Retinoblastoma, the most common primary intraocular malignancy in children, presents with diverse clinical features that are crucial for early detection and differential diagnosis in primary eye care settings. Recognizing these varied presentations is the first step towards prompt referral and effective management. This article details the key clinical presentations of retinoblastoma, emphasizing aspects relevant to primary eye care professionals.
Retinoblastoma’s growth patterns significantly influence its clinical appearance. Tumors originating from the inner retinal layers and growing into the vitreous cavity are termed endophytic retinoblastomas. Conversely, exophytic tumors arise from the outer layers, invading the subretinal space and causing retinal detachment. Mixed growth patterns combine both endophytic and exophytic characteristics. A less common variant, the diffuse infiltrating retinoblastoma, grows subtly within the retinal layers without forming a distinct mass, often mimicking inflammatory conditions, which can pose diagnostic challenges.
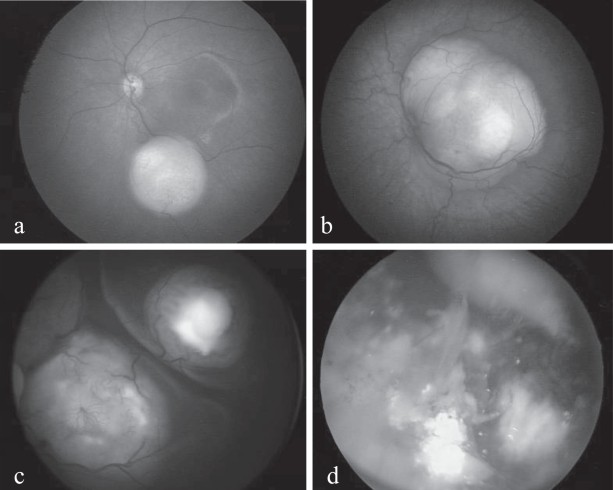
Endophytic retinoblastoma typically manifests as single or multiple yellowish-white (due to calcifications) or pinkish (due to vascularization) intraretinal tumors. These tumors may be round or oval and exhibit their own network of blood vessels, which can appear enlarged and twisted. A hallmark of endophytic tumors is their propensity to seed into the vitreous, creating floating tumor cells that resemble “vitreous snowballs” or haze during ophthalmoscopic examination.
Exophytic retinoblastoma, in contrast, grows outward towards the choroid, leading to retinal detachment. The detached retina can obscure the underlying tumor mass, making diagnosis more challenging. Subretinal seeding, tumor cells spreading within the fluid beneath the retina, can also occur in exophytic forms. Both endophytic and exophytic retinoblastomas are characterized by calcifications, appearing as chalky white patches within the tumor, a highly suggestive diagnostic feature. Vitreous and subretinal seeding, along with calcifications, are virtually pathognomonic for retinoblastoma and should raise immediate suspicion during primary eye examinations.
The diffuse infiltrating form of retinoblastoma presents a unique diagnostic challenge. It appears as a subtle, greyish retinal infiltration without a distinct mass or calcifications. This form can be easily mistaken for inflammatory conditions like uveitis, especially as it may eventually manifest as pseudo-hypopyon, an accumulation of inflammatory cells in the anterior chamber. Careful examination and a high index of suspicion are critical to avoid misdiagnosis in these cases.
Retinoma, or retinocytoma, represents an inactive, spontaneously regressed form of retinoblastoma. It is characterized by homogenous, greyish, translucent masses with calcifications and pigment changes at the tumor borders. Retinoma can mimic a treated retinoblastoma, but it occurs without any prior intervention. Distinguishing retinoma from active retinoblastoma is essential for appropriate management and genetic counseling.
In hereditary retinoblastoma, particularly the bilateral form, there is an increased risk of trilateral retinoblastoma, which involves the presence of an intracranial neuroblastic tumor, often pinealoblastoma, in addition to retinoblastoma. This association underscores the systemic nature of hereditary retinoblastoma and the importance of considering extraocular manifestations. Furthermore, children with the RB1 gene mutation are at increased lifetime risk for other cancers, highlighting the need for long-term surveillance.
Conclusion
Recognizing the diverse clinical presentations of retinoblastoma is paramount for primary eye care providers. Key diagnostic clues include leukocoria (white pupil), strabismus, and findings during fundus examination such as endophytic or exophytic masses, vitreous or subretinal seeding, and calcifications. Understanding these signs enables effective differential diagnosis in primary eye care, facilitating timely referral to specialist centers and improving outcomes for children with retinoblastoma. Further resources and downloadable guides on differential diagnosis in primary eye care are available to enhance clinical practice and ensure optimal patient care.