Introduction
Deep vein thrombosis (DVT) is a serious medical condition characterized by the formation of a blood clot in a deep vein, most commonly in the legs. While seemingly unrelated to automotive repair, understanding DVT is crucial for professionals in physically demanding roles, as prolonged immobility and certain risk factors can increase susceptibility. Recognizing the signs and symptoms and being aware of the Differential Diagnosis For Deep Vein Thrombosis can be life-saving, both personally and for those around you. DVT is a significant health concern, ranking as the third leading cause of cardiovascular death after heart attacks and strokes. Beyond the immediate threat of pulmonary embolism, recurrent thrombosis and post-thrombotic syndrome contribute significantly to long-term morbidity. Early and accurate diagnosis is paramount to mitigate these risks.
Etiology and Risk Factors
Several factors contribute to the development of DVT. Understanding these is essential for appreciating the diverse patient populations affected and for considering differential diagnoses.
Increased Risk of Coagulation
Constitutional Factors: Conditions that inherently increase the risk of blood clot formation are significant contributors. Obesity, a growing concern globally, is linked to hypercoagulability through elevated fibrinogen levels and slower venous blood flow, particularly in the lower limbs. Pregnancy and advanced age (over 60) are also established risk factors. Major surgery, critical care admissions, dehydration, and cancer further elevate the risk profile.
Transient Risk Factors: These are short-term conditions that increase DVT risk. They include surgery requiring general anesthesia, hospitalization (especially prolonged stays), cesarean sections, hormone replacement therapy, pregnancy and the postpartum period, and lower extremity injuries leading to immobilization for over 72 hours. General anesthesia lasting more than 30 minutes and hospitalization exceeding 72 hours are specifically recognized as transient risk factors.
Persistent Risk Factors: Ongoing medical conditions can create a sustained elevated risk for DVT. Active cancers and conditions like systemic lupus erythematosus and inflammatory bowel disease fall into this category, requiring careful consideration in differential diagnosis.
Unprovoked VTE: When DVT occurs without identifiable transient or persistent risk factors, it is classified as unprovoked venous thromboembolism (VTE). Emerging research suggests a link between blood lipid profiles and DVT risk. Higher triglyceride levels may increase the risk of lower extremity DVT (LEDVT), while higher total cholesterol, HDL-C, and apolipoprotein A1 levels may be protective.
Epidemiology
DVT and pulmonary embolism are prevalent yet often underdiagnosed conditions. Their “silent” nature leads to underestimation of true incidence and prevalence, often only discovered during autopsy or incidentally. The estimated annual incidence of DVT is approximately 80 cases per 100,000 individuals, with a lower limb DVT prevalence around 1 in 1000. In the United States alone, over 200,000 people develop venous thrombosis annually, with pulmonary embolism complicating 50,000 of these cases.
Age: DVT is uncommon in children, with risk escalating with age, predominantly affecting individuals over 40.
Gender and Ethnicity: While gender bias in DVT incidence remains debated, ethnicity plays a role. Studies in the US indicate a higher incidence and complication risk among African Americans and white individuals compared to Hispanic and Asian populations.
Associated Diseases: In hospitalized patients, malignancy, congestive heart failure, obstructive airway disease, and postoperative states are frequently associated with DVT.
Pathophysiology
Virchow’s triad elucidates the key pathophysiological mechanisms underlying DVT:
- Vessel Wall Damage: Injury to the inner lining of blood vessels can initiate clot formation.
- Blood Flow Stasis: Turbulent or slowed blood flow promotes coagulation.
- Hypercoagulability: Conditions that increase the blood’s tendency to clot are central to DVT development.
Thrombosis is a natural protective response to prevent blood loss from damaged vessels. Fibrinolysis counterbalances this process. DVT often arises from multifactorial triggers, with varying contributions from each element of Virchow’s triad. Early thrombus interaction with the endothelium triggers local cytokine production and leukocyte adhesion, furthering thrombosis. The balance between coagulation and thrombolysis dictates thrombus propagation. DVT commonly starts in low-flow areas of the lower limb, such as soleal sinuses and venous valve pockets. Emerging evidence suggests a potential link between DVT and atherosclerosis, with endothelial dysfunction in DVT potentially predisposing to atherosclerosis development.
