Introduction
Dyspnea, commonly known as shortness of breath, is a prevalent symptom affecting a significant portion of patients in ambulatory care, with estimates reaching as high as 25%. This distressing sensation can stem from a diverse range of underlying medical conditions, some of which pose an immediate threat to life. Prompt and accurate diagnosis is therefore crucial in managing dyspnea to mitigate mortality and morbidity. The diagnostic process can be complex, especially when clinical presentations overlap, or when patients have multiple co-existing diseases, such as the common combination of congestive heart failure and chronic obstructive pulmonary disease (COPD). Adding to the challenge, dyspnea is a subjective experience, encompassing a variety of sensations, making its evaluation a nuanced clinical undertaking. The presence of dyspnea itself is a recognized indicator of increased mortality, underscoring the importance of effective diagnostic strategies.
This article aims to provide a comprehensive overview of the differential diagnosis of dyspnea, focusing on the key steps in evaluation and the broad spectrum of potential underlying causes. It is designed to equip clinicians with the knowledge to approach dyspnea systematically, ensuring timely and accurate diagnoses.
Understanding Dyspnea: Definition and Pathophysiology
The American Thoracic Society defines dyspnea as “a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity.” This definition highlights the multifaceted nature of dyspnea, influenced by physiological, psychological, social, and environmental factors. Patients may describe dyspnea in various ways, including effortful breathing, a sensation of choking or suffocation, or an intense need for air. This subjective variability poses a diagnostic challenge, requiring clinicians to carefully interpret patient descriptions in the context of clinical findings.
The precise mechanisms behind dyspnea are still under investigation, but current theories center on a complex regulatory circuit. This circuit involves afferent signals transmitted centrally from chemoreceptors (sensitive to pH, CO2, and O2 levels) and mechanoreceptors in muscles and lungs (including C fibers in the parenchyma and J fibers in bronchi and pulmonary vessels). These signals trigger a corresponding ventilatory response, which, when perceived as uncomfortable or labored, results in the sensation of dyspnea.
To quantify and communicate the severity of dyspnea, various assessment tools are employed. These range from simple scales like the visual analog scale and Borg scale, which measure intensity, to more comprehensive multidimensional questionnaires such as the Multidimensional Dyspnea Profile. Disease-specific classifications, such as the New York Heart Association (NYHA) classification for chronic congestive heart failure, also play a role in assessing dyspnea in specific patient populations.
Epidemiology of Dyspnea
Dyspnea is a common complaint across various healthcare settings, from primary care to emergency departments. Studies indicate that approximately 7.4% of emergency room visits are due to dyspnea. In general practice, dyspnea is reported by 10% of patients during normal activities like walking on level ground, and this number rises to 25% with more strenuous activities such as climbing stairs. For a notable 1–4% of patients, dyspnea is the primary reason for seeking medical consultation.
In specialized medical practices, dyspnea is a frequent concern, affecting 15–50% of cardiology patients and nearly 60% of pulmonology patients. Emergency medical services also frequently encounter dyspnea, accounting for 12% of calls, with about half of these patients requiring hospitalization. Among those hospitalized for dyspnea, in-hospital mortality is approximately 10%, highlighting the serious nature of this symptom. The distribution of underlying causes of dyspnea varies significantly depending on the healthcare setting, as detailed in Table 1.
Diagnostic Evaluation of Dyspnea
The diagnostic evaluation of dyspnea is often challenging due to its subjective nature and diverse etiology. A systematic approach is essential to effectively narrow down the differential diagnoses and guide appropriate management.
Initial Assessment: History and Physical Examination
The initial step in evaluating dyspnea involves a thorough patient history and physical examination. Gathering detailed information about the onset, duration, and progression of dyspnea is crucial. Clinicians should inquire about factors that trigger or alleviate symptoms, such as exertion, body position, and environmental exposures. Understanding the temporal pattern of dyspnea – whether it is acute, chronic, intermittent, or episodic – provides valuable diagnostic clues.
Table 1: Common Causes of Dyspnea Across Different Healthcare Settings
| Healthcare Setting | Common Causes |
|---|---|
| Emergency Medical Services | Heart Failure (15–16%), Pneumonia (10–18%), COPD (13%), Bronchial Asthma (5–6%) |
| Emergency Room | COPD (16.5%), Heart Failure (16.1%), Pneumonia (8.8%), Myocardial Infarction (5.3%) |
| General Practice | Acute Bronchitis (24.7%), Acute Upper Respiratory Infection (9.7%), Other Airway Infections (6.5%) |
Adapted from modified data from [6, 8, e3]
The patient’s medical history, including pre-existing conditions, medications, smoking history, and occupational exposures, should be carefully reviewed. Associated symptoms, such as cough, chest pain, wheezing, edema, and palpitations, can further refine the differential diagnosis. A detailed physical examination should include assessment of vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation), auscultation of the lungs and heart, and examination for signs of respiratory distress (e.g., use of accessory muscles, cyanosis) and fluid overload (e.g., peripheral edema, jugular venous distention). Table 2 outlines symptoms and signs accompanying dyspnea that can be particularly informative for differential diagnosis.
Acute Dyspnea: Rapid Evaluation and Management
Acute dyspnea, characterized by a sudden onset of shortness of breath, often indicates a potentially life-threatening condition requiring immediate evaluation and intervention. Alarm symptoms include confusion, new-onset cyanosis, dyspnea severe enough to impair speech, and signs of respiratory exhaustion. In such cases, rapid assessment of vital signs, particularly respiratory rate, heart rate, blood pressure, and oxygen saturation, is paramount. An elevated respiratory rate is a strong predictor of adverse outcomes and the need for intensive care.
Table 2: Symptoms and Signs Accompanying Dyspnea and Differential Diagnostic Considerations
| Additional Symptoms and Signs | Differential Diagnostic Considerations |
|---|---|
| Bradycardia | SA or AV block, drug overdose (heart rate slowing agents) |
| Brainstem signs, neurological deficits | Brain tumor, cerebral hemorrhage, cerebral vasculitis, encephalitis |
| Cough | Non-specific; airway and lung parenchyma diseases |
| Cyanosis | Acute respiratory failure, congenital heart defect with right-to-left shunt, Eisenmenger syndrome (chronic) |
| Diminished or absent breathing sounds | COPD, severe asthma, pneumothorax (tension), pleural effusion, hemothorax |
| Distended neck veins with lung rales | Acutely decompensated congestive heart failure, acute respiratory failure |
| Distended neck veins, normal lung sounds | Pericardial tamponade, acute pulmonary embolism |
| Dizziness, syncope | Valvular heart disease (aortic stenosis), cardiomyopathy (hypertrophic, dilated), anemia, anxiety, hyperventilation |
| Exhaustion, generalized weakness, exercise intolerance | Anemia, collagenoses, malignancy (lung cancer), neuromuscular disease |
| Fever | Pulmonary infection (pneumonia, acute bronchitis), exogenous allergic alveolitis, thyrotoxicosis |
| Heart murmur | Cardiac valvular disease |
| Hemodynamic dysfunction (hypertensive) | Hypertensive crisis, panic attack, acute coronary syndrome |
| Hemodynamic dysfunction (hypotensive) | Forward heart failure, metabolic disturbance, sepsis, pulmonary embolism |
| Hemoptysis | Lung cancer, pulmonary embolism, bronchiectasis, chronic bronchitis, tuberculosis |
| Hepatojugular reflux | Acutely decompensated congestive heart failure |
| Hoarseness | Glottis or trachea disease, recurrent laryngeal nerve palsy |
| Hyperventilation | Acidosis, sepsis, salicylate poisoning, psychogenic (anxiety) |
| Impaired consciousness | Psychogenic hyperventilation, brain disease, metabolic disturbance, pneumonia |
| Orthopnea | Acute congestive heart failure, toxic pulmonary edema |
| Pain on respiration | Pneumothorax, pleuritis/pleuropneumonia, pulmonary embolism |
| Pain independent of respiration | Myocardial infarction, aortic aneurysm, Roemheld syndrome, renal or biliary colic, acute gastritis |
| Pallor | Marked anemia |
| Paradoxical pulse | Right-heart failure, pulmonary embolism, cardiogenic shock, pericardial tamponade, asthma exacerbation |
| Peripheral edema | Congestive heart failure |
| Platypnea | Hepatopulmonary syndrome, intrapulmonary shunting |
| Rales | Pneumonia, acutely decompensated congestive heart failure, acute respiratory failure |
| Stridor (inspiratory) | Croup, foreign body, bacterial tracheitis |
| Stridor (expiratory/combined) | Foreign body, epiglottitis, angioedema |
| Urticaria | Angioedema |
| Use of auxiliary muscles of respiration | Acute respiratory failure, severe COPD, severe asthma |
| Vegetative symptoms (trembling, cold sweat) | Respiratory failure, anxiety disorder, acute myocardial infarction |
| Wheezes | Asthma exacerbation, COPD, acutely decompensated congestive heart failure, foreign body |
Modified from [3, e4–e6]
Initial diagnostic steps often include an electrocardiogram (ECG) to rule out acute myocardial infarction or arrhythmias and a chest X-ray to identify pulmonary congestion, pneumothorax, or pneumonia. Biomarkers, particularly natriuretic peptides and troponins, play a crucial role in the differential diagnosis of acute dyspnea, as discussed in detail below. It’s also important to consider and address emotional factors such as panic and anxiety, which can exacerbate dyspnea symptoms.
Chronic Dyspnea: Systematic Diagnostic Approach
Chronic dyspnea, defined as dyspnea lasting for more than four weeks, is commonly attributed to a limited set of conditions, including bronchial asthma, COPD, congestive heart failure, interstitial lung disease, and mental disorders. However, in older, multimorbid patients, identifying a single cause can be challenging. A systematic diagnostic approach is essential, often starting with basic investigations and progressing to more specialized tests as needed.
The diagnostic process for chronic dyspnea begins with a detailed history and physical examination, similar to acute dyspnea evaluation, but with a focus on the long-term symptom trajectory and potential chronic underlying conditions. Observation of the patient’s breathing pattern can provide valuable clues; for instance, rapid, shallow breathing may suggest interstitial lung disease, while deep, slow breathing is more typical of COPD. Auscultation findings such as wheezes, crackles (rales), or diminished breath sounds further guide the differential diagnosis.
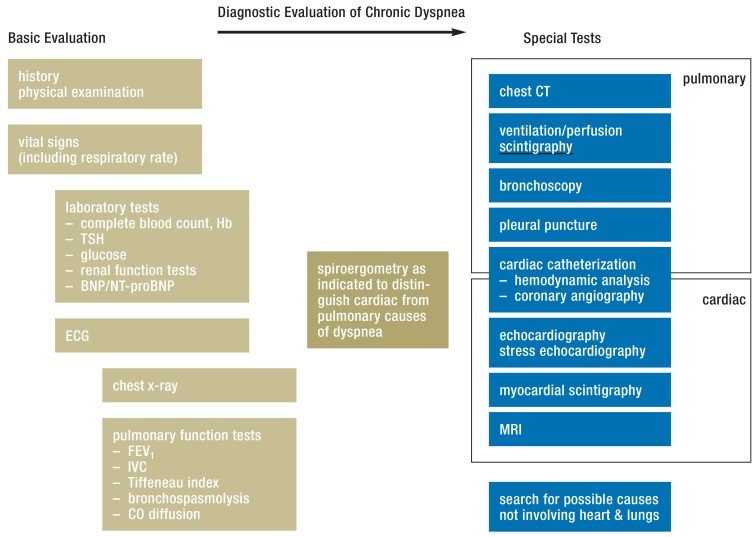
Initial investigations in chronic dyspnea often include basic laboratory tests (complete blood count, thyroid function tests, and potentially D-dimer if pulmonary embolism is considered), an ECG, and spirometry to assess pulmonary function. Depending on the suspected etiology, further tests may include echocardiography, chest computed tomography (CT), or invasive hemodynamic assessments. Figure 1 outlines a diagnostic algorithm for chronic dyspnea, emphasizing a step-wise approach based on initial findings. Spiroergometry (cardiopulmonary exercise testing) can be particularly useful in differentiating between cardiac and pulmonary limitations in patients with unexplained chronic dyspnea.
Figure 1: Diagnostic Evaluation of Chronic Dyspnea. Modified from [3, 9, 22, 24]. BNP: brain natriuretic peptide; CT: computed tomography; ECG: electrocardiography; FEV1: forced expiratory volume in 1 second; Hb: Hemoglobin; IVC: inspiratory vital capacity; MRI: magnetic resonance imaging; NT-proBNP: N-terminal prohormone brain natriuretic peptide; TSH: thyroid-stimulating hormone.
The Role of Biomarkers in Dyspnea Diagnosis
Biomarkers have become increasingly important in the differential diagnosis of dyspnea, particularly in acute settings. Natriuretic peptides, cardiac troponins, and D-dimers are among the most valuable biomarkers in this context.
Natriuretic Peptides (BNP, NT-proBNP)
Brain natriuretic peptide (BNP) and its N-terminal prohormone (NT-proBNP) are essential biomarkers for excluding acute congestive heart failure as a cause of dyspnea. Elevated levels of BNP or NT-proBNP strongly suggest cardiac dysfunction. Guidelines from the European Society of Cardiology (ESC) recommend specific cut-off values for BNP and NT-proBNP to rule out heart failure in patients presenting with dyspnea. However, it is important to note that these thresholds may be lower for patients with known chronic heart failure.
Cardiac Troponins
When acute coronary syndrome is suspected as the cause of dyspnea, cardiac troponins (troponin I or T) are critical. Serial measurements of troponin levels can effectively rule out acute myocardial ischemia. The threshold for a positive troponin test varies depending on the assay used, but elevated troponin levels indicate myocardial injury, which could be due to acute coronary syndrome or other cardiac or non-cardiac conditions.
D-dimers
D-dimers, fibrin degradation products, are elevated in thrombotic conditions. In the context of dyspnea, D-dimer testing is primarily used to rule out pulmonary embolism. D-dimers have a high negative predictive value for pulmonary embolism, meaning a normal D-dimer level in a patient with low or intermediate clinical probability of pulmonary embolism effectively excludes this diagnosis. Clinical probability assessment tools, such as the Wells score (eTable 3 in original article), are used to stratify patients before D-dimer testing. Age-adjusted D-dimer thresholds can improve test specificity in older patients without compromising sensitivity. Elevated D-dimer levels, especially in patients with high clinical suspicion, warrant further investigation with imaging studies to confirm or exclude pulmonary embolism.
It is important to recognize that both cardiac troponins and natriuretic peptides can be elevated in conditions other than acute coronary syndrome and heart failure, respectively. For example, pulmonary embolism causing right heart strain can also lead to elevated troponins and natriuretic peptides. Therefore, biomarker results should always be interpreted in conjunction with the clinical context and other diagnostic findings.
Differential Diagnosis of Dyspnea: Key Considerations
The differential diagnosis of dyspnea is broad, encompassing diseases of the respiratory, cardiovascular, and other organ systems. Categorizing potential causes by organ system helps to organize the diagnostic approach.
Respiratory System Diseases
Respiratory diseases are among the most common causes of dyspnea.
Bronchial Asthma
Bronchial asthma is characterized by chronic airway inflammation leading to variable airflow obstruction. Patients typically experience recurrent episodes of dyspnea, often nocturnal, accompanied by wheezing and cough. Triggers can include allergens, respiratory irritants, exercise, and infections. Spirometry reveals reversible airflow obstruction, which improves significantly after bronchodilator administration. Acute asthma exacerbations are marked by increased dyspnea, tachypnea, and prominent wheezing.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive disease characterized by persistent airflow limitation, usually associated with chronic bronchitis and emphysema. It is predominantly caused by smoking. Patients with COPD typically present with chronic dyspnea, cough, and sputum production. Pulmonary function testing shows irreversible airflow obstruction (low FEV1/IVC ratio), and chest imaging may reveal hyperinflation and emphysematous changes. COPD exacerbations lead to worsening dyspnea and may require hospitalization.
Pneumonia
Pneumonia, particularly in older adults, commonly presents with dyspnea as a primary symptom. Accompanying symptoms often include fever, cough, and pleuritic chest pain. Physical examination may reveal tachypnea and rales (crackles) on lung auscultation. Chest X-ray is essential for diagnosis, and severity assessment tools like the CRB-65 score help guide management decisions.
Interstitial Lung Diseases
Interstitial lung diseases (ILDs) comprise a heterogeneous group of disorders affecting the lung parenchyma. Patients typically report chronic, progressive dyspnea and dry cough. Physical examination may reveal fine inspiratory crackles (rales) and, in some cases, digital clubbing. Pulmonary function tests show restrictive ventilatory defects and reduced diffusing capacity for carbon monoxide (DLCO). High-resolution CT scanning and sometimes lung biopsy are needed for specific ILD diagnosis.
Pulmonary Embolism
Pulmonary embolism (PE) often presents with acute onset of dyspnea, sometimes accompanied by pleuritic chest pain and hemoptysis. Tachycardia and tachypnea are common examination findings. Risk factors for venous thromboembolism, such as recent surgery, immobilization, and malignancy, should be assessed. Clinical probability scores (e.g., Wells score), D-dimer testing, and CT pulmonary angiography are key diagnostic tools.
Cardiovascular System Diseases
Cardiovascular diseases are another major category in the differential diagnosis of dyspnea.
Congestive Heart Failure
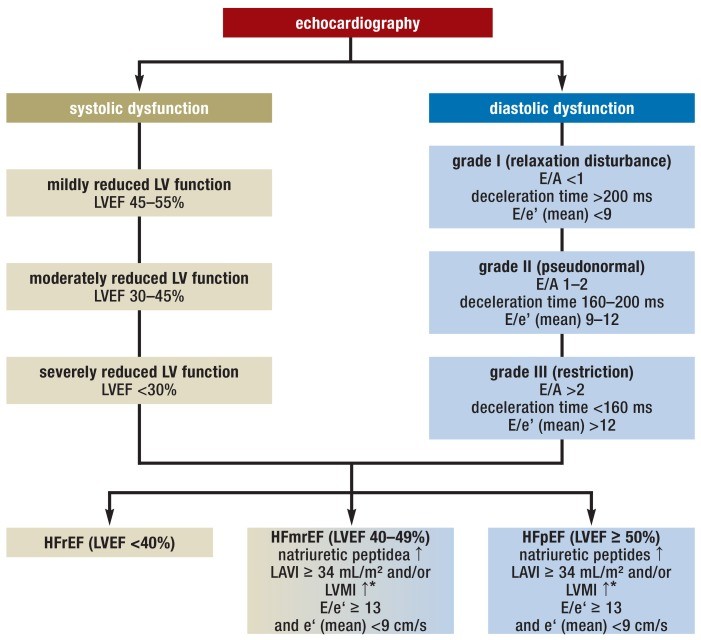
Congestive heart failure (CHF) is a common cause of both acute and chronic dyspnea. Patients with CHF may also experience fatigue, exercise intolerance, and fluid retention (edema). Dyspnea in CHF can be due to heart failure with reduced ejection fraction (HFrEF) or heart failure with preserved ejection fraction (HFpEF). Echocardiography is the primary diagnostic modality, assessing left ventricular function and structure. Natriuretic peptides (BNP, NT-proBNP) are valuable biomarkers in diagnosing and risk-stratifying CHF.
Figure 2: Echocardiographic Criteria for Congestive Heart Failure with Reduced (HFrEF) or Preserved (HFpEF) Ejection Fraction and Heart Failure with Mid-Range Ejection Fraction (HFmrEF). Modified from [17, 38]. LV: left ventricular; LVEF: left ventricular ejection fraction; LAVI: left atrial volume index; LVMI: left ventricular mass index; E: maximal speed of E-wave; A: maximal speed of A-wave; e’(mean): mean maximal (early) diastolic speed.
Coronary Heart Disease
Coronary heart disease (CHD) can manifest as dyspnea, particularly exertional dyspnea, even in the absence of typical angina. Dyspnea may be the predominant symptom, especially in patients with diabetes. Evaluation for CHD should be considered in patients with unexplained dyspnea, especially those with risk factors for atherosclerosis. Stress testing, including exercise ECG, stress echocardiography, or myocardial perfusion imaging, can help diagnose myocardial ischemia. Cardiac catheterization may be indicated for definitive diagnosis and intervention.
Valvular Heart Disease
Valvular heart diseases, such as aortic stenosis and mitral regurgitation, are important causes of dyspnea, especially in older adults. Aortic stenosis may present with exertional dyspnea, syncope, and angina. Mitral regurgitation often leads to dyspnea due to heart failure. Echocardiography is the definitive diagnostic test for valvular heart disease, and auscultation often provides valuable initial clues (e.g., systolic murmur in aortic stenosis, holosystolic murmur in mitral regurgitation).
Dyspnea from Other Causes
Dyspnea can also arise from conditions outside the respiratory and cardiovascular systems.
Anemia
Anemia, defined by reduced hemoglobin levels, can cause dyspnea, especially on exertion. The severity of dyspnea in anemia varies, and there is no specific hemoglobin threshold. Evaluation for anemia should be part of the workup for dyspnea, particularly in patients with fatigue and pallor.
Ear, Nose, and Throat Disorders
Upper airway obstruction due to ear, nose, and throat (ENT) disorders can cause dyspnea, often accompanied by stridor. Causes include infections, trauma, tumors, and vocal cord dysfunction. ENT examination, laryngoscopy, and imaging studies may be needed for diagnosis.
Neuromuscular Diseases
Neuromuscular diseases affecting respiratory muscles, such as muscular dystrophy, myasthenia gravis, and amyotrophic lateral sclerosis (ALS), can lead to dyspnea. These conditions typically have other neurological manifestations in addition to dyspnea.
Mental Illnesses
Mental health conditions, including anxiety disorders, panic disorder, and somatization disorders, can present with dyspnea. Psychogenic dyspnea is a diagnosis of exclusion, considered after thorough medical evaluation has ruled out organic causes.
Iatrogenic Causes (Drug-induced)
Certain medications can induce dyspnea. Non-selective beta-blockers can cause bronchospasm, and nonsteroidal anti-inflammatory drugs (NSAIDs) can exacerbate asthma and induce dyspnea in susceptible individuals. The antiplatelet drug ticagrelor has also been associated with dyspnea in some patients. Medication review is important in the evaluation of dyspnea.
Conclusion
Dyspnea is a complex symptom with a wide range of potential underlying causes, making differential diagnosis a significant clinical challenge. A systematic approach, starting with a detailed history and physical examination, followed by targeted investigations including biomarkers and imaging, is crucial for accurate diagnosis. Understanding the diverse etiologies of dyspnea, from respiratory and cardiovascular diseases to systemic and psychogenic causes, is essential for effective patient management and improved outcomes. Prompt and accurate diagnosis is paramount to reduce mortality and the burden of disease associated with dyspnea. Clinicians must remain vigilant for the subtle clues that guide them towards the correct diagnosis and ensure timely intervention for this common and often distressing symptom.