Have you ever found yourself perplexed by the sudden onset of mental status changes in a patient, particularly when trying to discern if the cause is neurological or drug-related? Are you sometimes unsure about which historical details, physical examination findings, and laboratory results are most crucial in determining the underlying cause and guiding treatment? And have you ever felt uncertain about the best approach to manage acute agitation in the emergency department (ED)? If these questions resonate with you, the following case study and discussion will offer valuable insights.
CASE VIGNETTE
Mr. A, a 62-year-old man in disheveled condition, was brought to the ED by police at his wife’s request due to a month-long escalation of irritable and unsettling behavior. He reported visual hallucinations of small men walking through walls and inhabiting his living room, whom he believed were stealing his money and car keys. His medical history included type 2 diabetes mellitus, hypertension, and coronary artery disease. His wife, concerned about his increasing unreliability, had been managing his medication administration for several months. Both Mr. A and his wife stated that he had no prior psychiatric evaluations.
Upon the ED physician’s attempt to conduct a physical examination, Mr. A became acutely agitated, screaming loudly, yelling obscenities, and making threatening gestures. The physician, prioritizing safety, requested assistance from hospital security to ensure the well-being of himself, Mr. A, and other patients and staff in the ED. Establishing safety protocols became paramount, and orders for medication and physical restraints were considered. This scenario highlights the critical need for a differential diagnosis when confronted with acute agitation, even when the presenting behaviors, like yelling obscenities, may seem primarily behavioral.
Mr. A’s wife was interviewed separately. She recounted that her husband had been in his usual health until about three months prior, when he began exhibiting disorganization, frequently misplacing his wallet and car keys, and missing work appointments. At times, he appeared inattentive and excessively sleepy. He also developed clumsiness, bumping into furniture and experiencing several falls, though without head trauma or loss of consciousness. Over the past month, his visual hallucinations of small men stealing from him emerged. His irritability intensified, and his wife expressed concern about potential violence. He experienced vivid dreams and acted them out during sleep. Mrs. A confirmed consistent medication adherence, including metformin, lisinopril, and atorvastatin, with no recent changes. She reported minimal alcohol consumption (one beer weekly) and no nicotine or recreational drug use. She also noted a family history of similar behavioral changes, hallucinations, slow gait, and dementia in her father-in-law starting in his 70s.
After sedation, blood samples were collected for laboratory analysis. Complete blood count (CBC) and differential, electrolytes, liver function tests (LFTs), thyroid function tests (TFTs), vitamin B12 and folate levels, rapid plasma reagin (RPR) for syphilis, serum and urine toxicology screens, and urinalysis all returned within normal limits. Electrocardiogram (EKG) and chest x-ray were also normal. Vital signs showed mild tachycardia (heart rate 105–110 bpm). Several hours later, Mr. A was calmer and able to cooperate with a physical examination. Notable findings included general bradykinesia and a bilateral pill-rolling tremor, but no other focal neurological deficits. Mental status examination revealed no signs of depression or mania, but he reported well-formed visual hallucinations. He denied suicidal or homicidal ideation and lacked insight into his symptoms. His Mini-Mental State Examination (MMSE) score was 23 out of 30, with points lost on serial 7s, multistep directions, and figure copying.
Based on this information, a differential diagnosis for Mr. A’s altered mental status and behavior was formulated, and further evaluation was initiated.
DISCUSSION
Understanding Altered Mental Status
Altered mental status (AMS) is not a diagnosis in itself, but rather a clinical descriptor encompassing a broad spectrum of signs and symptoms. Its interpretation is highly context-dependent. AMS can manifest as “changes in consciousness, appearance, behavior, mood, affect, motor activity, or cognitive function.”
One way to conceptualize AMS is by categorizing its manifestations according to the components of a mental status examination. Behavioral signs, observable through direct observation, might include poor hygiene, neglect of personal appearance, comfort, or safety, or contextually inappropriate behavior, such as agitation and yelling obscenities in a secure environment. AMS can also involve alterations in mood or affect, ranging from elation in mania to fear in persecutory delusions, or flattened affect in schizophrenia. Motoric manifestations, such as abnormal postures, gestures, or changes in movement speed, can also indicate AMS.
