Introduction
Deep vein thrombosis (DVT), the formation of blood clots in deep veins, predominantly in the legs, stands as a significant health concern. While often associated with immobility and certain medical conditions, understanding DVT is crucial even for professionals outside direct patient care, including auto repair experts. This knowledge becomes relevant in scenarios involving workplace injuries, understanding employee health risks, and even in a broader understanding of human physiology which can sometimes be analogized to complex systems like automobiles – where blockages and flow issues are critical diagnostic considerations. DVT, a component of venous thromboembolism (VTE), ranks as the third leading cause of cardiovascular death, following myocardial infarction and stroke. Beyond the immediate threat of pulmonary embolism, recurrent thrombosis and post-thrombotic syndrome contribute significantly to long-term morbidity. Early and accurate diagnosis is paramount to mitigating these risks. This article aims to provide an in-depth exploration of the differential diagnosis of DVT, enhancing the original article by providing a more detailed and SEO-optimized resource for an English-speaking audience.
Etiology of Deep Vein Thrombosis
Risk Factors
Several factors elevate the risk of developing DVT. These can be broadly categorized based on their impact on coagulation.
Increased Risk of Coagulation
Conditions that predispose individuals to hypercoagulability are primary risk factors for DVT.
Constitutional Factors
Obesity, pregnancy, advanced age (over 60), surgery, critical care admission, dehydration, and cancer are well-established constitutional risk factors for DVT and VTE. Obesity, for instance, promotes hypercoagulability through elevated fibrinogen levels and reduced venous flow, particularly in the lower limbs. These factors, combined with coagulation factor abnormalities, increase the likelihood of venous thrombosis and thromboembolism, including fatal pulmonary embolisms, a leading cause of mortality in obese patients.
Risk factors can also be classified by duration:
-
Transient Risk Factors: These are temporary conditions that increase DVT risk. Examples include:
- Surgery with general anesthesia
- Hospitalization
- Cesarean section
- Hormone replacement therapy
- Pregnancy and the peripartum period
- Lower extremity injury with immobilization exceeding 72 hours. General anesthesia lasting over 30 minutes and hospitalization longer than 72 hours are significant transient risk factors.
-
Persistent Risk Factors: These are ongoing conditions that sustain an elevated DVT risk. Active cancers and specific medical conditions like systemic lupus erythematosus and inflammatory bowel disease fall into this category.
-
Unprovoked VTE: Risk factors that are neither transient nor persistent are classified as unprovoked VTE. Emerging research suggests links between lipid profiles and DVT risk. For example, higher triglyceride levels have been associated with an increased risk of lower extremity DVT, while higher total cholesterol and HDL-C levels may correlate with decreased risk.
Epidemiology of Deep Vein Thrombosis
Incidence and Prevalence
DVT and pulmonary embolism are often underdiagnosed due to their “silent” nature, frequently detected only during autopsy. The true incidence and prevalence are likely underestimated. Estimates suggest an annual DVT incidence of 80 per 100,000 individuals, with a lower limb DVT prevalence of approximately 1 per 1,000 people. In the United States, over 200,000 individuals develop venous thrombosis annually, with pulmonary embolism complicating 50,000 of these cases.
- Age: DVT is rare in children, with risk escalating with age, predominantly affecting individuals over 40.
- Gender: There is no definitive consensus on gender bias in DVT incidence.
- Ethnicity: Data from the United States indicates a higher DVT incidence and complication risk in African Americans and White individuals compared to Hispanic and Asian populations.
- Associated Diseases: In hospitalized settings, common conditions associated with DVT include malignancy, congestive heart failure, obstructive airway disease, and post-surgical states.
Pathophysiology of Deep Vein Thrombosis
The Virchow triad outlines the primary pathophysiological mechanisms contributing to DVT:
- Vessel Wall Damage: Injury to the endothelial lining of blood vessels can initiate the coagulation cascade.
- Turbulent Blood Flow: Stasis or abnormal blood flow patterns can promote clot formation by preventing dilution of clotting factors and hindering the influx of clotting inhibitors.
