Cough stands as the most prevalent complaint prompting patients to seek consultation with their primary care physicians, accounting for approximately 8% of all visits. The sheer volume of new research necessitates a thoroughly updated version of the cough guideline issued by the German College of General Practitioners and Family Physicians (DEGAM), the last iteration of which was released in 2008. This updated guideline aims to provide a robust framework for primary care physicians in diagnosing and managing acute cough, emphasizing evidence-based practices and reducing the overuse of antibiotics.
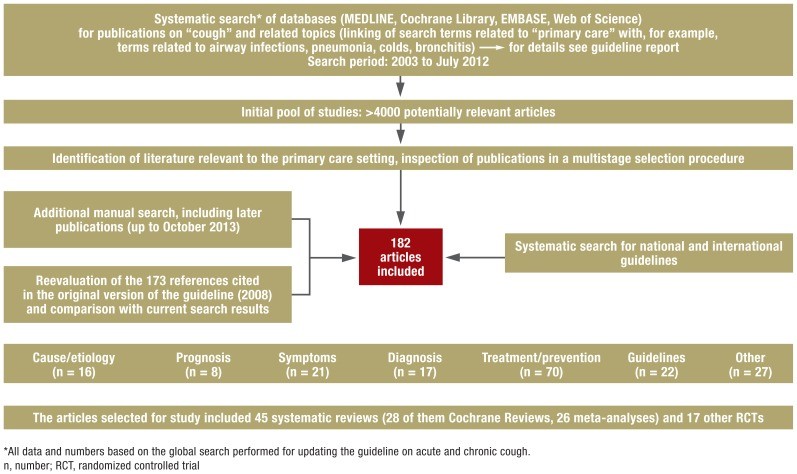
The cornerstone of this updated S3 guideline from DEGAM is a systematic review of pertinent literature published between 2003 and July 2012. This review encompassed a comprehensive search across MEDLINE, Cochrane Library, EMBASE, and Web of Science databases. The guideline development adhered to rigorous standards set by the Association of Scientific Medical Societies in Germany (AWMF), incorporating evidence level assessments and consensus procedures with the active participation of seven medical societies. This meticulous process ensures the guideline reflects the best available evidence and expert consensus, enhancing its reliability and applicability in clinical practice.
The updated guideline integrates findings from 182 publications, including 45 systematic reviews (26 with meta-analyses) and 17 randomized controlled trials (RCTs). Through a nominal group process, 11 recommendations for managing acute cough were unanimously approved. Central to the diagnostic approach are the patient’s history and physical examination. Significantly, the guideline recommends against routine laboratory tests, sputum evaluations, or chest X-rays, and the use of antibiotics when acute, uncomplicated bronchitis is clinically diagnosed. The evidence supporting the effectiveness of antitussive or expectorant medications for acute cough is deemed insufficient. While phytotherapeutic agents show promise, the evidence base is varied. For community-acquired pneumonia, empirical antibiotic treatment for 5 to 7 days is advised, with drug choice guided by specific risk factors. The guideline also advises against routine laboratory tests and neuraminidase inhibitors in typical influenza management. A key objective of these updated recommendations is to significantly decrease antibiotic use for colds and acute bronchitis, conditions for which antibiotics are not indicated and contribute to growing antimicrobial resistance. The guideline underscores the need for more robust clinical trials to strengthen the evidence base for cough treatments, which currently remains fragmented.
Cough is indeed the most common reason for patients to visit primary care physicians, constituting approximately 8% of all consultations. The widespread prevalence of cough is further highlighted by annual estimates ranging from 10% to 33% in the general population. Acute cough is overwhelmingly caused by upper respiratory tract infections and acute bronchitis, collectively accounting for over 60% of diagnosed cases. The economic burden is substantial, with respiratory infections contributing to about 20% of work absences and around 10% of sick leave days.
This article provides a concise overview of the essential content and recommendations from the recent update to the guideline on acute cough, defined as cough lasting less than 8 weeks. The primary goal of this guideline is to elucidate the differential diagnoses for the symptom of “cough” in adult patients. It aims to equip physicians with the necessary guidance to effectively identify the underlying cause of acute cough and implement evidence-based treatments, with a strong focus on practical relevance within primary care settings. Reflecting the realities of primary care, DEGAM guidelines are intentionally symptom-focused rather than solely disease-oriented. Consequently, this guideline approaches cough as the primary concern, discussing underlying diseases only as they relate to the symptom itself, not in exhaustive detail.
