Introduction
Head injury, encompassing a spectrum of conditions from mild concussions to severe traumatic brain injuries (TBIs), poses a significant diagnostic challenge in clinical practice. A concussion, often referred to as mild traumatic brain injury (mTBI), is defined as a traumatically induced transient disturbance of brain function. While concussions are generally self-limiting, it’s crucial to accurately diagnose them and differentiate them from other conditions that may present with similar symptoms. This article provides a comprehensive overview of the Differential Diagnosis For Head Injury, focusing on concussions, to aid healthcare professionals in the evaluation and management of patients presenting with head trauma. Understanding the nuances of differential diagnosis is paramount for appropriate patient care, ensuring timely intervention and preventing potential complications.
Etiology of Head Injury
Head injuries can arise from various mechanisms, broadly categorized as direct and indirect trauma. Direct head injuries involve a direct blow to the head, commonly seen in sports-related collisions, falls, or assaults. Indirect injuries occur when forces transmitted to the head from other parts of the body cause rapid acceleration and deceleration of the brain within the skull. Whiplash injuries from motor vehicle accidents are a prime example of indirect head trauma leading to concussion. Recognizing the mechanism of injury is a crucial first step in the differential diagnosis, as it helps to contextualize the patient’s symptoms and guide further evaluation.
Epidemiology of Concussions
Concussions are a widespread public health concern. In the United States alone, millions of traumatic brain injuries occur annually, with a significant proportion being concussions. While sports-related concussions are frequently studied, they represent only a fraction of overall cases. Motor vehicle accidents, falls, and assaults are major contributors to concussion incidence across all age groups. The prevalence and varied causes of concussions highlight the importance of considering head injury in a broad range of clinical scenarios and maintaining a robust differential diagnosis.
Pathophysiology of Concussion
The pathophysiology of concussion is complex and involves a cascade of neurochemical and neurometabolic events. At a cellular level, concussions are considered functional rather than structural injuries, meaning symptoms arise from disturbances in brain function without gross anatomical damage visible on standard imaging. The rapid acceleration and deceleration forces disrupt neuronal membranes, leading to ion channel dysfunction, neurotransmitter release, and altered cerebral blood flow and glucose metabolism. These physiological disruptions manifest as the diverse symptoms associated with concussion. Understanding the pathophysiology helps in appreciating why diagnostic imaging is often normal in concussions and why clinical assessment is paramount for diagnosis and differential diagnosis.
History and Physical Examination in Head Injury
A thorough history and physical examination are the cornerstones of evaluating a potential head injury and formulating a differential diagnosis.
History Taking
Crucial aspects of the history include:
- Mechanism of Injury: Details about how the injury occurred, including the force of impact, direction, and any associated events like loss of consciousness or amnesia.
- Symptom Onset and Progression: When did symptoms begin? Have they worsened, improved, or remained stable? Note the specific symptoms experienced by the patient across different domains.
- Symptom Domains: Concussion symptoms typically fall into four domains:
- Affective/Emotional: Irritability, mood changes, anxiety, depression.
- Cognitive: Confusion, disorientation, amnesia (retrograde or anterograde), “brain fog,” difficulty concentrating, slowed processing speed.
- Physical/Somatic: Headache, dizziness, balance problems, nausea, vomiting, visual disturbances (blurred vision, double vision), sensitivity to light or sound.
- Sleep: Drowsiness, insomnia, hypersomnia.
- Loss of Consciousness (LOC): While LOC is not always present in concussion (occurring in less than 10% of cases), its presence and duration should be documented as it may suggest a more significant injury or influence the differential diagnosis.
- Prior Concussions: History of previous concussions, their severity, and recovery duration are important prognostic factors and can influence the current presentation.
- Pre-existing Conditions: Pre-existing conditions such as migraines, mood disorders, learning disabilities, and sleep disorders can complicate the clinical picture and need to be considered in the differential diagnosis.
Physical Examination
The physical examination should be comprehensive and include:
- Scalp and Skull Examination: Inspect for lacerations, contusions, hematomas, or signs of skull fracture.
- Cervical Spine Examination: Assess for neck pain, tenderness, and range of motion to rule out cervical spine injury, especially in trauma cases.
- Neurological Examination:
- Mental Status: Evaluate orientation, attention, memory, and higher cognitive functions.
- Cranial Nerves: Assess pupillary response, extraocular movements (saccades, smooth pursuits, convergence), facial sensation and movement, hearing, and balance.
- Motor Examination: Assess strength, tone, and reflexes in all extremities.
- Sensory Examination: Evaluate sensation to light touch, pain, and proprioception.
- Cerebellar Function: Assess balance, coordination (finger-to-nose, heel-to-shin), and gait.
- Vestibular and Balance Assessment: Specific tests for balance and vestibular function, such as Romberg test and tandem gait, are important in concussion evaluation.
- Emotional and Behavioral Assessment: Observe the patient’s affect, mood, and behavior, comparing to baseline if possible, to identify emotional or behavioral disturbances.
Alt text: Components of the Sports Concussion Assessment Tool 6th Edition (SCAT6), outlining tests for immediate assessment of athletes suspected of concussion, including symptom evaluation, cognitive assessment, balance examination, and coordination tests.