- Hypercoagulability: Conditions that increase the blood’s tendency to clot, as discussed in etiology, play a crucial role.
Thrombosis is a protective mechanism to prevent blood loss from damaged vessels. Fibrinolysis counteracts thrombosis. DVT triggers are often multifactorial, with varying contributions from each element of Virchow’s triad. Early thrombus interaction with the endothelium stimulates cytokine production and leukocyte adhesion, further promoting thrombosis. Thrombus propagation depends on the balance between coagulation and thrombolytic pathways. DVT is most common in the lower limbs, below the knee, often initiating in low-flow areas such as soleal sinuses and behind venous valve pockets. Emerging research explores a potential link between DVT and atherosclerosis (AS). Endothelial dysfunction, a key factor in DVT, could also contribute to AS, suggesting a potentially increased risk of subsequent AS in DVT patients.
Histopathology of Deep Vein Thrombosis
Following acute thrombus formation in veins, a remodeling process ensues. Neutrophils and macrophages infiltrate the fibrin clot over weeks, leading to cytokine release and eventual replacement of fibrin with fibroblasts and collagen. This remodeling and fibrosis can impair blood flow long after the acute thrombus resolves, contributing to chronic venous insufficiency and post-thrombotic syndrome.
History and Physical Examination in Deep Vein Thrombosis
Clinical presentation of acute lower extremity DVT varies based on thrombus location, extent, and occlusion degree. Symptoms can range from absent to severe swelling and cyanosis, potentially progressing to venous gangrene. Three main patterns are recognized: distal calf vein thrombosis, femoropopliteal thrombosis, and iliofemoral thrombosis. Symptoms typically worsen with proximal thrombus extension. Notably, up to 50% of acute DVT patients may present with non-specific or absent signs and symptoms. Postoperative patients are particularly prone to asymptomatic, distal, non-occlusive thrombi.
When present, DVT signs and symptoms may include:
- Pain
- Edema
- Erythema (redness)
- Tenderness
- Fever
- Prominent superficial veins
- Pain with passive foot dorsiflexion (Homan’s sign – low sensitivity and specificity)
- Peripheral cyanosis
Phlegmasia cerulea dolens, a severe form of DVT characterized by massive swelling, cyanosis, and pain, results from complete venous outflow obstruction. Advanced cases exhibit severe venous hypertension, collateral and microvascular thrombosis, potentially leading to venous gangrene. Venous gangrene is particularly associated with warfarin-induced protein C depletion in cancer patients or heparin-induced thrombocytopenia.
Clinical diagnosis of DVT based solely on signs and symptoms is unreliable due to their non-specificity. Symptoms can mimic other lower extremity disorders, necessitating exclusion of conditions like lymphedema, superficial venous thrombosis, and cellulitis. Calf pain and swelling are common presenting symptoms but lack both sensitivity and specificity for accurate DVT diagnosis. No single sign or symptom, or symptom combination, is sufficiently accurate to definitively diagnose or exclude DVT.
History Taking for Suspected DVT
- Pain (present in approximately 50% of patients)
- Redness
- Swelling (present in about 70% of patients)
Physical Examination Findings in DVT
- Limb edema (unilateral or bilateral if thrombus extends to pelvic veins)
- Red and warm skin with dilated superficial veins
- Tenderness along the deep veins
Evaluation and Diagnostic Modalities for Deep Vein Thrombosis
According to the Clinical-Etiology-Anatomy-Pathophysiology (CEAP) classification, deep veins include: inferior vena cava, iliac veins (common, internal, external), pelvic veins (gonadal, broad ligament), femoral veins (common, deep, femoral), popliteal vein, paired crural veins (anterior and posterior tibial, peroneal), and muscular veins (gastrocnemial, soleal).
National Institute for Clinical Excellence (NICE) guidelines recommend the following investigations:
- D-dimer Assay: Highly sensitive but not specific; elevated levels suggest fibrin degradation, but can be elevated in other conditions.
