Hearing loss is a significant global health issue, impacting millions worldwide and becoming increasingly prevalent across all age groups. As automotive repair experts at xentrydiagnosis.store, understanding the intricacies of human sensory perception, particularly hearing, might seem tangential. However, recognizing the challenges faced by individuals with hearing impairments is crucial for effective communication and customer service in our field. Moreover, a deeper understanding of auditory conditions can enhance our problem-solving skills and diagnostic approaches, applicable even to complex automotive issues.
This article provides a detailed exploration of the Differential Diagnosis Of Deafness, aiming to equip you with knowledge comparable to that of a medical professional in this specific domain. While our primary expertise lies in vehicle diagnostics, broadening our understanding of diagnostic principles in other fields, such as medicine, can sharpen our analytical abilities.
Understanding Hearing Impairment: Definitions and Terminology
Hearing impairment, broadly defined, refers to any reduction in hearing ability, ranging from subtle difficulties to complete deafness. Synonyms include “hardness of hearing” and “hypacusis.” It’s crucial to distinguish deafness from other auditory disturbances like hyperacusis (sound oversensitivity), fluctuating hearing, and tinnitus (ringing in the ears). Deafness is a symptom stemming from disruptions at various points within the auditory system:
- Conductive Hearing Loss: Issues in the outer or middle ear that prevent sound from effectively reaching the inner ear.
- Sensorineural Hearing Loss: Damage to the inner ear (cochlea) or the auditory nerve, affecting sound perception and transmission to the brain.
- Central Hearing Loss: Dysfunction in the auditory pathways within the brain or the auditory cortex, impacting sound processing.
Prevalence of Hearing Impairment
Epidemiological studies indicate that a significant portion of the population experiences hearing loss requiring intervention. In Germany, approximately 19% of the population is estimated to have a hearing impairment requiring treatment. This figure is based on a hearing loss threshold of 40 dB in at least five frequencies (0.5 to 4 kHz). Using the World Health Organization’s (WHO) lower threshold of 25 dB, the actual prevalence could be even higher. Congenital bilateral hearing loss, present at birth, occurs in about 1.2 per 1000 newborns.
The most common type of hearing loss in children is transient conductive hearing loss due to middle ear fluid buildup. In adults, age-related sensorineural hearing loss (presbycusis) is most prevalent, affecting around 40% of individuals over 65. Other common causes include chronic middle ear infections and noise-induced hearing loss.
Recognizing the Clinical Features of Hearing Impairment
Early stages of hearing loss can be subtle, with individuals often compensating unconsciously. Common signs include:
- Increasing the volume on radios or televisions.
- Turning one ear towards sound sources (in cases of unilateral hearing loss).
- Difficulty understanding speech in noisy environments.
- Asking for repetition frequently.
- Providing inappropriate responses due to mishearing.
- Speaking louder than usual.
- Increased reliance on visual cues like lip-reading.
Classifying Hearing Impairment: A Diagnostic Framework
Classifying hearing impairment is crucial for accurate diagnosis and effective management. The primary classifications are based on:
- Severity: Quantified by pure-tone audiometry, as outlined by the WHO (Table 1).
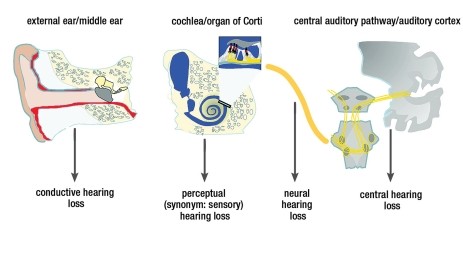
- Topography and Function: Differentiating between conductive, sensorineural, and central hearing loss (Figure 1).
Additional classifications consider:
- Age of onset (childhood vs. old age).
- Temporal course (sudden vs. progressive).
- Specific patterns on audiograms.
Table 1: WHO Classification of Hearing Impairment Severity
| Grades of Hearing Impairment | Mean Hearing Loss (dB) | Clinical Findings | Recommendations |
|---|---|---|---|
| 0 – No Impairment | ≤ 25 dB | No or very slight hearing problems; hears whispers. | Counseling, follow-up; evaluate surgery for conductive loss. |
| 1 – Slight Impairment | 26-40 dB | Hears normal voice at 1 meter. | Counseling, hearing aids may be considered; evaluate surgery for conductive or mixed loss. |
| 2 – Moderate Impairment | 41-60 dB | Hears raised voice at 1 meter. | Hearing aids recommended; evaluate surgery for conductive or mixed loss. |
| 3 – Severe Impairment | 61-80 dB | Hears some words when shouted into better ear. | Hearing aids needed; consider implanted aids or cochlear implant if external aids fail; lip-reading and signing. |
| 4 – Profound Impairment/Deafness | ≥ 81 dB | Unable to hear even shouted voice. | Cochlear or brainstem implant often indicated after hearing aid failure; lip-reading and signing. |

*Mean hearing loss is calculated for each ear at 500 Hz, 1000 Hz, 2000 Hz, and 4000 Hz. Modified from WHO guidelines.