Standardized concussion assessment tools like the Sports Concussion Assessment Tool 6 (SCAT6) can be used to systematically evaluate athletes and others with suspected concussion. These tools aid in documenting symptoms, cognitive deficits, and physical signs, facilitating a more objective assessment. However, it’s crucial to remember that these tools are adjuncts to clinical judgment and do not replace a comprehensive history and physical exam in differential diagnosis.
Evaluation and Diagnostic Testing in Head Injury
The diagnosis of concussion is primarily clinical, based on the history and physical exam. However, diagnostic testing plays a crucial role in the differential diagnosis of head injury, primarily to rule out more serious conditions.
Neuroimaging
- Computed Tomography (CT) Scan: Head CT is the neuroimaging modality of choice in the acute setting, particularly in the emergency department. It is highly sensitive for detecting acute intracranial hemorrhage (epidural hematoma, subdural hematoma, subarachnoid hemorrhage), skull fractures, and large contusions – conditions that require immediate neurosurgical intervention and must be differentiated from concussion. Clinical decision rules like the Canadian CT Head Rule and PECARN guidelines help clinicians decide when CT imaging is necessary in minor head injury. However, it’s important to emphasize that a normal CT scan does not rule out a concussion, as concussions are functional injuries without macroscopic structural damage.
- Magnetic Resonance Imaging (MRI): MRI is generally not indicated in the acute evaluation of concussion when CT is negative and there are no red flags. However, MRI may be considered in patients with persistent post-concussive symptoms (PCS) lasting beyond a few weeks, or when there is suspicion of other intracranial pathology not readily visible on CT. MRI is more sensitive than CT for detecting subtle brain injuries, such as diffuse axonal injury, small contusions, and white matter lesions, which might contribute to prolonged symptoms. In the differential diagnosis, MRI can help exclude conditions like multiple sclerosis, brain tumors, or vascular malformations that could mimic PCS.
Biomarkers
Research is ongoing into serum biomarkers for concussion diagnosis and prognosis. Biomarkers like ubiquitin C-terminal hydrolase-L1 (UCH-L1) and glial fibrillary acidic protein (GFAP) have shown promise in early detection of brain injury. However, at present, serum biomarkers are not routinely used in clinical practice for concussion diagnosis or differential diagnosis. Their role is still largely investigational.
Neuropsychological Testing
Formal neuropsychological testing, performed by a neuropsychologist, can provide a detailed assessment of cognitive functions affected by concussion, including attention, memory, processing speed, and executive functions. While not essential for the initial diagnosis of concussion, neuropsychological testing can be valuable in:
- Establishing Baseline Function: Baseline testing in athletes can be helpful for comparison after a suspected concussion.
- Monitoring Recovery: Serial testing can track cognitive recovery and guide return-to-activity decisions.
- Differential Diagnosis: Neuropsychological profiles can help differentiate cognitive deficits due to concussion from those related to pre-existing learning disabilities, ADHD, anxiety, depression, or other conditions.
Differential Diagnosis of Head Injury
The differential diagnosis of head injury varies depending on the timing post-injury – acute versus post-acute/chronic.
Acute Differential Diagnosis (Immediately after Head Injury)
In the immediate aftermath of a head injury, the primary differential diagnosis focuses on ruling out serious, life-threatening conditions that require immediate medical or surgical intervention. These include:
- Intracranial Hemorrhage: Epidural hematoma, subdural hematoma, subarachnoid hemorrhage. These are typically detected by CT scan and often present with focal neurological deficits, altered level of consciousness, or rapidly deteriorating clinical status.
- Skull Fracture: Can be linear, depressed, or basilar. Basilar skull fractures may present with specific signs like raccoon eyes (periorbital ecchymosis), Battle’s sign (retroauricular ecchymosis), CSF rhinorrhea, or CSF otorrhea.
- Cervical Spine Injury: Especially important to consider in trauma patients. Neck pain, neurological deficits, or restricted neck movement should raise suspicion. Cervical spine immobilization and imaging (X-ray, CT) are crucial.
- Diffuse Axonal Injury (DAI): A more severe form of TBI involving widespread microscopic damage to axons. Often associated with prolonged loss of consciousness and significant cognitive impairment. May be subtle on initial CT but more evident on MRI.
- Cerebral Contusion: Bruising of brain tissue. Can be seen on CT or MRI. Location and size can vary, and clinical presentation depends on the area affected.
- Seizure: Post-traumatic seizures can occur immediately or within the first week after head injury. Epilepsy needs to be considered in the longer-term differential diagnosis if seizures persist.
- Hypoxic-Ischemic Brain Injury: If the head injury is associated with respiratory compromise or hypotension, hypoxic-ischemic brain injury should be considered.