- Coagulation Profile: Baseline assessment of clotting factors, although often normal in acute DVT.
- Proximal Leg Vein Ultrasound: The primary imaging modality. Positive results (non-compressibility of veins) indicate DVT.
Diagnostic strategy is guided by DVT risk assessment. The Wells score is a common clinical probability assessment tool.
- Low Probability: Wells score 0-1.
- High Probability: Wells score ≥ 2.
Diagnostic Algorithm based on Wells Score:
-
Wells Score ≥ 2 (High Probability):
- Proximal leg vein ultrasound within 4 hours.
- Positive Ultrasound: Treat for DVT.
- Negative Ultrasound: D-dimer test.
- Positive D-dimer: Repeat ultrasound in 6-8 days.
- Negative D-dimer: DVT unlikely.
- If ultrasound within 4 hours is not feasible: D-dimer test and interim 24-hour parenteral anticoagulant dose. Ultrasound within 24 hours of request.
- Follow D-dimer/ultrasound results as above.
- Proximal leg vein ultrasound within 4 hours.
-
Wells Score < 2 (Low Probability):
- D-dimer test.
- Negative D-dimer: DVT unlikely.
- Positive D-dimer: Proximal leg vein ultrasound within 4 hours (or within 24 hours with interim anticoagulation if 4-hour ultrasound not possible).
- Positive Ultrasound: Treat for DVT.
- Negative Ultrasound: Consider repeat ultrasound in 6-8 days or further investigation based on clinical suspicion.
- D-dimer test.
Clinical decision rules like the Pulmonary Embolism Rule-Out Criteria (PERC) and Wells criteria aid in risk stratification. PERC-positive patients may require no further testing, while PERC-negative, low-probability Wells score patients may be ruled out with D-dimer. D-dimer, while sensitive, lacks specificity and should be used judiciously in low-probability patients without other conditions that could cause false positives. Age-adjusted D-dimer cutoffs may be considered in elderly patients.
Imaging Modalities for DVT Diagnosis
- Diagnostic Ultrasound (Duplex Ultrasound): The gold standard for DVT diagnosis. Assesses vein compressibility and blood flow.
- Vascular Studies (Plethysmography): Less common now, measures volume changes in limbs to detect venous obstruction.
- CT Venography: Used when ultrasound is inconclusive or to assess pelvic or abdominal veins. Involves IV contrast.
- Point-of-Care Ultrasound (POCUS): Rapid bedside ultrasound by emergency providers, particularly useful when 24-hour ultrasound access is limited. Can expedite diagnosis and treatment. Two-point compression (femoral and popliteal veins) or 2-region serial compression techniques are used.
POCUS Technique:
- Patient supine in frog-leg position, 20-30 degrees reverse Trendelenburg.
- High-frequency linear transducer (5-10 MHz) in transverse plane at inguinal ligament.
- Visualize common femoral vein distal to inguinal ligament.
- Apply pressure to vein; complete collapse indicates no DVT at that point.
- Continue distally along femoral vein to bifurcation of greater saphenous and deep femoral veins. Compress all venous structures.
- Proceed to popliteal fossa (laterally rotated leg, flexed knee).
- Transverse transducer in popliteal fossa; popliteal vein anterior to artery.
- Apply compression; observe for complete collapse. Compress proximal and distal to popliteal fossa.
Negative POCUS may require repeat testing in 1-2 weeks to rule out propagating calf DVT or D-dimer testing in select patients. Standard laboratory tests (coagulation status, blood count, renal function) should also be obtained.
Treatment and Management of Deep Vein Thrombosis
DVT treatment aims to prevent pulmonary embolism, reduce morbidity, and prevent post-thrombotic syndrome. Anticoagulation is the cornerstone of treatment. NICE guidelines recommend treating proximal DVT and pulmonary embolism, weighing anticoagulation risks against benefits for each patient.