Conductive vs. Sensorineural Hearing Loss: Distinguishing the Mechanisms
Understanding the difference between conductive and sensorineural hearing loss is fundamental to differential diagnosis.
Conductive Hearing Loss: Occurs when sound transmission is blocked in the outer or middle ear. Imagine a vehicle’s exhaust system obstruction – sound (or exhaust) cannot pass efficiently. Causes can include earwax buildup, middle ear infections, or ossicle damage. Audiometry reveals an “air-bone gap,” where bone conduction thresholds are better than air conduction thresholds.
Sensorineural Hearing Loss: Results from damage within the inner ear (cochlea) or auditory nerve. This is akin to engine damage in a car – the sound signal is generated but not properly processed. Common causes include aging, noise exposure, and certain medications. Audiometry shows air and bone conduction thresholds are similarly affected, without a significant air-bone gap.
Tone Audiometry: A Key Diagnostic Tool
Tone audiometry is crucial for differentiating these types of hearing loss.
- Sensorineural Hearing Loss: Air and bone conduction curves on the audiogram are superimposed, indicating inner ear or nerve dysfunction.
- Conductive Hearing Loss: Air and bone conduction curves are separated, showing a problem in sound conduction pathways before the inner ear.
Common Causes of Hearing Impairment: A Site-Specific Approach
To effectively perform a differential diagnosis of deafness, we must consider the anatomical location of potential issues.
External Auditory Canal
Conductive Hearing Loss: Obstruction of the ear canal is a common cause of conductive hearing loss.
- Cerumen Impaction (Earwax Buildup): Simple blockage by earwax.
- Canal Atresia: Congenital absence or closure of the ear canal, causing significant hearing loss (up to 60 dB). Bilateral atresia in newborns requires early intervention with bone-conduction hearing aids to support speech and language development.
Tympanic Membrane, Tympanic Cavity, and Ossicular Chain
Transient Conductive Hearing Loss: Temporary blockage of the Eustachian tube is a frequent cause of transient conductive hearing loss, especially in children.
- Eustachian Tube Dysfunction: Reduced pressure in the middle ear due to Eustachian tube blockage, often from colds or allergies.
- Tympanic Effusion (Middle Ear Fluid): Prolonged Eustachian tube blockage can lead to fluid buildup in the middle ear, causing conductive hearing loss (up to 40 dB). Common in children due to narrower Eustachian tubes and susceptibility to infections. Children with craniofacial abnormalities like cleft palate are at higher risk. Persistent tympanic effusion (over 3 months) requires treatment like tympanic drainage and adenoidectomy to prevent speech development delays.
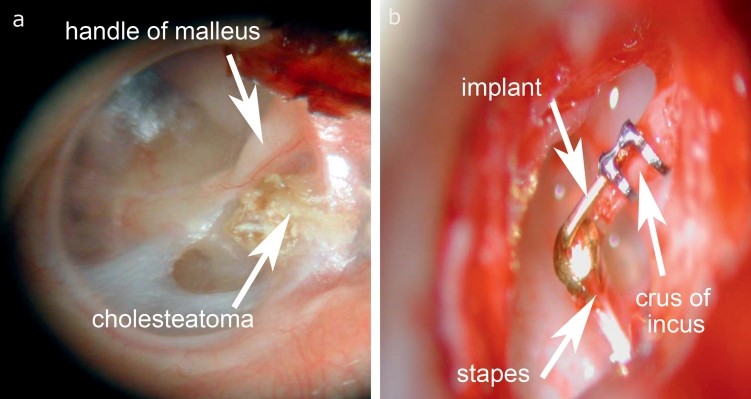
Permanent Conductive Hearing Loss: Chronic middle ear infections are a primary cause.
- Chronic Otitis Media: Persistent bacterial infection of the middle ear mucosa or bone (cholesteatoma). Inflammation and tissue damage disrupt sound transmission. Surgical intervention is often necessary to eradicate infection and reconstruct the ossicular chain.