Furthermore, AMS can involve cognitive impairment, including disorientation to person, place, or time. Attentional deficits, demonstrated by difficulty with tasks like serial 7s or reciting days of the week backward, are also indicative. Language disturbances, affecting fluency, semantics, reading, or writing, can be present. Memory impairment, such as difficulty recalling three words after a delay or recent events, is another feature. Executive function, planning, and visuospatial abilities may also be affected. Finally, AMS can encompass changes in thought content, such as hallucinations or delusions, or thought process. Given the diverse ways AMS can present through dysregulated affect, behavior, or cognition, clinicians must develop a broad differential diagnosis and clearly articulate the specific signs and symptoms observed.
Etiologies of Altered Mental Status
The causes of AMS are as varied as its presentations. Several frameworks can guide clinicians in systematically identifying these causes.
The differential diagnosis for AMS includes metabolic and medication-related etiologies, such as opioid, benzodiazepine, or steroid excess, and effects of other substances like alcohol, cocaine, or marijuana. Electrolyte imbalances, whether acute (e.g., hyponatremia in primary polydipsia) or secondary to underlying conditions (e.g., malignancy-related hyponatremia), can also precipitate AMS. Therefore, assessment of sodium, potassium, calcium, and magnesium levels is crucial. Endocrine disorders, such as hyperthyroidism or diabetic ketoacidosis, can also lead to AMS. Environmental factors, such as hypothermia, hyperthermia, or hypoxia (e.g., at high altitudes), can impact metabolic function and contribute to AMS. Vitamin deficiencies, such as niacin deficiency (pellagra, characterized by the “3 Ds”: diarrhea, dermatitis, and dementia) or thiamine deficiency (Wernicke encephalopathy), are also potential causes. Hepatic or uremic encephalopathy resulting from liver or renal dysfunction can present with a wide range of AMS symptoms.
Infections are another significant category of AMS causes. Sepsis, meningitis, brain abscesses, and systemic infections like urinary tract infections or pneumonia can induce changes in behavior and cognition, particularly in older adults where AMS may be misattributed to dementia. Noninfectious inflammatory, autoimmune, and neurodegenerative conditions should also be considered. Seizures, regardless of etiology (epilepsy, metabolic disturbances, drug withdrawal), can cause AMS in the ictal or postictal phases.
Primary neurological and psychiatric conditions are also important etiologies of AMS. Ischemic and hemorrhagic strokes, traumatic brain injury, and central nervous system (CNS) tumors or paraneoplastic syndromes must be considered. Finally, a range of primary psychiatric disorders, including mood disorders (bipolar I and II, major depressive disorder), psychotic disorders (schizophrenia, schizophreniform disorder, brief psychotic disorder, delusional disorder), dementias (Alzheimer’s, vascular dementia, neurodegenerative dementias like Parkinson’s disease and diffuse Lewy body disease [DLBD]), and catatonia (hyperactive or hypoactive), should be included in the differential.
Given the wide range of potential causes, some rapidly progressive and life-threatening, a systematic and timely approach to differential diagnosis is essential.
Historical Factors in Differential Diagnosis
Agitation and altered mental status can stem from various underlying causes, including substance intoxication or withdrawal (prescribed or illicit), psychiatric illness, and medical illness. Key aspects of the presentation, such as the timeline, psychiatric and medical history, associated symptoms, and family history, help refine the differential diagnosis. Patients may have multiple contributing conditions, necessitating a broad differential. When patient history is unreliable, collateral information from family, friends, or healthcare providers is vital. Family interviews should ideally occur separate from the patient to encourage open communication.
The timeline of symptom onset and progression is critical. Acute onset (hours to days) suggests acute medical events (stroke, substance intoxication/withdrawal), while acute onset with fluctuating course points to delirium. Subacute onset (days to weeks) suggests gradual development (mania, psychotic decompensation in schizophrenia). Chronic course (months) suggests longer-term processes like dementia (Alzheimer’s, DLBD, frontotemporal dementia). Stepwise chronic course is suggestive of vascular dementia. Acute-on-chronic course (pre-existing impairment worsening acutely) suggests superimposed conditions, such as delirium on dementia.