Methodology for Guideline Revision
Revision Process
DEGAM established a comprehensive framework for guideline development, dissemination, implementation, and evaluation fifteen years prior to this update. This framework includes the creation of practice-oriented concise versions and patient information sheets to complement the full guidelines. The original cough guideline was published in 2008. In 2013, a comprehensive update was undertaken, adhering to the rigorous standards for S3 guidelines under the auspices of the AWMF. This revision was driven by a significant influx of new evidence concerning both the diagnosis and treatment of acute cough, necessitating a thorough reassessment and update of the existing recommendations.
Guideline Development Group
The revision process engaged a multidisciplinary group, with representatives from seven prominent German medical societies (Box 1). To ensure transparency and minimize bias, all members of the guideline group were required to disclose any potential conflicts of interest, a process meticulously documented in the full guideline report. This collaborative and transparent approach strengthens the credibility and broad applicability of the revised guideline.
Box 1. Organizations and Persons Involved in the Revision of the S3 Guideline.
- Institute for General Practice, Charité Universitätsmedizin, Berlin
- Dr. Sabine Beck*1
- Prof. Vittoria Braun
- Dr. Lorena Dini MScIH*1
- Dr. Christoph Heintze MPH*1
- Dr. Felix Holzinger MPH*1
- Christiane Stöter MPH
- Dr. Susanne Pruskil MScPH
- Mehtap Hanenberg
- Max Hartog
- Representatives of Medical Societies
- Prof. Stefan Andreas, German Respiratory Society (DGP), German Society for Internal Medicine (DGIM)*1
- Patrick Heldmann MSc, Federal Association of Self-employed Physiotherapists (IFK)*1
- Dr. Susanne Herold PhD, German Society for Infectious Diseases (DGI)*1
- Dr. Peter Kardos, German Respiratory League
- Dorothea Pfeiffer-Kascha, German Association for Physiotherapy (ZVK)*1
- Dr. Guido Schmiemann MPH, German College of General Practitioners and Family Physicians (DEGAM)*1
- Prof. Heinrich Worth, German Respiratory Society (DGP), German Respiratory League*1
- Guideline Patrons (DEGAM)
- Prof. Annette Becker
- Dr. Günther Egidi
- Dr. Detmar Jobst
- Dr. Guido Schmiemann MPH
- Dr. Hannelore Wächtler
- The authors also thank
- Prof. Jost Langhorst
- Dr. Petra Klose
- Dr. Cathleen Muche-Borowski MPH (DEGAM, AWMF)
- Dr. Monika Nothacker MPH (AWMF)*2
- Dr. Anja Wollny MSc (DEGAM)
*1 Participants of consensus conference
*2 Moderator of consensus conference
Literature Review Strategy
Building upon the search strategy used for the original guideline, the literature review was extended to include publications up to July 2012. Key databases including MEDLINE, Cochrane Library, EMBASE, and Web of Science were systematically searched. This was complemented by a search for relevant national and international guidelines and a manual search to capture sources published after the systematic database search cutoff date.
The identified sources underwent a rigorous screening process, examining titles, abstracts, and full-text versions to determine relevance. The inclusion criteria prioritized randomized controlled trials (RCTs), meta-analyses, and reviews, particularly systematic reviews, alongside high-quality clinical guidelines. In total, 182 publications were deemed pertinent and incorporated into the guideline update (Box 2, Figure). This comprehensive literature review ensures the guideline is grounded in the most current and robust evidence available.
Box 2. Examples of Search Terms.
- Search terms related to acute cough (selection)
- (acute) cough*
- common cold*
- respiratory tract infections*
- bronchitis
- sputum
- pneumonia
- Search terms related to primary care (selection)
- general practice
- family practice*
- family medicine
- primary (health) care*
*Additional search in PubMed via corresponding MeSH terms; MeSH, medical subject headings
Figure.
Overview of the literature search
Consensus and Recommendation Strength
A consensus conference, moderated by AWMF, was held on June 17, 2013, to review the draft guideline. Recommendations derived from the evidence analysis were presented and, through a nominal group process, unanimously adopted. One exception occurred where a participant abstained from voting on a single recommendation due to a self-identified conflict of interest. This strong consensus among experts from various medical societies reinforces the guideline’s validity and clinical applicability.