Treatment strategies vary based on DVT etiology:
-
Cancer-Associated Thromboembolism: Low molecular weight heparin (LMWH) and factor Xa inhibitors (rivaroxaban) are preferred. Higher anticoagulation levels may be needed for newly diagnosed cancer, extensive VTE, or cancer treatment-related adverse effects (e.g., vomiting).
-
Preferred Oral Therapy: Rivaroxaban, edoxaban, and vitamin K antagonists (VKAs) are options for once-daily oral therapy.
-
Liver Disease: LMWH is recommended. Direct oral anticoagulants (DOACs) are contraindicated in elevated INR.
-
Renal Disease: VKAs are recommended for creatinine clearance < 30 ml/min. DOACs and LMWH should be avoided in end-stage renal disease.
-
Coronary Artery Disease History: VKAs, rivaroxaban, apixaban, and edoxaban are alternatives.
-
Dyspepsia/Gastrointestinal Bleeding History: VKAs and apixaban are preferred due to lower GI bleeding risk compared to other DOACs.
-
Poor Compliance Risk: VKA may be preferred, though some patients may be compliant with DOACs.
-
Thrombolytic Therapy Indication: Unfractionated heparin is indicated.
-
Potential Thrombolytic Reversal: Reversal agents for DOACs are not universally available.
-
Pregnancy: LMWH is the preferred anticoagulant due to limited placental transfer.
Treatment Duration Guidelines:
- LMWH or fondaparinux for 5 days or until INR > 2 for 24 hours (unfractionated heparin for renal failure/high bleeding risk).
- Vitamin K antagonists for 3 months.
- Cancer patients: Consider anticoagulation for 6 months with LMWH.
- Unprovoked DVT: Consider vitamin K antagonists beyond 3 months.
- Rivaroxaban (oral factor Xa inhibitor): Approved by FDA/NICE; no routine INR monitoring needed.
- Heparin-induced thrombocytopenia: Switch from heparin to fondaparinux if platelet count < 75,000.
Thrombolysis: Indications include:
- Symptomatic iliofemoral DVT
- Symptoms < 14 days duration
- Good functional status
- Life expectancy ≥ 1 year
- Low bleeding risk
Thrombolysis carries intracranial bleed risk; careful patient selection is crucial. Endovascular interventions (catheter-directed extraction, stenting, mechanical thrombectomy) are used with varying success.
Other Management Strategies:
- Compression Hosiery: Below-knee graduated compression stockings (> 23 mm Hg ankle pressure) for 2 years if no contraindications, to prevent post-thrombotic syndrome.
- Inferior Vena Cava Filters: For anticoagulation contraindications or recurrent emboli despite anticoagulation.
Newer Drugs:
Rivaroxaban, apixaban, dabigatran, edoxaban, betrixaban are newer factor Xa inhibitors for DVT prophylaxis. Typical DVT treatment duration is 3-6 months, longer for recurrent episodes (≥ 12 months) or cancer patients (long-term). Inferior vena cava filters are not recommended in acute DVT except in specific circumstances.
Differential Diagnosis of Deep Vein Thrombosis
Accurate diagnosis of DVT is crucial, but its symptoms can overlap with various other conditions. A thorough differential diagnosis is essential to ensure appropriate management and avoid misdiagnosis. Here’s a detailed Differential Diagnosis Of Deep Vein Thrombosis:
1. Cellulitis
- Distinguishing Features from DVT: Cellulitis is a bacterial skin infection, presenting with skin warmth, intense redness, and often skin breaks or entry points for bacteria. Pain in cellulitis is typically more superficial and localized to the skin, whereas DVT pain can be deeper and more diffuse. Fever and systemic signs are more common and pronounced in cellulitis. Edema in cellulitis is also often associated with skin changes and is not primarily due to venous obstruction. Ultrasound in cellulitis will not show a thrombus in the deep veins, which is the hallmark of DVT.