Post-Acute and Chronic Differential Diagnosis (Post-Concussive Syndrome)
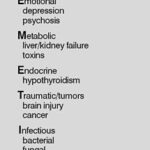
When symptoms persist beyond the expected recovery period for concussion (typically weeks to months), the differential diagnosis expands to include conditions that can mimic post-concussive syndrome (PCS). It becomes crucial to differentiate PCS from:
- Migraine and Headache Disorders: Post-traumatic headache is a common PCS symptom. However, pre-existing migraine disorders can be exacerbated by head injury, or new-onset migraines can develop. Features like headache quality, associated symptoms (photophobia, phonophobia, aura), and response to migraine-specific treatments can help differentiate migraine from PCS-related headache.
- Mental Health Disorders:
- Anxiety Disorders: Generalized anxiety disorder, panic disorder, post-traumatic stress disorder (PTSD). Symptoms like anxiety, irritability, sleep disturbance, and concentration problems overlap with PCS. However, PTSD typically has a clear traumatic event trigger and involves intrusive memories, avoidance, and hyperarousal.
- Depressive Disorders: Major depressive disorder, adjustment disorder with depressed mood. Symptoms like low mood, fatigue, sleep disturbance, and cognitive difficulties can be seen in both PCS and depression. Assessing for anhedonia, guilt, and suicidal ideation is important in differentiating depression.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Pre-existing ADHD can be unmasked or exacerbated by head injury, or PCS can cause attention and concentration problems that mimic ADHD. Detailed history of childhood symptoms and pre-injury cognitive function is helpful.
- Sleep Disorders: Insomnia, hypersomnia, sleep apnea. Sleep disturbances are common in PCS. However, primary sleep disorders may pre-exist or develop independently of the head injury. Sleep studies may be needed to differentiate.
- Vestibular Disorders: Benign paroxysmal positional vertigo (BPPV), vestibular neuritis, labyrinthitis. Dizziness and balance problems are prominent PCS symptoms. Specific vestibular testing (Dix-Hallpike maneuver, caloric testing) can help diagnose primary vestibular disorders.
- Cervicogenic Headache and Neck Pain: Pain originating from the cervical spine can radiate to the head and mimic headache from concussion. Physical exam findings of neck tenderness, restricted range of motion, and pain provocation with neck movements can suggest cervicogenic headache.
- Temporomandibular Joint (TMJ) Disorders: TMJ pain and dysfunction can cause headaches, facial pain, and dizziness, potentially overlapping with PCS symptoms, particularly if the head injury involved jaw trauma.
- Vision Problems: Convergence insufficiency, accommodative dysfunction, and other vision problems can contribute to headache, dizziness, and concentration difficulties after head injury. Ophthalmological or neuro-ophthalmological evaluation may be necessary.
- Medication Side Effects: Certain medications can cause symptoms like fatigue, dizziness, cognitive impairment, or headache, which could be misinterpreted as PCS, especially if medications were started around the time of injury.
Alt text: Axial view of a normal computed tomography (CT) scan of the brain in a patient with concussion, demonstrating the absence of visible structural abnormalities, emphasizing that concussion is a functional injury.
Management and Treatment of Concussion
Management of concussion primarily involves supportive care and a gradual, stepwise return to activity. While specific treatments for concussion are limited, addressing symptoms and co-existing conditions is crucial in the differential diagnosis and management process.
- Rest and Activity Modification: Initially, a brief period of physical and cognitive rest (24-48 hours) is recommended. Prolonged strict rest is no longer advised. Gradual return to activity should be guided by symptom tolerance.
- Symptom Management:
- Headache: Over-the-counter analgesics like acetaminophen or NSAIDs can be used for headache relief, provided they do not mask worsening symptoms or have contraindications.
- Dizziness and Balance Problems: Vestibular rehabilitation therapy can be effective for persistent dizziness and balance issues.
- Sleep Disturbances: Good sleep hygiene practices are essential. Medications for sleep should be used cautiously and under medical supervision, considering potential cognitive effects.
- Mood and Anxiety Symptoms: Cognitive-behavioral therapy (CBT) and other psychological therapies can be beneficial for managing emotional symptoms. In some cases, medication may be considered for co-existing anxiety or depression, but should be carefully weighed against potential side effects.
- Rehabilitation Therapies: Physical therapy, occupational therapy, and speech therapy may be indicated depending on the specific symptom profile and functional deficits.
- Return to Activity/Sport Protocol: A structured, gradual return-to-activity protocol is crucial for athletes and active individuals. This typically involves progressing through stages of increasing physical and cognitive exertion, with medical clearance required before full return to sport.
Conclusion
Differential diagnosis for head injury, particularly concussion, is a complex and nuanced process. It requires a thorough understanding of the mechanisms of injury, pathophysiology, clinical presentation, and potential mimicking conditions. While concussion itself is a clinical diagnosis, diagnostic testing, especially neuroimaging, plays a critical role in ruling out more severe and potentially life-threatening conditions in the acute setting. In the post-acute phase, differentiating PCS from other medical and psychiatric conditions becomes paramount. A comprehensive approach involving detailed history, careful physical and neurological examination, appropriate use of diagnostic testing, and consideration of pre-existing conditions is essential for accurate diagnosis and effective management of patients with head injury. This detailed differential diagnostic approach ensures that patients receive the correct diagnosis and targeted treatment, optimizing their recovery and long-term outcomes.