The strength of each recommendation is determined by the quality of the underlying evidence, considering study type, design adequacy, internal validity, and potential for bias. The GRADE (Grading of Recommendations Assessment, Development and Evaluation) Working Group criteria were also applied, encompassing factors like uncertainty in benefit magnitude, patient preferences, and cost-effectiveness. The guideline employs a three-tiered recommendation strength system: A, B, and C (Table 1), providing clinicians with a clear understanding of the evidence base and the strength of each recommendation.
Table 1. Recommendations and Evidence.
| Recommendation strength A | Evidence level |
|---|---|
| Clinical diagnosis of acute uncomplicated bronchitis renders laboratory testing, sputum evaluation, and chest radiographs unnecessary. | TIa, PII ↔ |
| Uncomplicated acute bronchitis should not be treated with antibiotics. | TIa ↔ |
| The patient should be informed about the spontaneous course of acute (cold-related) cough. | TIb, SIII ↔ |
| Recommendation strength B | Evidence level |
| Technical investigations should be dispensed with in acute cough with no danger signs. | SIV ↑ |
| Acute cough in the context of infection should not be treated with expectorants (secretolytics, mucolytics). | TIa ↓ |
| Acute cough in the context of infection should only exceptionally be treated with antitussives. | TIIa ↔ |
| Sputum evaluation should not be routine in community-acquired pneumonia. | DII, CII ↔ |
| In the absence of risk factors, community-acquired pneumonia should be treated with an empirical oral antibiotic (an aminopenicillin, or alternatively a tetracycline or a macrolide) for 5 to 7 days. | TIa ↓ |
| In the presence of risk factors, community-acquired pneumonia should be treated with an empirical oral antibiotic (an aminopenicillin with a betalactamase inhibitor, or alternatively with a cephalosporin) for 5 to 7 days. | TIa ↓ |
| Laboratory testing (serology, direct demonstration of virus) should not be routine in suspicion of an influenza ‧infection. | TIa, DI ↓ |
| Neuraminidase inhibitors should be used only exceptionally for treatment of seasonal influenza. | TIa ↓ |
- Evidence level depending on the respective research question: T, treatment-related; D, diagnosis-related; S, symptom-related; C, cause-related; P, prognosis-related
- Level I–IV: strength of underlying evidence, e.g., for treatment-related questions: Ia, systematic reviews/meta-analyses; Ib, randomized controlled trials (RCT); IIa, controlled cohort studies; IIb, case–control studies; III, noncontrolled studies; IV, expert opinion/Good Clinical Practice, according to DEGAM guideline development concept
- Result of consensus process/application of GRADE criteria: ↔ Recommendation strength corresponds to evidence level, ↑ Upgrading, ↓ Downgrading GRADE, Grading of Recommendations Assessment, Development and Evaluation
Guideline Contents and Recommendations: Differential Diagnoses of Acute Cough
History and Clinical Examination in Acute Cough
In the majority of primary care patients presenting with acute cough, a diagnosis can be effectively established through a thorough medical history and a symptom-focused physical examination. In these typical cases, extensive technical diagnostic investigations offer limited additional value. The guideline emphasizes the importance of these fundamental clinical skills in efficiently managing acute cough.
Key elements of history taking and physical examination are summarized in Table 2, providing a structured approach for clinicians. This table serves as a quick reference for essential components of the initial patient assessment.
Table 2. History, Physical Examination, and Danger Signs in Acute Cough.
| History and accompanying symptoms |
|---|
| – Nature and duration of cough – Fever – Expectoration (amount, consistency, hemoptysis) – Breathing problems (dyspnea, stridor) – Smoking history – Previous respiratory tract infections, chronic bronchitis/sinusitis – Allergies, asthma, COPD |
| Physical examination |
| – Inspection of skin (pallor, cyanosis, sweating) – Inspection of mouth and throat, obstructed nasal breathing, percussion pain in nasal sinuses – Examination of thorax (inspection, percussion and auscultation of lungs, breathing rate, auscultation of heart) – Palpation of abdomen depending on history and clinical findings – Inspection and palpation of legs (edema, signs of thrombosis) |
| Dangers |
| Pulmonary embolism |
| Pulmonary edema |
| Status asthmaticus |
| Pneumothorax |
| Foreign body aspiration |
COPD, chronic obstructive pulmonary disease
Identifying Danger Signs in Acute Cough
A critical objective of history taking and physical examination is to differentiate between benign infections and more serious underlying conditions, facilitating early detection of patients at potential risk. In some instances, a life-threatening illness may be present or imminent. Recognizing these “red flags” is paramount for timely intervention.