2. Post-thrombotic Syndrome
- Distinguishing Features from DVT: Post-thrombotic syndrome (PTS) is a chronic condition developing after DVT, characterized by persistent leg pain, swelling, skin changes (venous eczema, lipodermatosclerosis), and sometimes ulceration. PTS is a sequela of DVT, not a differential diagnosis for acute DVT. However, when evaluating a patient with chronic leg swelling and discomfort, differentiating between acute DVT and pre-existing PTS is important. History of prior DVT is key for PTS. Ultrasound may show chronic changes in veins in PTS, but the acute symptoms and signs suggesting new thrombus formation are typically absent.
3. Ruptured Baker’s Cyst (Popliteal Cyst Rupture)
- Distinguishing Features from DVT: A Baker’s cyst is a fluid-filled sac behind the knee. Rupture causes sudden onset calf pain and swelling, mimicking DVT. However, Baker’s cyst rupture often presents with ecchymosis (bruising) around the ankle (“crescent sign”) and calf, which is less common in DVT. Pain in Baker’s cyst rupture may be more localized to the calf and posterior knee. Ultrasound can differentiate: Baker’s cyst rupture will show fluid collection in the calf and popliteal fossa, while DVT ultrasound will demonstrate thrombus in the deep veins.
4. Trauma (Muscle Strain, Hematoma, Soft Tissue Injury)
- Distinguishing Features from DVT: Trauma-related leg pain and swelling usually have a clear history of injury. Pain is often localized to the injured area and can be reproduced with palpation of specific muscles or tissues. Ecchymosis and visible signs of injury (abrasions, lacerations) are common. While trauma can be a risk factor for DVT (due to immobility and vessel injury), in isolated trauma without other risk factors, DVT is less likely as the primary diagnosis. Ultrasound is crucial to rule out DVT if there is any clinical suspicion, especially in patients with risk factors for thrombosis.
5. Superficial Thrombophlebitis
- Distinguishing Features from DVT: Superficial thrombophlebitis involves thrombosis and inflammation of superficial veins, often visible and palpable as a tender, cord-like vein just beneath the skin surface. Redness and warmth are localized along the course of the superficial vein. Pain is typically more superficial and localized. While superficial thrombophlebitis itself is less likely to cause pulmonary embolism than DVT, it can sometimes propagate into the deep venous system. Ultrasound can distinguish between superficial and deep vein thrombosis.
6. Peripheral Edema (Heart Failure, Cirrhosis, Nephrotic Syndrome, Venous Insufficiency)
- Distinguishing Features from DVT: Peripheral edema from systemic conditions like heart failure, cirrhosis, or nephrotic syndrome is usually bilateral and symmetrical, affecting both legs equally. Pitting edema is common. Other systemic symptoms related to the underlying condition (e.g., shortness of breath in heart failure, jaundice in cirrhosis, proteinuria in nephrotic syndrome) are often present. Venous insufficiency edema is also typically bilateral, chronic, and worsened by prolonged standing. DVT edema is more often unilateral and acute or subacute in onset. Ultrasound is essential to rule out DVT in patients presenting with unilateral leg edema, even if systemic conditions are also present.
7. Venous or Lymphatic Obstruction (Non-thrombotic)
- Distinguishing Features from DVT: Non-thrombotic venous obstruction can be caused by external compression (e.g., tumor, mass) or intrinsic venous abnormalities. Lymphatic obstruction (lymphedema) results from impaired lymphatic drainage. Edema in venous obstruction may be unilateral or bilateral depending on the level of obstruction. Lymphedema is often non-pitting, chronic, and may involve the foot and toes, unlike typical DVT edema. Imaging (CT venography, MR venography, lymphoscintigraphy) may be needed to differentiate non-thrombotic obstruction from DVT and lymphedema. Ultrasound is still the first-line to rule out DVT.
8. Arteriovenous Fistula and Congenital Vascular Abnormalities
- Distinguishing Features from DVT: Arteriovenous fistula (abnormal connection between artery and vein) can cause localized swelling and warmth, sometimes with a palpable thrill or audible bruit. Congenital vascular malformations can present with chronic limb swelling, pain, and skin changes. These conditions are often long-standing and may have other associated features not typical of acute DVT. Vascular imaging (Duplex ultrasound, MR angiography, CT angiography) is needed for definitive diagnosis and differentiation from DVT.
