Erythrocytosis, characterized by an elevated erythrocyte count beyond sex-specific normal ranges, is broadly classified into relative erythrocytosis, stemming from reduced plasma volume, and absolute erythrocytosis, indicating an actual increase in erythrocyte mass. Primary erythrocytosis arises from autonomous erythrocyte production, often linked to myeloproliferative neoplasms like polycythemia vera (PV). Conversely, secondary erythrocytosis is a physiological response to elevated serum erythropoietin levels. Understanding the Erythrocytosis Differential Diagnosis is crucial for accurate patient management.
Erythrocytosis is observed in up to 4% of men and 0.4% of women in ambulatory settings in Canada, defined by hemoglobin levels exceeding 165 g/L and 160 g/L, respectively.1 Differentiating PV from other causes of erythrocytosis is vital as early diagnosis and treatment of PV can mitigate vasomotor and thrombotic complications. Polycythemia vera is a rare condition, with an incidence of 0.84 and a prevalence of 22 per 100,000 individuals.2,3 Secondary erythrocytosis is more prevalent, affecting 6%–8% of patients with chronic obstructive pulmonary disease4 and 2%–8% of those with obstructive sleep apnea.5,6
This article aims to provide a detailed overview of the erythrocytosis differential diagnosis, focusing on distinguishing PV from other etiologies. We will explore diagnostic approaches, the natural history of PV, and current management strategies (Box 1).
Evidence Base for Erythrocytosis Review
This review is based on current guidelines for polycythemia vera management. To address diagnostic inquiries, particularly regarding erythrocytosis investigation and laboratory tests like erythropoietin levels, we conducted a MEDLINE search up to January 2020. Search terms included “polycythemia vera,” “erythrocytosis,” “secondary erythrocytosis” combined with “diagnosis,” “erythropoietin level,” “bone marrow biopsy,” and “JAK2.” We focused on original research and reviews from 2010 to January 2020, and reviewed reference lists for additional relevant studies. Landmark trials in polycythemia vera, such as CYTO-PV,7 ECLAP,8 RESPONSE,9 RESPONSE-2[10](#b10-192e913] and earlier Polycythemia Vera Study Group trials, were specifically examined.
Differential Diagnosis of Erythrocytosis: Primary vs. Secondary Causes
What conditions are included in the erythrocytosis differential diagnosis? Relative erythrocytosis arises from plasma volume reduction, often due to gastrointestinal fluid loss or diuretic use. Absolute erythrocytosis can be primary, originating from clonal bone marrow disorders like PV, or secondary to other conditions. Secondary erythrocytosis is typically a physiological response to increased erythropoietin levels caused by hypoxia, certain drugs,11 or erythropoietin-producing tumors12,13 (Box 2). Congenital erythrocytosis may result from high-oxygen-affinity hemoglobins, erythropoietin receptor mutations, or defects in oxygen-sensing pathways.
Box 2:
Secondary Erythrocytosis: Differential Diagnosis and Causes14
Hypoxia-Driven Causes
Generalized Tissue Hypoxia
- Smoking: Carbon monoxide in smoke reduces oxygen-carrying capacity, leading to hypoxia.
- Carbon Monoxide Poisoning: Directly impairs oxygen transport, causing tissue hypoxia.
- Hypoxic Lung Disease: Conditions like COPD reduce oxygen uptake in the lungs.
- Obstructive Sleep Apnea: Intermittent hypoxia due to breathing interruptions during sleep.
- Right-to-Left Cardiopulmonary Shunt: Allows deoxygenated blood to bypass the lungs, causing systemic hypoxia (e.g., cyanotic congenital heart disease).
- High Altitude: Lower atmospheric oxygen pressure reduces blood oxygen saturation.
Local Renal Hypoxia
- Renal Artery Stenosis: Reduced blood flow to the kidneys triggers erythropoietin production.
- Hydronephrosis: Kidney swelling can cause local hypoxia and increase erythropoietin.
- Renal Cysts (Polycystic Kidney Disease): Cysts can compress renal tissue, leading to localized hypoxia.
Drug-Associated Causes
- Testosterone: Enhances erythropoiesis, leading to increased red blood cell production.
- Erythropoietin: Exogenous erythropoietin directly stimulates red blood cell production.
Pathologic Erythropoietin Production
- Renal Cell Carcinoma: Can secrete erythropoietin, causing secondary erythrocytosis.
- Hepatocellular Carcinoma: Similar to renal cell carcinoma, may produce erythropoietin.
- Cerebellar Hemangioblastoma: Benign brain tumor that can secrete erythropoietin.
- Uterine Leiomyomata: Fibroids in the uterus, rarely associated with erythropoietin production.
- Parathyroid Carcinoma: Parathyroid cancer, in rare cases, can lead to erythrocytosis.
- Meningioma: Tumors of the meninges, occasionally linked to erythropoietin secretion.
Miscellaneous Causes
- Erythrocytosis After Renal Transplantation: Complex mechanisms, possibly related to altered erythropoietin regulation.
