inquire about your past medical conditions, especially any history of lung diseases, recent illnesses, and exposure to potential irritants or infections.
- Symptom Review: You’ll be asked about your current symptoms, such as cough (productive or dry), fever, chills, chest pain, shortness of breath, and fatigue. Detailing the onset, duration, and severity of these symptoms is vital.
- Physical Examination: A key part of the initial diagnosis pneumonia is a physical exam. Your doctor will use a stethoscope to listen to your lungs. During auscultation, they will listen for:
- Crackling sounds (rales): These sounds, similar to rubbing strands of hair together, can indicate fluid in the small air sacs.
- Bubbling sounds (rhonchi): These lower-pitched, snoring-like sounds may suggest larger airways are obstructed with mucus.
- Wheezing: A high-pitched whistling sound, potentially indicating narrowed airways, although less specific to pneumonia.
- Decreased breath sounds: Reduced or absent sounds in certain lung areas might indicate consolidation, where air spaces are filled with fluid or inflammatory cells.
If the physical exam and medical history suggest pneumonia, further diagnostic tests are usually ordered to confirm the diagnosis pneumonia and identify the type and extent of the infection.
Diagnostic Tests for Pneumonia
To definitively diagnosis pneumonia and determine its characteristics, doctors utilize several diagnostic tests. These tests help visualize the lungs, identify the presence of infection, and sometimes pinpoint the causative organism.
Chest X-ray: Visualizing Lung Inflammation
A chest X-ray is a standard and crucial imaging test for diagnosis pneumonia. It uses a small amount of radiation to create images of your lungs. In the context of diagnosis pneumonia, a chest X-ray can:
- Confirm Pneumonia: Pneumonia typically appears on an X-ray as areas of increased density or opacity in the lungs. These opacities represent inflammation and fluid buildup in the air sacs (alveoli).
alt=”Chest X-ray image illustrating lung inflammation indicative of pneumonia, a key diagnostic tool for respiratory infections.”
- Determine Extent and Location: The X-ray helps assess how much of the lung is affected and whether the pneumonia is localized to one area or widespread.
- Rule Out Other Conditions: While not specific to pneumonia, a chest X-ray can help exclude other lung conditions that may mimic pneumonia symptoms.
- Monitor Treatment Progress: Follow-up X-rays may be used to track the resolution of pneumonia and ensure the infection is clearing as expected.
It’s important to note that while a chest X-ray is essential for diagnosis pneumonia, it usually cannot identify the specific germ causing the infection (bacterial, viral, fungal).
Blood Tests: Identifying Infection and Organism Type
Blood tests are another important component in the diagnosis pneumonia process. They provide valuable information about the presence and nature of the infection:
- Complete Blood Count (CBC): This test measures different types of blood cells. Elevated white blood cell counts, particularly neutrophils, often indicate a bacterial infection.
- Blood Culture: In more severe cases or when specific organisms are suspected, blood cultures may be ordered. This test attempts to grow bacteria or other pathogens from a blood sample, potentially identifying the causative agent of pneumonia. However, blood cultures are not always positive, even in bacterial pneumonia.
- Inflammatory Markers: Tests like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can measure general inflammation levels in the body, supporting the presence of an infection like pneumonia.
- Arterial Blood Gas (ABG): This test measures the oxygen and carbon dioxide levels in your blood, as well as blood pH. It helps assess the severity of pneumonia and how well your lungs are functioning in oxygenating your blood.
Pulse Oximetry: Measuring Blood Oxygen Levels
Pulse oximetry is a non-invasive and quick test used to measure the oxygen saturation level in your blood. A small sensor is placed on your fingertip or earlobe, and it estimates the percentage of hemoglobin in your red blood cells that is carrying oxygen. In diagnosis pneumonia, pulse oximetry is valuable because:
- Detects Hypoxemia: Pneumonia can impair the lungs’ ability to transfer oxygen into the bloodstream, leading to low blood oxygen levels (hypoxemia). Pulse oximetry helps identify this.