9. Vasculitis
- Distinguishing Features from DVT: Vasculitis (inflammation of blood vessels) can, in rare cases, affect veins and mimic DVT. However, vasculitis is typically a systemic illness with other constitutional symptoms (fever, fatigue, weight loss) and signs of inflammation in other organs. Skin changes in vasculitis may include palpable purpura, ulcers, or nodules, distinct from DVT redness. DVT is usually a more localized venous event, while vasculitis is a systemic inflammatory process affecting multiple organ systems. Blood tests (inflammatory markers, specific vasculitis panels) and sometimes biopsy are needed to diagnose vasculitis. Ultrasound is still needed to rule out DVT as a concurrent or primary diagnosis.
By systematically considering these differential diagnoses and utilizing appropriate clinical assessment and diagnostic tools, particularly Duplex ultrasound, clinicians can accurately diagnose DVT and differentiate it from mimicking conditions, leading to timely and effective management.
Surgical Oncology and Thromboprophylaxis
Cancer patients have a heightened thromboembolism risk. Thromboprophylaxis is beneficial for cancer patients undergoing chemotherapy or surgery. Meta-analyses show thromboprophylaxis reduces VTE incidence in cancer patients without increasing significant bleeding. Current National Comprehensive Cancer Network (NCCN) guidelines recommend anticoagulation (unfractionated heparin or LMWH) for hospitalized cancer patients as thromboprophylaxis. Mechanical prophylaxis (compression devices) should be used in patients with active bleeding, thrombocytopenia (< 50,000/MCL), coagulopathy, or neuraxial catheters. Contraindications to mechanical prophylaxis include acute DVT and severe arterial insufficiency.
Extended-duration anticoagulation prophylaxis in hospitalized acutely ill cancer patients did not significantly lower VTE risk but increased bleeding risk. Post-operative VTE prophylaxis for surgical pelvic or abdominal oncology patients should continue for up to four weeks. Aspirin or anticoagulation is recommended for multiple myeloma patients on immunomodulatory medications based on IMPEDE VTE score risk stratification. Prophylactic anticoagulation with DOACs or LMWH for solid cancer patients on chemotherapy with high Khorana scores reduces pulmonary embolism incidence.
LMWH remains the preferred anticoagulant for cancer-associated thrombosis. Dosage is typically 1 mg/kg every 12 hours (or 1 mg/kg daily for creatinine clearance < 30 mL/minute; avoid in dialysis). DOACs (apixaban, rivaroxaban, edoxaban, fondaparinux, warfarin) are also treatment options. The Caravaggio trial showed apixaban non-inferior to LMWH for cancer-associated VTE without increased bleeding risk.
Thrombolytic therapy may be used for life- or limb-threatening pulmonary embolism or acute DVT, considering contraindications (intracranial tumors/metastasis, active bleeding, intracranial hemorrhage history). NCCN recommends treatment duration minimum of 3 months or for active malignancy duration. Indefinite anticoagulation is recommended for non-catheter-related DVT or pulmonary embolism.
Continuous benefit-risk assessment and complication monitoring are essential. Retrievable vena cava filters can prevent pulmonary embolism in patients with DVT in the inferior vena cava, iliac, femoral, and popliteal veins who have contraindications to therapeutic anticoagulation. Monitor for contraindication resolution and consider vena cava filter removal and therapeutic anticoagulation. Catheter-associated thrombosis treatment involves catheter removal or anticoagulation if the catheter remains.
Staging of Deep Vein Thrombosis
DVT severity is classified as:
- Provoked: Secondary to acquired risk factors (surgery, oral contraceptives, trauma, immobility, obesity, cancer).
- Unprovoked: Idiopathic or endogenous causes; higher recurrence risk if anticoagulation stopped.
- Proximal: Above the knee, femoral or iliofemoral veins; higher risk of pulmonary embolism.