Middle Ear: Otosclerosis
Permanent Conductive Hearing Loss:
- Otosclerosis: Abnormal bone remodeling in the inner ear capsule, often affecting the stapes bone and causing stapes fixation. Leads to conductive hearing loss, more pronounced at lower frequencies. More common in women and typically manifests between 15 and 40 years old. Microsurgical stapedoplasty is highly effective in restoring hearing.
Perceptual (Sensory) Hearing Impairment: Focusing on the Inner Ear
Sensory Hearing Loss: Arises from dysfunction within the organ of Corti in the cochlea. Damage to the outer hair cells is most common.
- Organ of Corti Dysfunction: The organ of Corti transduces sound vibrations into neural signals. Outer hair cells amplify sound signals through a mechanoelectrical process. Damage disrupts this process, leading to hearing loss. Characteristics include elevated bone conduction thresholds, recruitment (abnormal loudness perception), and impaired frequency selectivity.
Permanent Sensorineural Hearing Loss in Childhood: Congenital Deafness
Congenital sensorineural hearing loss is a significant concern.
- Genetic Factors: A substantial portion (25%) of congenital sensorineural hearing loss is genetic, with non-syndromic causes being more common (70%) than syndromic (30%). Autosomal recessive inheritance is the most frequent pattern in non-syndromic cases. Mutations in connexin 26 and 30 genes are common causes, affecting ion transport in hair cells.
- Acquired Factors: Infections (TORCH infections, meningitis), metabolic issues (hyperbilirubinemia), toxins (alcohol, certain drugs), and birth trauma can also cause congenital hearing loss.
- Idiopathic Causes: A significant percentage (57%) of congenital sensorineural hearing loss has undetermined causes.
Acute Sensory Hearing Loss in Adulthood: Sudden Deafness
Acute sensory hearing loss can have various triggers.
- Traumatic Causes: Skull fractures or blast trauma (e.g., explosions, firecrackers). Blast trauma can rupture the tympanic membrane and cause immediate hearing loss with tinnitus.
- Noise-Induced Hearing Loss: Exposure to loud noise over time (e.g., concerts, occupational noise). Can cause metabolic stress in hair cells, leading to temporary or permanent hearing loss, often affecting high frequencies (around 4 kHz) and causing tinnitus.
- Toxic Causes: Ototoxic medications (aminoglycoside antibiotics, chemotherapy drugs, loop diuretics, salicylates, quinine) and toxins (industrial chemicals, abused substances, bacterial/viral toxins). Monitoring serum drug levels can help minimize ototoxicity.
Sudden Sensorineural Hearing Loss (SSNHL): An Audiological Emergency
SSNHL is characterized by rapid onset hearing loss, often with no identifiable cause.
- Idiopathic SSNHL: In most cases (71%), no specific cause is found. Viral, vascular, or immunological factors are suspected.
- Identifiable Causes: Systemic infections, ear diseases (cholesteatoma), trauma, cardiovascular disease, and paraneoplastic syndromes can also trigger SSNHL.
Permanent Sensorineural Hearing Loss in Adulthood: Age and Noise
- Presbycusis (Age-Related Hearing Loss): Progressive, bilateral sensorineural hearing loss, typically starting after age 50. Affects high frequencies initially. Caused by age-related changes in the inner ear, including microvascular damage, ischemia, and oxidative stress in hair cells and auditory pathways.
- Noise-Induced Hearing Loss (NIHL): Prolonged exposure to loud noise (occupational or recreational) damages hair cells. Characteristically shows a “noise notch” around 4 kHz on audiograms.
Neural Hearing Loss: Issues with the Auditory Nerve
Neural hearing loss involves the auditory nerve or its pathways.
- Acoustic Neuroma (Vestibular Schwannoma): Benign tumor on the vestibular nerve, often affecting the auditory nerve. A common cause of neural hearing loss, typically unilateral. Requires investigation with brainstem evoked response audiometry (BERA) and MRI.
- Other Tumors: Meningiomas, chordomas, chondrosarcomas in the petrous bone or cerebellopontine angle.
- Auditory Neuropathy Spectrum Disorder (ANSD): Affects the synapses between inner hair cells and the auditory nerve. Disrupts the timing of neural signals, impacting speech understanding, especially in noise.
Central Hearing Loss: Brain-Based Auditory Processing Issues
Central hearing loss involves dysfunction in the brain’s auditory pathways or cortex.