Major warning signs indicating potential danger are listed in Table 2. These include dyspnea, tachypnea, thoracic pain, hemoptysis, significant deterioration in general condition, and changes in vital signs such as high fever, tachycardia, and arterial hypotension. The presence of complicating underlying diseases like malignancy or immune deficiency further elevates the concern.
In urgent situations characterized by these danger signs, immediate action is crucial. Typically, this necessitates prompt transfer to a hospital setting, ideally accompanied by a physician or emergency medical personnel. Rapid response in these cases can be life-saving.
Differential Diagnosis: Frequent Causes of Acute Cough
The principal differential diagnoses for acute cough are outlined in Table 3. The most common causes encountered in primary care are discussed in detail below, providing a framework for diagnostic consideration.
Table 3. Frequent Causes of Acute Cough.
| Manifestation | Clinical presentation |
|---|---|
| Acute cough | – Colds (common cold, URTI) and acute bronchitis – Pneumonia – Influenza – Pertussis – Inhaled noxae – Acute left heart failure with congestion |
| Acute and chronic cough | – COPD (incl. acute exacerbation) – Gastroesophageal reflux – Upper airway cough syndrome (previously: postnasal drip syndrome) – Adverse drug effects |
COPD, chronic obstructive pulmonary disease; URTI, upper respiratory tract infection
Colds and Acute Bronchitis as a Cause of Acute Cough
Clinical Presentation: Upper respiratory tract infections (URTIs), commonly known as the “common cold,” are the most frequent cause of acute cough. Typical accompanying symptoms include sore throat, nasal congestion and discharge, headache, muscle aches, fatigue, and sometimes fever. Viral pathogens are predominantly responsible, including adenoviruses, rhinoviruses, influenza and parainfluenza viruses, coronaviruses, respiratory syncytial virus (RSV), and coxsackieviruses. The cough associated with acute bronchitis typically starts as dry and progresses to productive. It’s important to note that there isn’t a sharp distinction between a common cold and acute bronchitis, as both can involve varying degrees of lower respiratory tract involvement. While colds are generally self-limiting, resolving within two weeks in about two-thirds of cases, bronchitis-related cough can persist for several weeks. Acute sinusitis, often occurring in conjunction with a cold, can also trigger cough reflexes.
Diagnosis: When the patient’s history and clinical findings are consistent with a cold or bronchitis, and in the absence of danger signs (Table 2), routine chest radiographs or clinical chemistry tests are not necessary. Distinguishing between viral and bacterial bronchitis through leukocyte or C-reactive protein (CRP) determination is not clinically relevant, as treatment decisions remain unchanged. Sputum color is not a reliable indicator of bacterial bronchitis or in differentiating between pneumonia and bronchitis. Sputum examination in otherwise healthy bronchitis patients is generally not indicated, as antibiotics are not recommended. Spirometry may be considered if there are signs of bronchial obstruction, as acute bronchitis can induce temporary airway constriction. For patients whose cough persists beyond 8 weeks, further detailed investigation is warranted to explore other potential underlying causes.
Treatment: Evidence supporting non-pharmacological treatments for colds and bronchitis is limited. Maintaining adequate hydration is physiologically sensible, although excessive fluid intake carries a potential risk of hyponatremia. Smoking cessation is strongly advised, as both active and passive smoking prolong recovery from colds. The efficacy of nasal saline rinses/sprays and steam inhalation is inconsistent across RCTs. To minimize transmission of respiratory viruses, coughing into the elbow rather than the hand is recommended. Frequent handwashing, particularly during cold and flu seasons, is a sensible preventative measure.
Cough associated with colds, acute bronchitis, or sinusitis typically resolves spontaneously without specific medicinal intervention. Patients should be reassured that these illnesses are usually self-limiting and benign, and that routine medication is often unnecessary. However, symptomatic relief can be offered if desired by the patient.
Analgesics like acetaminophen and ibuprofen are recommended for managing headache and muscle aches. RCTs have not demonstrated a significant advantage of antitussives (e.g., codeine) over placebo in reducing cough frequency in common colds, although they may improve nighttime sleep. Expectorants are frequently prescribed for productive cough, despite a lack of robust evidence supporting their efficacy in acute cough. High-quality observational studies or RCTs for this indication are lacking, and the applicability of findings from chronic bronchitis studies to acute bronchitis or colds remains uncertain. Decongestant nasal drops or sprays can provide short-term symptom relief, but prolonged use beyond 7 days is not recommended due to diminishing returns and the risk of atrophic rhinitis.