- Distal: Below the knee.
Prognosis of Deep Vein Thrombosis
DVT prognosis includes:
- Many DVTs resolve without complications.
- Post-thrombotic syndrome occurs in approximately 43% of patients within 2 years post-DVT (30% mild, 10% moderate, 3% severe).
- High DVT recurrence risk (up to 25%).
- Mortality in approximately 6% of DVT cases and 12% of pulmonary embolism cases within one month of diagnosis.
- Early mortality associated with pulmonary embolism presentation, advanced age, cancer, and cardiovascular disease.
Complications of Deep Vein Thrombosis
Major DVT complications include:
- Pulmonary embolism (paradoxical emboli if atrial-septal defect present).
- Post-thrombotic syndrome.
- Bleeding from anticoagulation.
Postoperative and Rehabilitation Care for DVT
Thromboprophylaxis for hospitalized patients at DVT risk includes pharmacological and mechanical strategies. Pharmacological options: unfractionated and low-molecular-weight heparins, novel oral anticoagulants (NOACs – direct thrombin inhibitors like dabigatran, factor Xa inhibitors like rivaroxaban), aspirin, or warfarin. Network meta-analysis suggests NOACs are effective for VTE thromboprophylaxis and VTE-related mortality in extended treatment scenarios, with apixaban showing a favorable bleeding risk profile compared to other NOACs, warfarin, and aspirin.
Mechanical prophylaxis measures:
- Graduated compression stockings.
- Intermittent pneumatic compression devices.
- Venous foot pumps.
- Electrical stimulation devices.
Mechanical devices should be used in conjunction with pharmacological prophylaxis when appropriate.
Deterrence and Patient Education for DVT
Patient education should emphasize:
- Ambulation (mobility).
- Compression stocking use.
- Smoking cessation.
Enhancing Healthcare Team Outcomes in DVT Management
Effective DVT diagnosis and management require an interprofessional healthcare team (clinicians, specialists, nurses, physical therapists, vascular technicians, pharmacists) to prevent pulmonary embolism and reduce healthcare costs associated with prolonged hospitalization and treatment.
Prevention is key. Nurses and pharmacists are vital in patient DVT prophylaxis education. Nurses initiate prevention upon hospital admission, educating patients on ambulation, compression stockings, and anticoagulation medication adherence. Nurses also remind physicians about DVT prophylaxis in pre- and post-operative settings. Hospitals should have and enforce DVT prophylaxis and treatment guidelines.
Pharmacists should be knowledgeable about current anticoagulants, indications, and medication reconciliation. Pharmacists educate patients on treatment compliance and INR monitoring. Hematology nurses or pharmacists monitor INR and bleeding risk during anticoagulant therapy. Open communication among the interprofessional team is crucial for safe and effective DVT management.
Outcomes:
Pulmonary embolism causes nearly 300,000 deaths annually in the US. Despite guidelines and healthcare worker education, DVT prophylaxis is often underutilized. DVT is largely preventable, and healthcare workers must be vigilant. Post-thrombotic phlebitis is a common long-term sequela of DVT, highlighting the importance of interprofessional care coordination and communication for long-term patient management.
Review Questions
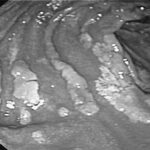
Figure
Deep Vein Thrombosis. This illustration compares normal blood flow with that of deep vein thrombosis and embolism within the deep veins of the leg. Contributed by M Schick, DO
Figure
Deep Vein Thrombosis. This illustration compares normal blood flow with that of deep vein thrombosis and embolism within the deep veins of the leg. (https://creativecommons.org/licenses/by-nd/2.0/deed.en)
References
[List of references from original article – kept as is]
Disclosure: Sheikh Waheed declares no relevant financial relationships with ineligible companies.
Disclosure: Pujitha Kudaravalli declares no relevant financial relationships with ineligible companies.
Disclosure: David Hotwagner declares no relevant financial relationships with ineligible companies.