- Central Auditory Processing Disorder (CAPD): Difficulty processing auditory information in the brain, despite normal peripheral hearing. Can affect sound localization, speech understanding in noise, and auditory memory. Often associated with developmental disorders, learning disabilities, and attention deficits.
- Brainstem Lesions: Infarction, hemorrhage, tumors, multiple sclerosis affecting the brainstem auditory pathways can cause central hearing loss, often accompanied by other neurological symptoms.
- Cortical Lesions: Damage to the auditory cortex due to stroke, trauma, or tumors can result in complex auditory processing deficits.
Audiological Testing: Essential Tools for Differential Diagnosis
A comprehensive audiological evaluation is crucial for accurately diagnosing hearing loss and differentiating between its various types. Key components include:
- Simple Clinical Tests: Tuning fork tests (Rinne and Weber tests) and speech tests at varying distances provide initial clues about hearing function and type of loss.
- Pure-Tone and Speech Audiometry: Quantifies hearing thresholds at different frequencies and assesses speech understanding ability.
- Impedance Audiometry (Tympanometry and Acoustic Reflex Testing): Evaluates middle ear function, helping to identify conductive hearing loss due to middle ear fluid or ossicular chain problems.
- Supraliminal Tests: Assess loudness recruitment, adaptation, and other auditory phenomena to further characterize sensorineural hearing loss.
- Otoacoustic Emissions (OAEs): Objective test measuring the function of outer hair cells in the cochlea, useful in differentiating sensory from neural hearing loss and in neonatal hearing screening.
- Auditory Brainstem Response (ABR): Objective test assessing the neural pathway from the auditory nerve to the brainstem, crucial for diagnosing neural hearing loss, particularly acoustic neuroma, and for infant hearing assessment.
Differential Diagnosis: A Summary Table
Table 2 provides a concise overview of the differential diagnosis of deafness, summarizing causes, clinical features, and audiological findings for conductive, sensory, neural, and central hearing loss.
Table 2: Differential Diagnosis of Hearing Impairment Syndromes
| Feature | Conductive Hearing Loss | Sensory Hearing Loss | Neural Hearing Loss | Central Hearing Loss |
|---|---|---|---|---|
| Cause | Mechanical obstruction in outer/middle ear. | Dysfunction of hair cells or synapses in cochlea. | Cochlear nerve dysfunction; delayed impulse conduction. | Dysfunction of auditory pathway or cortex (processing, synchronization, recognition). |
| Clinical Features | Reduced sound intensity; altered frequency perception. | Loss of intensity and dynamics; distorted perception; recruitment. | Similar to sensory loss, often unilateral; speech perception worse than tone perception. | May have normal tone perception; impaired rapid speech processing, sound localization, speech understanding in noise, auditory memory. |
| Differential Diagnosis | Acute: Cerumen, tubal catarrh, effusion, perforation, otitis. Permanent: Stenosis, ossicle defect, cholesteatoma, otosclerosis. | Acute: Sudden SNHL, noise trauma, labyrinthitis. Hereditary/Permanent: Presbycusis, NIHL, ototoxicity, genetic hearing loss. | Acoustic neuroma, tumors of petrous bone/CPA, compression syndromes. | Infarction, hemorrhage, tumor, multiple sclerosis, auditory processing disorder. |
| Audiological Testing | Tuning fork tests, pure-tone audiometry, impedance audiometry. | Tuning fork tests, pure-tone audiometry, speech audiometry, otoacoustic emissions. | Pure-tone audiometry, speech audiometry, supraliminal tests, ABR. | Hearing at a distance test, pure-tone audiometry, speech audiometry, supraliminal tests, ABR, specialized central auditory tests. |
Conclusion: Towards Accurate Diagnosis and Effective Management
Accurate differential diagnosis of deafness is paramount for guiding appropriate treatment and rehabilitation strategies. From conductive hearing loss treatable with surgery or hearing aids to sensorineural hearing loss requiring amplification or cochlear implantation, and central auditory processing disorders needing specialized therapy, each type demands a tailored approach.
As automotive experts, while we may not directly treat deafness, understanding the complexities of this condition highlights the importance of systematic diagnostics and problem-solving – skills directly transferable to our automotive work. Just as we meticulously diagnose vehicle malfunctions, a thorough approach to understanding hearing loss, as outlined in this guide, underscores the value of comprehensive assessment and targeted interventions in any field of expertise. For those seeking further information or experiencing hearing difficulties, consulting an audiologist or otolaryngologist is crucial for professional diagnosis and care.