The evidence base for phytotherapeutics is complex due to methodological variations in studies and inconsistent compositions of herbal preparations. Some RCTs suggest potential benefits of myrtol standardized for symptom severity and recovery time. One study reported a 62.1% reduction in daytime cough frequency by day 7 with myrtol, compared to 49.8% with placebo. Adverse effects are mainly mild gastrointestinal symptoms. Another RCT indicated improved symptom relief with a thyme and ivy leaf preparation (77.6% cough reduction on day 9 vs. 55.9% for placebo), and similar effects were observed for thyme and primrose root combinations, with no reports of serious side effects for these preparations. A limited number of studies suggest a slight, dose-dependent acceleration of bronchitis recovery with Pelargonium sidoides. However, placebo-controlled studies showed a higher rate of gastrointestinal side effects compared to placebo, and concerns about potential hepatotoxicity limit firm conclusions regarding its benefit-harm ratio. A Cochrane Review suggested possible therapeutic efficacy for early administration of Echinacea aerial parts, with a low risk of allergic reactions with oral intake, although contraindications (e.g., tuberculosis, AIDS, autoimmune diseases) must be considered. Echinacea root components have not shown preventive or therapeutic effects.
Regular vitamin C intake does not reduce cold frequency in the general population, except for individuals under extreme physical stress (e.g., marathon runners). Vitamin C has not demonstrated therapeutic benefit once a cold has developed. A meta-analysis indicated that regular zinc intake might reduce cold symptom duration, but adverse effects like nausea and unpleasant taste limit general recommendations due to unclear optimal dosage and duration.
Antibiotic treatment is not necessary for uncomplicated acute bronchitis. Antibiotics offer minimal symptom relief and shorten recovery time by less than a day, while posing risks of adverse effects and antibiotic resistance. Patient education can effectively reduce antibiotic prescription rates. Antibiotic use might be considered in select patients with serious chronic diseases or immune deficiencies where ruling out pneumonia is challenging, but even in these cases, routine antibiotic use is discouraged as bronchitis is typically viral in origin.
Pneumonia as a Cause of Acute Cough
Clinical Presentation: Cough accompanied by tachypnea, tachycardia, high fever, characteristic auscultation findings, and pleuritic chest pain are suggestive of pneumonia. However, pneumonia presentation can be atypical, particularly in older or immunosuppressed patients, or those with pre-existing chronic lung disease, potentially lacking typical fever or respiratory signs.
Diagnosis: Chest radiography in two projections is advisable, especially when diagnostic uncertainty exists, in cases of severe illness, or in patients with comorbidities. Neither leukocyte count nor CRP levels definitively confirm pneumonia diagnosis. CRP measurement may be useful for monitoring disease progression but is not routinely recommended for outpatients. Procalcitonin measurement has shown potential to reduce or avoid antibiotic use, but routine procalcitonin testing is not currently recommended due to cost considerations. Sputum tests in outpatients with community-acquired pneumonia have low sensitivity and specificity. Given that targeted antibiotic therapy is not superior to empirical treatment, sputum testing is generally not advised in community-acquired pneumonia management in the outpatient setting.
Treatment: Clinically stable patients with community-acquired pneumonia can be managed by primary care physicians. Empirical antibiotic selection should consider the presence of risk factors, necessitating coverage for a broader range of potential pathogens. Clinical reassessment of treatment effectiveness is needed within 48 to 72 hours. Extending antibiotic treatment beyond 7 days does not improve success rates. Fluoroquinolones should be reserved for exceptional outpatient scenarios due to potential severe adverse effects and the promotion of antibiotic resistance (Table 4).
Table 4. Antibiotic Treatment in Community-Acquired Pneumonia*.
| Patients without risk factors |
|—|—|—|
| Substances | Dosage | Duration |
| Penicillin (oral): Amoxicillin | ≥ 70 kg: 3 x 1000 mg | 5–7 days |
| Tetracycline (oral): Doxycycline | ≥ 70 kg: 200 mg |
| Macrolide (oral): Roxithromycin, Clarithromycin | 1 x 300 mg, 2 × 500 mg | |
| Azithromycin | 1 × 500 mg | 3 days |
| Patients with risk factors (antibiotic treatment in previous 3 months, severe comorbidity, care home resident) |
| Substances | Dosage | Duration |
| Aminopenicillin + betalactamase inhibitor: e.g., sultamicillin (oral) | 2 x 750 mg | 5–7 days |
| Alternative: cephalosporins: e.g., cefuroxime axetil (oral) | 2 x 500 mg | |
*Modified from
Influenza as a Cause of Acute Cough
Clinical Presentation: Influenza typically presents with an abrupt onset of symptoms, including high fever, marked malaise, and muscle pain. This rapid and systemic presentation helps differentiate it from milder upper respiratory infections.