Histopathology
Following acute thrombus formation in veins, a remodeling process ensues. Neutrophils and macrophages infiltrate the fibrin clot over weeks, leading to cytokine release and eventual replacement of fibrin by fibroblasts and collagen. This remodeling and fibrosis can impair blood flow long after the acute thrombosis resolves, contributing to long-term complications.
History and Physical Examination: Clues for Differential Diagnosis
Clinical presentation of acute lower extremity DVT is highly variable, ranging from asymptomatic to severe swelling and cyanosis. Three main patterns are recognized: distal calf vein thrombosis, femoropopliteal thrombosis, and iliofemoral thrombosis. Proximal thrombosis tends to present with more pronounced symptoms. Alarmingly, up to 50% of DVT cases may lack specific signs or symptoms, particularly postoperative patients with distal, non-occlusive thrombi.
When present, DVT signs and symptoms can include pain, edema, erythema, tenderness, fever, prominent superficial veins, pain on passive foot dorsiflexion (Homan’s sign), and cyanosis. Phlegmasia cerulea dolens, the most severe form, presents with massive swelling, cyanosis, and pain due to complete venous outflow obstruction, potentially leading to venous gangrene.
Crucially, clinical signs and symptoms alone are unreliable for DVT diagnosis. They are non-specific and overlap with other lower extremity disorders, necessitating a robust differential diagnosis approach. Conditions like lymphedema, superficial venous thrombosis, and cellulitis must be considered and excluded. Calf pain and swelling, while common, lack sufficient sensitivity and specificity for definitive diagnosis.
History Taking: Key historical features to elicit include:
- Pain (present in approximately 50% of patients, but location and character are non-specific)
- Redness (less specific and can be associated with infection or inflammation)
- Swelling (present in about 70% of patients, but can be bilateral or unilateral and have various causes)
Physical Examination Findings:
- Limb edema (unilateral edema is more suggestive of DVT, but bilateral can occur with proximal thrombus extension or systemic conditions)
- Red and warm skin with dilated veins (can also indicate cellulitis or superficial thrombophlebitis)
- Tenderness along the deep veins (non-specific, muscle strains and other soft tissue injuries can also cause tenderness)
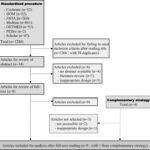
Evaluation: Ruling Out and Confirming DVT
The evaluation of suspected DVT requires a systematic approach, especially considering the wide differential diagnosis. The Clinical-Etiology-Anatomy-Pathophysiology (CEAP) classification helps categorize veins, including deep veins such as the inferior vena cava, iliac, femoral, popliteal, and crural veins.
Initial Risk Assessment: The Wells score is a critical tool for assessing the clinical probability of DVT. Scores guide subsequent investigations. A low score (0-1) indicates low probability, while a score of 2 or higher suggests high probability.
D-dimer Testing: D-dimer is a highly sensitive but non-specific test. It is most useful in ruling out DVT in low-probability patients. A negative D-dimer in a low-risk patient often excludes DVT. However, elevated D-dimer can be due to many other conditions, limiting its specificity.
Duplex Ultrasound: Proximal leg vein ultrasound is the primary imaging modality for DVT diagnosis. A positive result confirms DVT. However, negative results in high-probability patients or those with positive D-dimer may require repeat ultrasound in 6-8 days to rule out propagating calf DVT.
Point-of-Care Ultrasound (POCUS): Emergency providers can use POCUS for rapid DVT assessment, particularly when timely formal ultrasound is unavailable. Compression ultrasound at femoral and popliteal veins can quickly rule out proximal DVT. Two-region or serial compression techniques enhance sensitivity. POCUS should be integrated with clinical decision rules.
Clinical Decision Rules: Tools like the Pulmonary Embolism Rule-Out Criteria (PERC) and Wells Criteria help stratify risk and guide diagnostic pathways. PERC can identify very low-risk patients needing no further testing.
Laboratory Tests: Beyond D-dimer, baseline coagulation studies, blood counts, and renal function tests are often obtained to assess overall patient status and guide anticoagulation management.
Differential Diagnosis: Key Conditions to Differentiate from DVT
Given the non-specific nature of DVT symptoms, a comprehensive differential diagnosis is crucial. Conditions that can mimic DVT include:
-
Cellulitis: Infection of the skin and subcutaneous tissues can cause redness, warmth, swelling, and pain, similar to DVT. However, cellulitis typically presents with more prominent skin changes, fever, and often a clear entry point for infection. Ultrasound can help differentiate by showing no thrombus in cellulitis.