- Assesses Severity: Lower oxygen saturation levels can indicate more severe pneumonia and the need for supplemental oxygen or hospitalization.
- Monitors Oxygenation: Pulse oximetry can be used to continuously monitor oxygen levels during treatment and recovery.
Sputum Test: Pinpointing the Cause of Infection
A sputum test involves analyzing a sample of mucus (sputum) coughed up from your lungs. This test can be particularly helpful in diagnosis pneumonia as it aims to identify the specific organism causing the infection:
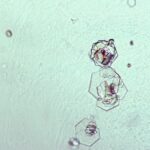
- Gram Stain and Culture: The sputum sample is examined under a microscope after Gram staining to identify bacteria and their characteristics. It’s also cultured in a lab to grow bacteria or fungi, allowing for more precise identification and antibiotic susceptibility testing.
- Viral Testing: In certain cases, sputum can be tested for specific viruses, especially if viral pneumonia is suspected (e.g., influenza, respiratory syncytial virus (RSV)).
- Pneumocystis jirovecii (PJP) testing: For individuals with weakened immune systems, sputum may be tested for this specific fungal pneumonia.
Obtaining a good quality sputum sample can be challenging, as it needs to be coughed up from the lungs and not just saliva.
CT Scan: Detailed Lung Imaging
In some situations, particularly if pneumonia symptoms are severe, not improving as expected, or if there are complications, a chest CT (computed tomography) scan may be recommended. A CT scan provides more detailed cross-sectional images of the lungs compared to a standard X-ray. In diagnosis pneumonia, a CT scan can:
- Provide More Detail: It can reveal subtle lung abnormalities that may not be visible on a chest X-ray.
- Assess Complications: CT scans are useful for detecting complications of pneumonia, such as lung abscesses, pleural effusions (fluid around the lungs), or empyema (pus in the pleural space).
- Investigate Underlying Conditions: If pneumonia is recurrent or atypical, a CT scan can help identify underlying lung diseases or structural abnormalities that might be predisposing to infections.
Pleural Fluid Culture: Diagnosing Pleural Effusion Infections
If pneumonia is associated with a pleural effusion (fluid buildup between the lung and chest wall), a pleural fluid culture may be performed as part of the diagnosis pneumonia process, especially if infection of the pleural space (empyema) is suspected. This procedure, called thoracentesis, involves:
- Fluid Aspiration: A needle is inserted through the chest wall to withdraw a sample of pleural fluid.
- Fluid Analysis: The fluid is sent to the lab for analysis, including cell counts, protein and glucose levels, Gram stain, and culture to identify bacteria or other organisms causing infection in the pleural space.
When Additional Tests Are Considered
While chest X-rays and basic tests are often sufficient for diagnosis pneumonia, additional tests might be considered in specific situations:
- Older Adults (Age 65+): Due to potentially weaker immune systems and higher risk of complications, older adults may undergo more comprehensive testing.
- Hospitalized Patients: Individuals admitted to the hospital for pneumonia often require more extensive testing to manage their condition effectively.
- Severe Symptoms or Underlying Health Conditions: Patients with severe pneumonia, weakened immune systems, or other chronic health issues may need further investigation to guide treatment and monitor their progress.
- Pneumonia Not Clearing as Expected: If pneumonia symptoms and X-ray findings are not improving with initial treatment, further tests like CT scans or bronchoscopy (visualizing airways with a camera) may be necessary to rule out resistant organisms, complications, or alternative diagnoses.
Conclusion
Accurate and timely diagnosis pneumonia is the first critical step in managing this common respiratory infection. The diagnostic process typically involves a combination of medical history, physical examination, and various tests, including chest X-rays, blood tests, sputum analysis, and in some cases, more advanced imaging like CT scans. Understanding the methods used in diagnosis pneumonia can empower you to engage effectively with your healthcare provider and ensure you receive the most appropriate care. If you experience symptoms suggestive of pneumonia, seek medical attention promptly for proper evaluation and diagnosis.