Medical and psychiatric history provides crucial clues. Medical conditions associated with AMS (endocrinopathies, hypoxia from pulmonary disease, severe hypertension) raise suspicion for delirium. Psychiatric history (schizophrenia, bipolar disorder, dementia) suggests psychiatric etiology. Substance use disorder history points to intoxication or withdrawal. Medication review is essential, as narrow therapeutic index medications can cause toxicity with minor dose changes or fluctuations in blood levels. Overdose or abrupt discontinuation can also cause agitation and AMS. Patient age is also relevant; new mood or psychotic disorders become less likely with age, while dementia risk increases.
Co-occurring symptoms further narrow the differential. Agitation with waxing and waning mental status, diurnal fluctuations, inattention, and impaired consciousness strongly suggests delirium. Agitation with decreased sleep need, pressured speech, hypersexuality, impulsivity, and euphoria suggests bipolar disorder. Specific symptom clusters suggest toxidromes (e.g., anticholinergic toxicity with mydriasis, dry skin, urinary retention, hyperthermia, tachycardia, hypertension). Agitation with memory changes or executive dysfunction raises concern for dementia.
Social and occupational history helps assess premorbid cognitive function, intelligence, education level (influencing mental status exam interpretation), and environmental risk factors. Family history can indicate genetic predisposition to dementias, mood disorders, and schizophrenia.
In Mr. A’s case, subacute onset (months, not hours/days) makes delirium less likely. Absence of psychiatric and family psychiatric history makes mood or psychotic disorders less probable. Medications and alcohol use are unlikely contributors. However, age, family history, and time course increase likelihood of dementia.
Physical Examination in Altered Mental Status
Physical examination in AMS must be systematic and comprehensive, even when psychiatric cause is suspected, to rule out contributing or causative medical factors.
Complete vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation) are crucial, as abnormalities can suggest underlying illness. The physical exam should focus on associated signs and symptoms indicative of specific diagnoses. For example, Argyll-Robertson pupils suggest neurosyphilis; ataxia and ophthalmoplegia suggest Wernicke-Korsakoff syndrome. Physical findings can also indicate toxidromes (e.g., anticholinergic toxicity with dry skin and mydriasis in acute AMS).
Neurological examination is critical, including cranial nerves, sensory and motor function, deep tendon reflexes, cerebellar function, and gait. Focal findings suggest specific etiologies like stroke or Parkinson’s disease. Screening for visual or hearing impairment is important, as sensory deficits can exacerbate cognitive and behavioral changes. In Mr. A, physical examination revealed parkinsonian symptoms (bradykinesia and tremor) without other focal neurologic deficits.
Laboratory and Diagnostic Testing
Laboratory testing for AMS should be broad, addressing reversible causes including vascular (stroke), infectious (neurosyphilis), neoplastic (primary, metastatic, paraneoplastic), degenerative (multiple sclerosis), inflammatory (vasculitis), endocrine (hyperthyroidism/hypothyroidism), metabolic (thiamine deficiency), toxic (medication effects), traumatic (dementia pugilistica), and other (normal pressure hydrocephalus) etiologies. Minimum testing includes CBC with differential, chemistry panel (calcium, magnesium, phosphorus, glucose), LFTs, TFTs, B12 and folate levels, RPR, relevant drug levels (digoxin, lithium, alcohol), urine drug screen, and urinalysis. EKG and chest x-ray are also recommended. CT or MRI brain scan should be obtained, with MRI preferred unless intracranial hemorrhage is suspected. Further testing is needed if initial workup is inconclusive or atypical symptoms are present. Lumbar puncture for CSF analysis is indicated for suspected CNS infection or autoimmune encephalitis. EEG can diagnose seizure disorder, Creutzfeldt-Jacob disease, or confirm delirium. In Mr. A’s case, initial normal labs prompted further diagnostic testing.