-
Superficial Thrombophlebitis: Inflammation and thrombosis of a superficial vein present with localized redness, tenderness, and a palpable cord. Unlike DVT, superficial thrombophlebitis is typically less severe, confined to superficial veins, and carries a lower risk of pulmonary embolism. Ultrasound can distinguish between superficial and deep vein thrombosis.
-
Lymphedema: Fluid buildup in the lymphatic system causes swelling, often in the legs. Lymphedema is typically painless, chronic, and bilateral, although unilateral lymphedema can occur. Skin changes in lymphedema are different from DVT, often with thickened, non-pitting edema. Ultrasound rules out DVT, and lymphoscintigraphy can confirm lymphedema.
-
Ruptured Baker’s Cyst: A Baker’s cyst is a fluid-filled sac behind the knee. Rupture can cause sudden calf pain and swelling, mimicking DVT. However, Baker’s cyst rupture often presents with ecchymosis (bruising) in the calf and a history of knee problems. Ultrasound can visualize the ruptured cyst and rule out DVT.
-
Muscle Strain or Tear: Musculoskeletal injuries can cause localized pain, tenderness, and sometimes swelling in the calf. History of trauma or exertion is usually present. Physical exam findings are typically localized to the muscle, and ultrasound will not show thrombus.
-
Venous Insufficiency: Chronic venous insufficiency leads to leg swelling, skin changes (venous eczema, lipodermatosclerosis), and varicose veins. Swelling is often bilateral and worse with prolonged standing. Duplex ultrasound can assess for venous reflux and rule out acute DVT.
-
Peripheral Artery Disease (PAD): While PAD primarily affects arteries, severe ischemia can cause leg pain and swelling, potentially confused with DVT. However, PAD typically presents with coolness, pallor, and diminished pulses in the affected limb. Ankle-brachial index (ABI) and arterial Doppler studies can differentiate PAD.
-
Heart Failure, Cirrhosis, Nephrotic Syndrome: These systemic conditions can cause bilateral peripheral edema, which might be mistaken for bilateral DVT. However, edema in these conditions is usually pitting, generalized, and associated with other systemic signs and symptoms of the underlying disease.
-
Venous or Lymphatic Obstruction (non-thrombotic): External compression of veins or lymphatic vessels (e.g., by tumors, masses) can cause edema mimicking DVT. Clinical context and imaging (CT, MRI) can identify non-thrombotic obstruction.
-
Arteriovenous Fistula or Congenital Vascular Abnormalities: These rare conditions can alter limb hemodynamics and cause swelling. Clinical history and specialized vascular imaging can help differentiate them.
-
Vasculitis: Inflammation of blood vessels can cause leg pain and swelling, although systemic symptoms are usually more prominent. Vasculitis is less likely to mimic acute DVT but should be considered in atypical presentations.
Treatment and Management
Once DVT is confirmed and differential diagnoses are excluded, prompt treatment is crucial to prevent pulmonary embolism, reduce morbidity, and minimize post-thrombotic syndrome risk. Anticoagulation is the cornerstone of DVT treatment.
Anticoagulation Strategies:
- Cancer-Associated Thrombosis: Low molecular weight heparin and factor Xa inhibitors (rivaroxaban, apixaban, edoxaban) are preferred. Higher anticoagulation levels may be needed in newly diagnosed cancer, extensive VTE, or treatment-related adverse effects.
- General DVT Treatment: Options include rivaroxaban, edoxaban, and vitamin-K antagonists (warfarin).
- Liver Disease: Low-molecular-weight heparin is recommended. Direct oral anticoagulants (DOACs) are contraindicated in elevated INR.
- Renal Disease: Vitamin K antagonists are preferred if creatinine clearance is below 30 ml/min. DOACs and LMWH should be avoided in end-stage renal disease.
- Coronary Artery Disease History: Options include vitamin K antagonists, rivaroxaban, apixaban, and edoxaban.
- Gastrointestinal Bleeding Risk: Vitamin K antagonists and apixaban are preferred due to lower GI bleeding risk compared to other DOACs.