Diagnosis: Clinical examination is usually sufficient for influenza diagnosis in typical cases. Antibody testing or direct viral detection via swabs should be reserved for cases with diagnostic uncertainty or when treatment decisions depend on confirming influenza (see below).
Treatment: Neuraminidase inhibitors can be considered for treatment if initiated within the first 48 hours of symptom onset. However, the evidence for their efficacy is not conclusive, and due to a limited cost-benefit ratio, their use is generally recommended only for select individual patients, such as those with severe immunosuppression. Given the potentially severe course of influenza, hospitalization should be considered, especially for elderly or multimorbid patients and those with complications.
Vaccination against influenza is recommended for individuals over 60 years of age by the German Standing Committee on Vaccination Recommendations (STIKO). However, a recent meta-analysis with stringent inclusion criteria suggests that vaccine efficacy may be suboptimal in some cases, and RCT data for those over 65 are lacking, highlighting ongoing questions about influenza vaccination effectiveness in older adults.
Pertussis (Whooping Cough) as a Cause of Acute Cough
Clinical Presentation: Pertussis, or whooping cough, is increasingly affecting adults. Adult patients often exhibit an atypical, milder disease course characterized by a nonspecific dry cough. Vaccine-induced immunity wanes after several years. In the initial catarrhal stage, differentiating pertussis from a common cold is challenging. The characteristic paroxysmal whooping cough typically develops after 1 to 2 weeks (second peak) and can persist for 4 weeks or longer.
Diagnosis: Pathogen identification via culture of nasopharyngeal secretions is reliable only within the first 2 weeks of illness. Polymerase chain reaction (PCR) is more sensitive and can detect infection up to 4 weeks after onset but is more expensive. In later stages of the disease, serology is the primary diagnostic method, with results interpreted in the context of clinical presentation and in consultation with the laboratory.
Treatment: In the catarrhal stage, treatment with azithromycin or clarithromycin can accelerate recovery. Antibiotic treatment remains beneficial even later in the disease course as it shortens the period of contagiousness. Antibiotic prophylaxis is recommended for household contacts, particularly for those sharing a household with infants under 6 months. Vaccination according to STIKO recommendations is strongly encouraged. The pertussis vaccine is only available as a combination vaccine.
Asthma and Infection-Exacerbated COPD as Causes of Acute Cough
Chronic respiratory diseases such as asthma and COPD can present with acute exacerbations triggered by infections, leading to acute cough. In some cases, cough may be the initial presenting symptom of these underlying conditions. For detailed guidance on the diagnosis and management of asthma and chronic obstructive pulmonary disease (COPD), clinicians should consult the relevant National Disease Management Guidelines, which provide comprehensive recommendations for these chronic conditions.
Implementation and Outlook for Acute Cough Management
For uncomplicated colds and acute bronchitis, the central recommendation of this guideline is to adopt a restrained diagnostic and therapeutic approach. It is crucial to educate patients with these self-limiting, benign conditions that extensive technical investigations and medicinal treatments are generally unnecessary. This guideline, along with accompanying patient information sheets, provides evidence-based arguments to support primary care physicians in addressing patient anxieties and questions regarding treatment options. Even in cases of bronchitis with yellow-green sputum or mild fever, patients can be reassured that the infection is most likely viral, making antibiotic treatment inappropriate. In practice, antibiotics are frequently prescribed for URTIs or bronchitis, contributing to antibiotic resistance. If patients strongly desire treatment, symptomatic relief with agents like nonsteroidal anti-inflammatory drugs or decongestant nasal drops can be recommended. Phytotherapeutic substances represent another option, with some evidence suggesting modest symptom relief or shortening of illness duration, although patients must bear the costs and potential, albeit usually minor, side effects. The decision to use such preparations should be made through shared decision-making between physician and patient. Furthermore, given the widespread use of cough treatments lacking robust evidence of benefit, methodologically sound, publicly funded research is essential to systematically evaluate these substance groups for the indication of “acute cough.”
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.