Life-Threatening Causes of Altered Mental Status
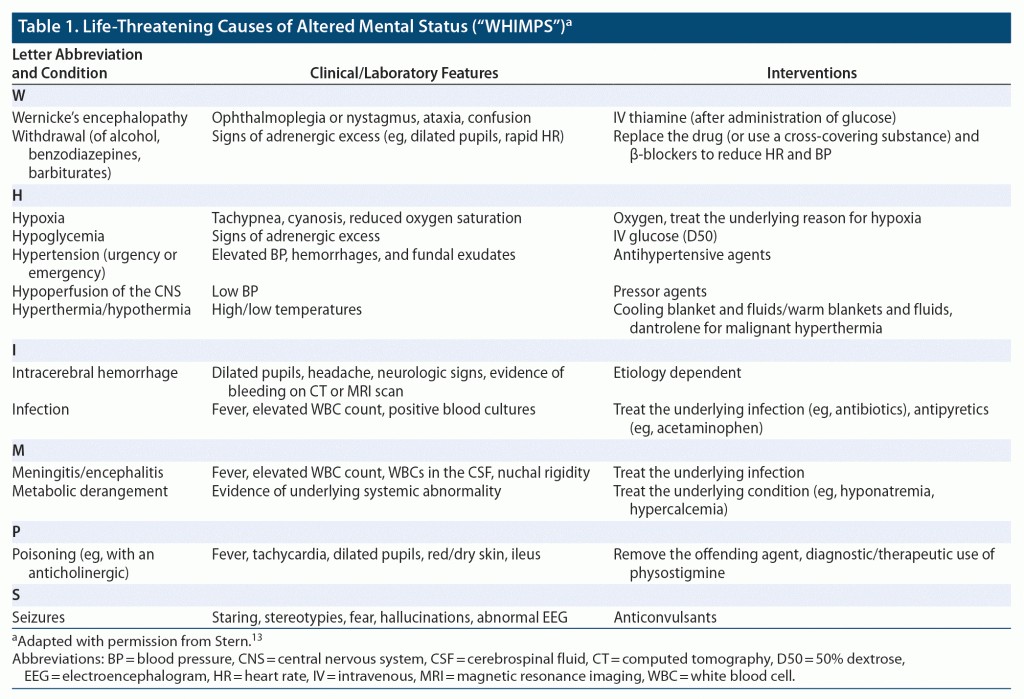
While any illness or physiological stress can contribute to AMS, some conditions are rapidly progressive and potentially lethal if undiagnosed and untreated. The mnemonic “rule out the WHIMPS” aids in recalling these critical conditions: Wernicke encephalopathy, Hypoglycemia, Hypoxia, Hyponatremia, Hemorrhage (intracranial), Infection (meningitis, encephalitis, sepsis), Meningitis, Poisoning/Overdose, Status epilepticus. Early recognition and intervention for these conditions can be life-saving.
Table 1: Life-Threatening Causes of Altered Mental Status: The “WHIMPS” Mnemonic.
Conditions Associated with Visual Hallucinations
Hallucinations, perceptions without external stimuli, can involve any of the five senses and arise from dysfunction in various organ systems (CNS, cardiopulmonary, endocrine, hematologic) and psychiatric, medical, metabolic, and ophthalmic disorders, as well as substance use or withdrawal. While auditory hallucinations are more commonly associated with primary psychiatric disorders (e.g., schizophrenia), visual hallucinations are also frequent. Neurological etiologies are more likely to cause visual hallucinations than other types. Migraine sufferers may experience visual hallucinations (aura) preceding headache. Charles Bonnet syndrome, resulting from visual system damage (e.g., macular degeneration) or deafferentation of visual cortex, is characterized by visual hallucinations. Sleep disturbances (insomnia, narcolepsy) can lead to hypnagogic (sleep onset) or hypnopompic (upon waking) visual hallucinations.
Table 2: Differential Diagnosis of Hallucinations.
Psychotic symptoms occur in 15%–78% of major neurocognitive disorders, often correlated with dementia etiology. Notably, visual hallucinations are early and prominent in DLBD, occurring in up to 80% of patients, helping differentiate it from Parkinson’s disease and Alzheimer’s disease, where visual hallucinations are less common.
Understanding Paranoia
Paranoia, characterized by extreme suspiciousness and mistrust, can escalate to delusions of persecution, jealousy, or harm. Paranoia exists across a spectrum of severity; mild paranoia is common under stress. However, severe, persistent paranoia with irrational thoughts and potentially dangerous actions requires clinical attention and patient and others’ protection. Risk factors for paranoia include biological (medical/neurological disorders, medication side effects, family history), sociocultural (race/ethnicity, social support), environmental (migration, toxins), and clinical (primary psychiatric etiologies) factors.
Table 3: Differential Diagnosis of Paranoia.