- Poor Compliance Risk: Vitamin K antagonists may be preferred, but DOACs can be viable with good compliance.
- Thrombolytic Therapy: Unfractionated heparin is used if thrombolysis is indicated.
- Pregnancy: Low molecular weight heparin is the preferred anticoagulant.
Duration of Anticoagulation:
- Initial phase: Low-molecular-weight heparin or fondaparinux for 5 days, overlapping with vitamin K antagonist until INR is therapeutic (2-3) for 24 hours.
- Maintenance phase: Vitamin K antagonists for at least 3 months.
- Cancer patients: Consider low-molecular-weight heparin for 6 months or longer.
- Unprovoked DVT: Consider extended vitamin K antagonist therapy beyond 3 months.
- Rivaroxaban, an oral factor Xa inhibitor, offers convenience without routine INR monitoring.
Thrombolysis: Reserved for severe symptomatic iliofemoral DVT with low bleeding risk and good functional status. Endovascular interventions like catheter-directed thrombolysis or mechanical thrombectomy may be considered.
Adjunctive Measures:
- Compression hosiery: Graduated compression stockings for 2 years to reduce post-thrombotic syndrome.
- Inferior vena cava filters: Used when anticoagulation is contraindicated or ineffective in preventing pulmonary embolism.
Newer Drugs: Rivaroxaban, apixaban, dabigatran, edoxaban, and betrixaban are newer factor Xa inhibitors for DVT prophylaxis and treatment.
Surgical Oncology and Thromboprophylaxis
Cancer patients have a heightened VTE risk, necessitating thromboprophylaxis. Guidelines recommend anticoagulation (unfractionated heparin or low molecular weight heparin) for hospitalized cancer patients. Mechanical prophylaxis is used when anticoagulation is contraindicated (active bleeding, thrombocytopenia). Post-operative VTE prophylaxis may extend up to 4 weeks in pelvic or abdominal oncology surgery. Low molecular weight heparin remains a preferred option for cancer-associated thrombosis.
Staging and Prognosis
DVT severity is staged based on:
- Provoked vs. Unprovoked: Provoked DVT has identifiable risk factors, while unprovoked DVT is idiopathic. Unprovoked DVT carries a higher recurrence risk.
- Proximal vs. Distal: Proximal DVT (above the knee) is more likely to cause pulmonary embolism. Distal DVT (below the knee) has a lower risk.
Prognosis varies:
- Many DVTs resolve without complications.
- Post-thrombotic syndrome occurs in a significant proportion of patients long-term.
- Recurrence risk is substantial.
- Mortality is associated with pulmonary embolism and underlying conditions.
Complications
Major DVT complications include:
- Pulmonary embolism (potentially fatal)
- Post-thrombotic syndrome (chronic venous insufficiency)
- Bleeding from anticoagulation
Postoperative and Rehabilitation Care
Thromboprophylaxis in hospitalized patients includes pharmacological (heparins, NOACs, aspirin, warfarin) and mechanical (compression stockings, pneumatic compression) measures. NOACs, particularly apixaban, may offer a favorable profile for extended thromboprophylaxis.
Deterrence and Patient Education
Patient education is crucial for DVT prevention and management:
- Encourage ambulation and physical activity.
- Promote compression stocking use in at-risk individuals.
- Advise smoking cessation.
Enhancing Healthcare Team Outcomes
Optimal DVT management requires an interprofessional team including clinicians, specialists, nurses, pharmacists, physical therapists, and vascular technicians. Prevention, early diagnosis, and coordinated care are essential to improve patient outcomes and reduce healthcare costs. Nurses and pharmacists play key roles in patient education, prophylaxis implementation, and medication management.
Conclusion
Differential diagnosis of deep vein thrombosis is a critical clinical skill due to the non-specific nature of its signs and symptoms. A systematic approach incorporating risk assessment, clinical evaluation, appropriate investigations (D-dimer, ultrasound), and a broad consideration of alternative diagnoses is essential for accurate diagnosis and timely management. Understanding the conditions that mimic DVT, from cellulitis to Baker’s cysts and systemic diseases, allows for targeted evaluation and prevents misdiagnosis, ultimately improving patient care and outcomes in this common and potentially life-threatening condition.
References
[List of references as in the original article]
Disclosure: