Ear infections, clinically known as otitis media, are a widespread health issue, particularly prevalent among infants and young children. As a dedicated healthcare professional, understanding the nuances of ear infections and formulating accurate nursing diagnoses is crucial for effective patient care. This comprehensive guide delves into the essential aspects of Ear Infection Nursing Diagnosis, providing you with the expertise to deliver optimal care.
Understanding Otitis Media: A Foundation for Nursing Diagnosis
Alt Text: Illustration depicting a child experiencing ear pain, highlighting the commonality of otitis media in children.
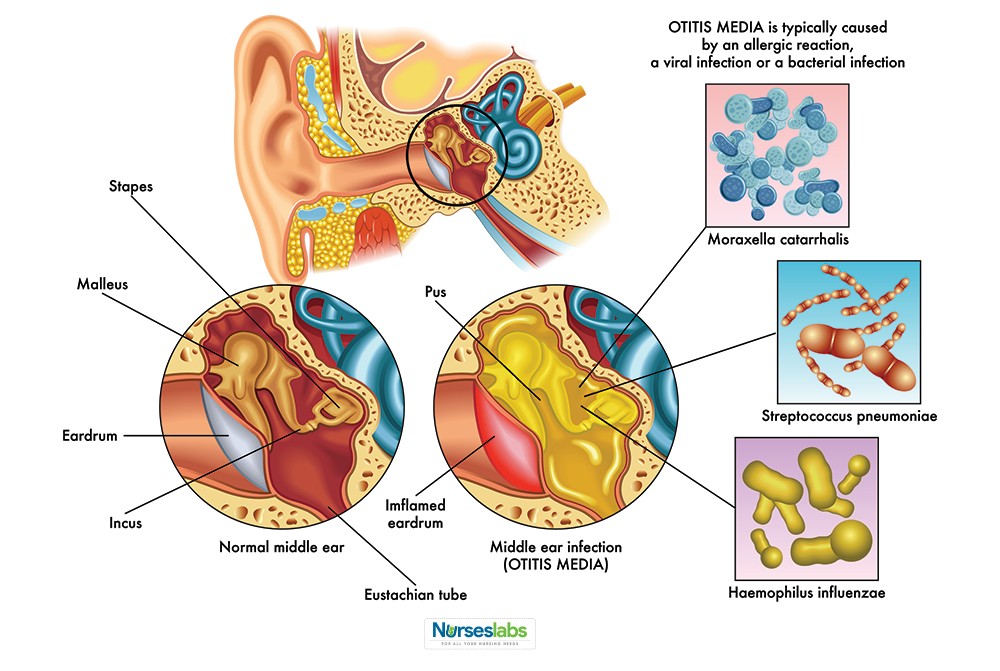
Otitis media is defined as the inflammation of the middle ear. This condition is not merely a singular entity but encompasses various forms based on its cause, duration, symptoms, and observable physical signs. Accurate classification is the first step towards an effective nursing diagnosis.
Pathophysiology: Unraveling the Mechanisms of Ear Infections
Alt Text: Comparative anatomical illustration of the Eustachian tube in children versus adults, emphasizing structural differences contributing to ear infection susceptibility in children.
A cornerstone in understanding ear infections for nursing diagnosis lies in grasping the pathophysiology. The Eustachian tube’s function is paramount in maintaining middle ear health. Dysfunction of this tube is often the primary culprit in otitis media.
In infants and young children, several factors heighten susceptibility:
- Eustachian Tube Anatomy: Infants have Eustachian tubes that are shorter, wider, and more horizontally oriented compared to adults. This anatomical configuration facilitates easier entry of nasopharyngeal secretions into the middle ear.
- Immature Immune System: A developing immune system in young children is less efficient at combating infections, making them more vulnerable to pathogens.
- Upper Respiratory Infections (URIs): Frequent URIs in children often lead to mucosal edema in the Eustachian tube, hindering its function and promoting bacterial or viral migration into the middle ear.
When the Eustachian tube is compromised – whether by edema from an URI, physical obstruction, or negative pressure – it disrupts the normal drainage and ventilation of the middle ear. This creates an environment conducive to pathogen proliferation, leading to inflammation and infection characteristic of otitis media.
Epidemiology: Recognizing the Scope of Ear Infections
Otitis media is a remarkably common childhood ailment. Statistics underscore its widespread impact:
- Prevalence in Early Childhood: By their first birthday, approximately two out of three children will have experienced at least one episode of otitis media.
- Physician Visits: Ear infections account for a significant portion of pediatric healthcare visits, estimated at around 20 million annually.
- Incidence Rate: Studies indicate that within the first two years of life, 17-20% of children will experience acute otitis media.
- Recurrent Infections: A substantial number of children, about one-third, will suffer from six or more ear infections by the age of seven.
- Peak Age Group: The highest prevalence of otitis media occurs in children between 6 and 18 months old, affecting both sexes equally.
These statistics highlight the importance for nurses to be well-versed in ear infection nursing diagnosis and management, particularly in pediatric settings.
Etiology: Identifying the Causes of Otitis Media
The development of otitis media is multifactorial, involving a combination of host, environmental, and infectious agents. Key contributing factors include:
- Immature Immune Defenses: As mentioned, a less developed immune system is a significant risk factor, making children more susceptible to infections.
- Genetic Predisposition: While the exact genetic links are still being researched, studies suggest a familial tendency for otitis media, though differentiating genetic from shared environmental factors is complex.
- Anatomical Abnormalities: Children with palate abnormalities or related muscular issues have a higher incidence of otitis media due to Eustachian tube dysfunction.
- Physiological Eustachian Tube Dysfunction: Intrinsic issues with the Eustachian tube mucosa can increase the risk of bacterial invasion and subsequent infection.
- Pathogenic Microorganisms: The most frequent bacterial culprits are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Viral infections also commonly precede or contribute to otitis media.
- Infant Feeding Practices: Research indicates that breastfeeding offers protective benefits against otitis media in infants, likely due to the transfer of maternal antibodies and the upright feeding position that reduces reflux into the Eustachian tube.
Clinical Manifestations: Recognizing Signs and Symptoms for Accurate Diagnosis
Identifying the clinical manifestations is paramount for formulating an accurate ear infection nursing diagnosis. Common signs and symptoms in children include:
- Otalgia (Ear Pain): Young children may express ear pain by tugging or pulling at their ear(s) or hair, especially when lying down.
- Otorrhea (Ear Discharge): Discharge from the ear may occur if the tympanic membrane has ruptured due to pressure buildup in the middle ear.
- Headache: Older children might verbalize headache pain associated with the ear infection.
- Upper Respiratory Infection (URI) Symptoms: Concurrent or recent cold-like symptoms such as cough, runny nose (rhinorrhea), and nasal congestion are frequently observed.
- Fever: Elevated body temperature is common, with approximately two-thirds of children with otitis media experiencing fever, though high fevers above 40°C (104°F) are less typical.
- Irritability: In infants and toddlers, increased irritability, fussiness, and unexplained crying may be the primary indicators of an ear infection, especially in preverbal children.
Assessment and Diagnostic Findings: Gathering Data for Nursing Diagnosis
Diagnosis of otitis media typically involves:
- Otoscopic Examination: Visual inspection of the tympanic membrane using an otoscope is the primary diagnostic tool. Nurses often assist or perform this assessment, noting signs of inflammation, redness, bulging, and fluid behind the eardrum.
- Pneumatic Otoscopy: This technique assesses the mobility of the tympanic membrane, which can be impaired in otitis media due to fluid accumulation.
- Tympanometry: This test measures middle ear pressure and tympanic membrane mobility, providing objective data to support the diagnosis.
- Tympanocentesis: In specific cases, particularly for severe or recurrent infections, tympanocentesis (aspiration of middle ear fluid) may be performed to identify the causative pathogens through culture and guide targeted antibiotic therapy. This is less common in routine cases.
- Laboratory Tests: Generally not required for routine otitis media. However, in infants under 12 weeks presenting with fever and otitis media, a sepsis workup might be recommended to rule out systemic infection.
Medical and Surgical Management: Overview for Nursing Care
Medical management of otitis media primarily focuses on pain relief and eradication of infection when bacterial.
Pharmacological Interventions:
- Analgesics and Antipyretics: Pain relievers like acetaminophen or ibuprofen are crucial for managing otalgia and fever.
- Antibiotics: Antibiotics are prescribed for bacterial otitis media. The choice of antibiotic depends on factors like patient age, severity of infection, and local antibiotic resistance patterns. Amoxicillin is often a first-line treatment.
Surgical Interventions:
Surgical options are considered for recurrent or chronic otitis media, or complications.