Severe, persistent paranoia is a core feature of primary psychiatric disorders, including psychotic and mood disorders. Comprehensive psychiatric evaluation is needed to determine etiology. Paranoid delusions often co-occur with other psychotic symptoms (disorganized speech, hallucinations) in schizophrenia. Persecutory delusional disorder may present without other psychotic symptoms or functional impairment. Genetic predisposition and childhood adversity are risk factors for paranoid personality disorder; early recognition can guide prevention and intervention.
Psychotic symptoms, including paranoia, can arise in diverse neuropsychiatric and medical conditions. Non-psychiatric paranoia may exhibit atypical features (cognitive fluctuations), abnormal vital signs, or lab results. Illicit drug use is the most common cause of secondary paranoia, particularly in young adults; new-onset paranoia can also be due to drug withdrawal. Elderly individuals are at higher risk for secondary psychosis/paranoia due to drugs, toxins, polypharmacy, and medical illnesses.
Treatments for Hallucinations and Paranoia
While treatment for hallucinations and paranoia targets the underlying etiology, symptomatic treatment may be needed immediately, even before diagnosis. Safety measures are paramount for patients with command hallucinations or intense persecutory delusions causing agitation. Immediate interventions ensure patient and staff safety. Physical or chemical restraints may be necessary. Parenteral haloperidol (with or without lorazepam), intramuscular (IM) olanzapine, and parenteral droperidol are reasonable options. However, the FDA issued a warning in 2005 regarding combined IM olanzapine and benzodiazepines due to potential excessive sedation and cardiorespiratory depression, following reports of adverse events including fatalities. Despite this, data supporting a clear cause-and-effect relationship are inconsistent, and co-administration has been reported as safe in some studies.
Once safety is assured, psychopharmacologic or neurotherapeutic agents can manage hallucinations/paranoia. Second-generation antipsychotics (SGAs) (olanzapine, risperidone, quetiapine) or first-generation antipsychotics (FGAs) (haloperidol, fluphenazine) can control psychotic symptoms. While evidence favoring one over another for agitation, hallucinations, or paranoia is limited, SGAs are increasingly recommended for better tolerability. Orally disintegrating antipsychotic formulations (risperidone, olanzapine) improve medication adherence. Agent choice depends on patient history, clinician preference, or hospital protocol. Benzodiazepine (lorazepam) or mood stabilizer (sodium valproate) augmentation may be needed for stabilization. Parenteral antipsychotics or benzodiazepines should be considered for uncooperative patients or when rapid onset is needed. Clozapine is reserved for treatment-resistant hallucinations and paranoia, requiring further evaluation and monitoring. Electroconvulsive therapy (ECT) can be highly effective in acutely controlling hallucinations and paranoia in the ED.
Adverse Effects of Antipsychotics
While antipsychotics are crucial for managing acute agitation and aggression unresponsive to non-pharmacological approaches, clinicians must be aware of potential side effects and their management. Safety and efficacy vary based on patient factors (age, medical/pharmacologic history, presentation – e.g., alcohol intoxication), antipsychotic agent (mechanism of action differences), dosage, and administration route. FGAs (haloperidol, droperidol) and SGAs (olanzapine) are commonly used for ED agitation.
Common short-term side effects include excessive sedation, somnolence, hypotension, dizziness, increasing fall risk (especially in elderly). Ziprasidone is associated with higher rates of somnolence (20%) and nausea (12%). Acute involuntary movement disorders (akathisia, acute dystonia) are more common with FGAs; co-administration of FGAs with benzodiazepines, benztropine, or diphenhydramine can reduce EPS risk. However, EPS (parkinsonism) can occur with SGAs (olanzapine), especially with repeated doses. QT interval prolongation is more frequent with ziprasidone and haloperidol, less so with olanzapine; Torsades de pointes is rare, primarily with IV haloperidol. Both are more likely in patients with pre-existing cardiac rhythm abnormalities and with drugs affecting P450 metabolism.
Airway compromise or respiratory complications with antipsychotics are rare but more likely with SGAs in alcohol-intoxicated patients. The FDA advises against co-administration of antipsychotics and benzodiazepines due to increased risk of sedation and cardiopulmonary depression. Ziprasidone should be avoided in women of childbearing age due to potential teratogenicity.
Potential side effects emphasize the need for thoughtful antipsychotic selection based on patient presentation and urgency, even when medical history is limited. ED clinicians should choose antipsychotics based on desired outcomes, continuously monitoring for side effects and intervening promptly if needed. The lowest effective antipsychotic dose should be used for the shortest duration needed for clinical efficacy and safe sedation, rather than anticipating long-term treatment, to minimize adverse effects.
Post-Emergency Department Treatment Settings
Disposition from the ED is as critical as acute ED management. Appropriate level of care depends on clinical presentation severity, etiology, ease of identification and reversal, patient baseline, recurrence likelihood, aftercare planning, support, and medical knowledge for safe management. A recent study showed patients with AMS presenting to the ED have significantly higher mortality risk within 7 and 30 days compared to patients with chest pain or headache. Most AMS patients require inpatient hospitalization for monitoring and management of hemodynamics, airway, incapacity, and medical/psychiatric problems. Given high mortality risk, AMS manifestations should be taken seriously, etiology investigated, and hospitalization threshold should be low.
Patients with AMS in the ED may become frustrated, especially with prolonged ED boarding, and request to leave against medical advice. This poses safety risks and presents ethical dilemmas regarding patient autonomy versus decision-making capacity. Rigorous capacity assessment and involvement of family/friends to advocate for hospitalization are important. Shared decision-making, empathic listening, and addressing patient concerns (pet care, childcare, work) are crucial. Informing patients about the process and potential time needed can improve adherence to care recommendations.
However, not all AMS patients require hospitalization. Safe discharge home or to primary residence is possible for those with resolved AMS and identified, reversed underlying cause, with reliable caregivers, accessible transportation, and ability to follow aftercare plans. Regardless of disposition, timely and effective communication between ED staff and inpatient/outpatient providers is vital for care coordination and patient safety.
Mr. A’s Outcome
Mr. A was admitted to neurology for further evaluation. EEG showed decreased background reactivity and frontal intermittent rhythmic delta activity. MRI revealed mild diffuse frontal and parieto-temporal volume loss, substantia nigra pallor, and preserved mesial temporal lobe/hippocampal volume. He was diagnosed with DLBD and started on rivastigmine and low-dose quetiapine, which reduced agitation. He was discharged home with his wife one week later, with close psychiatry and neurology follow-up.
Diffuse Lewy Body Disease Presentation and Course
Diffuse Lewy body disease (dementia with Lewy bodies) is a common dementia cause in the elderly. Pathophysiology involves Lewy body protein deposits in cortex, amygdala, and brainstem. Clinical features overlap with Alzheimer’s disease but commonly include visual hallucinations, fluctuating course, antipsychotic sensitivity, executive dysfunction, apathy, irritability, visuospatial and memory impairment, REM sleep behavior disorder, and agitation. No FDA-approved treatments exist, and average disease course is 5–7 years (variable).
CONCLUSION
Altered mental status, manifesting as disturbances in affect, behavior, and cognition, is prevalent and problematic, signaling potential life-threatening emergencies and reflecting dysfunction across organ systems – medical, neurological, or psychiatric. Diligent, comprehensive investigation of AMS cause is paramount, as treatment is etiology-dependent. While diagnosing, symptomatic interventions are crucial for patient, family, and staff safety. Awareness of pharmacologic treatment side effects guides agent choice, as do AMS etiology, severity, medication response (antipsychotics, benzodiazepines, mood stabilizers), and administration routes.
Submitted: March 3, 2021; accepted April 29, 2022. Published online: December 8, 2022. Relevant financial relationships: Dr Vyas has received research salary support from Nestlé Purina PetCare Company. Drs Donovan, Paudel, Van Alphen, and Stern and Mr Petriceks report no relevant financial relationships. Funding/support: None.
Clinical Points
- Altered mental status (AMS) is a clinical term describing a wide range of signs and symptoms, not a diagnosis itself.
- AMS can be caused by abnormalities in any organ system and can be medical, neurological, or psychiatric in origin.
- Treatment choice for AMS depends on etiology, severity, medication response (antipsychotics, benzodiazepines, mood stabilizers), and available administration routes.
- Timely and effective communication between ED staff and inpatient/outpatient providers is crucial for coordinated care and patient safety.