- Myringotomy and Tympanostomy Tube Placement: Myringotomy involves a small incision in the tympanic membrane to drain fluid. Tympanostomy tubes (pressure equalization or PE tubes) may be inserted to maintain drainage and ventilation of the middle ear in cases of recurrent effusions or chronic otitis media.
- Adenoidectomy: Removal of the adenoids may be considered in children with recurrent otitis media and adenoid hypertrophy, as enlarged adenoids can obstruct the Eustachian tube.
Nursing Management: Providing Holistic Care for Ear Infections
Nursing care is central to managing children with ear infections, focusing on both in-hospital and home care.
Nursing Assessment: Comprehensive Data Collection
A thorough nursing assessment includes:
- Otoscopic Examination: As mentioned, nurses are often involved in or assist with otoscopic exams.
- History Taking: Gather information regarding:
- Symptoms: Onset, duration, severity of ear pain, fever, discharge, hearing changes, irritability.
- Risk Factors: Age, daycare attendance, exposure to smoke, history of URIs, allergies, feeding methods (bottle vs. breastfeeding), family history of ear infections.
- Past Medical History: Previous ear infections, antibiotic use, presence of craniofacial anomalies or other relevant conditions.
- Pain Assessment: Utilize age-appropriate pain scales to quantify pain levels.
Nursing Diagnoses: Prioritizing Patient Needs
Based on assessment data, common nursing diagnoses for a child with an ear infection include:
- Acute Pain related to inflammation and pressure in the middle ear.
- Risk for Infection (or Active Infection) related to pathogen invasion of the middle ear.
- Impaired Verbal Communication related to potential temporary hearing loss secondary to middle ear effusion.
- Disturbed Sensory Perception (Auditory) related to middle ear obstruction and inflammation.
- Anxiety (child and/or parents) related to illness, pain, and potential hearing issues.
- Deficient Knowledge (parents/caregivers) regarding otitis media, treatment, prevention, and home care.
Nursing Care Planning and Goals: Setting Desired Outcomes
Key goals in nursing care planning for otitis media are:
- Pain management and relief.
- Resolution of infection.
- Restoration of normal hearing (or minimizing hearing impairment).
- Prevention of recurrence.
- Parent/caregiver understanding of the condition and its management.
Nursing Interventions: Implementing Evidence-Based Care
Nursing interventions are focused on achieving the established goals:
- Pain Management:
- Administer analgesics as prescribed and assess effectiveness.
- Apply local heat (warm compress) to the affected ear for comfort, if appropriate.
- Position the child comfortably, often elevating the head or positioning them on the unaffected side to promote drainage and reduce pressure.
- Infection Management:
- Administer antibiotics as prescribed and educate caregivers on completing the full course.
- Monitor for signs of worsening infection or complications.
- Maintain hygiene practices to prevent spread of infection.
- Promoting Communication:
- Assess hearing ability and note any changes.
- Speak clearly and face the child when communicating.
- Reduce background noise to improve communication.
- Educate caregivers about potential temporary hearing loss and strategies to facilitate communication.
- Education and Support:
- Educate parents/caregivers about otitis media, its causes, symptoms, treatment, and prevention.
- Teach proper medication administration.
- Emphasize the importance of follow-up appointments.
- Provide guidance on preventive measures such as breastfeeding, avoiding smoke exposure, and proper hand hygiene.
- Address parental anxiety and concerns, providing emotional support and reassurance.
Evaluation: Assessing Effectiveness of Nursing Care
Nursing care effectiveness is evaluated based on:
- Child reports or demonstrates reduced pain levels.
- Resolution of infection (absence of fever, ear discharge, improvement in otoscopic findings).
- Return to baseline hearing ability.
- Parents/caregivers demonstrate understanding of otitis media management and preventive strategies.
Documentation: Ensuring Continuity of Care
Accurate and thorough documentation is essential, including:
- Assessment findings (otoscopic exam, symptoms, pain level).
- Nursing diagnoses.
- Care plan and interventions implemented.
- Medication administration.
- Patient and family education provided.
- Patient response to interventions and progress towards goals.
- Discharge instructions.
Conclusion: Expert Nursing Care for Ear Infections
Effective nursing diagnosis and management of ear infections are crucial for alleviating symptoms, resolving infections, and preventing complications, particularly in vulnerable pediatric populations. By understanding the pathophysiology, clinical presentation, and evidence-based nursing interventions, you, as a healthcare professional, can significantly enhance the well-being of patients affected by ear infections. This comprehensive guide serves as a foundation for providing expert, compassionate, and effective nursing care for individuals with ear infections.