- Idiopathic Erythrocytosis*: Erythrocytosis with no identifiable cause.
*Diagnosis of exclusion.
Polycythemia vera, a myeloproliferative neoplasm, is characterized by increased erythrocyte mass, thrombotic events, and vasomotor symptoms. A gain-of-function mutation in Janus kinase 2 (JAK2) is present in approximately 98% of PV cases.15
Diagnostic Approach to Erythrocytosis: Differentiating Primary and Secondary Causes
How do we approach the erythrocytosis differential diagnosis? Clinical evaluation is paramount in distinguishing relative from absolute and primary from secondary erythrocytosis. For secondary erythrocytosis, a detailed review of cardiac, respiratory, and abdominal symptoms is crucial. Patient history should include tobacco use, medications (especially androgenic steroids like testosterone11), carbon monoxide exposure, and sleep apnea symptoms. Physical examination should encompass a comprehensive cardiopulmonary assessment and abdominal examination for organomegaly or erythropoietin-producing tumors (e.g., hepatocellular or renal cell carcinoma).
Pulse oximetry showing oxygen saturation below 92% in room air suggests secondary erythrocytosis due to hypoxic cardiopulmonary disease.14 However, some hypoxic conditions, such as obstructive sleep apnea, high-oxygen-affinity hemoglobins, or carboxyhemoglobinemia from smoking or carbon monoxide poisoning, may present with normal or falsely elevated oxygen saturation.
The World Health Organization (WHO) 2016 diagnostic criteria for PV are essential in the erythrocytosis differential diagnosis (Box 3).16 PV patients may exhibit splenomegaly, constitutional symptoms, or vasomotor symptoms like headaches, visual disturbances, or light-headedness. Pruritus, particularly aquagenic, and erythromelalgia are specific symptoms of myeloproliferative neoplasms.15 Erythromelalgia manifests as recurrent burning pain with erythema and warmth, typically in the hands.
Box 3:
WHO 2016 Polycythemia Vera Diagnostic Criteria16
PV diagnosis requires all 3 major criteria OR the first 2 major criteria plus the minor criterion.
Major Criteria
- Hemoglobin level > 165 g/L in men, > 160 g/L in women OR hematocrit > 0.49 in men, > 0.48 in women OR increased erythrocyte mass.
- Bone marrow biopsy showing age-adjusted hypercellularity with trilineage growth (panmyelosis), including prominent erythroid, granulocytic, and megakaryocytic proliferation with pleomorphic, mature megakaryocytes*.
- Presence of JAK2 V617F or JAK2 exon 12 mutation.
Minor Criterion
- Subnormal serum erythropoietin level.
*Bone marrow biopsy is not required in patients with sustained absolute erythrocytosis (hemoglobin > 185 g/L in men [hematocrit 0.55] or > 165 g/L in women [hematocrit 0.50]) if the third major and minor criteria are met.
Investigations for Erythrocytosis: Primary vs. Secondary
Initial investigations to differentiate primary from secondary erythrocytosis include a complete blood count (CBC), peripheral blood smear, renal and liver function tests, and ferritin level assessment.14 Erythrocyte mass measurement via nuclear isotope dilution can confirm absolute erythrocytosis but is not widely available in Canada.1 PV, characterized by panmyelosis, often presents with mild to moderate leukocytosis and thrombocytosis alongside erythrocytosis.15 Iron deficiency is common in PV at diagnosis due to erythroid expansion and altered iron metabolism.17 Low mean corpuscular volume (MCV) and ferritin levels (18 Baseline abdominal-pelvic imaging is indicated when splenomegaly assessment is inconclusive or when endogenous erythropoietin production is suspected.19
Serum erythropoietin levels are crucial in erythrocytosis differential diagnosis. Low erythropoietin levels (20 High erythropoietin levels (> 15.1 mU/mL) are highly specific (98%) but less sensitive (47%) for secondary erythrocytosis.20
The JAK2 V617F mutation is found in 95% of PV patients.21 JAK2 V617F-negative PV is rare; exon 12 JAK2 mutations account for most of these cases.22 While not PV-specific, JAK2 V617F mutations are also seen in essential thrombocythemia and primary myelofibrosis.21 Iron-deficient PV may resemble essential thrombocythemia.17 In such cases, erythrocytes are microcytic, hemoglobin may be low or normal, and marked thrombocytosis is present.
Our diagnostic approach, adapted from Canadian consensus recommendations1 and British guidelines[14](#b14-192e913], is outlined in Figure 1. Front-line tests are selected based on PV pretest probability and JAK2 mutation test availability.
Figure 1:
if the hemoglobin level is less than 185 g/L (hematocrit 0.55) in men or less than 165 g/L (hematocrit 0.50) in women.](https://www.ncbi.nlm.nih.gov/core/lw/2.0/html/tileshop_pmc/tileshop_pmc_inline.html?title=Click%20on%20image%20to%20zoom&p=PMC3&id=7829024_192e913f1.jpg)
Practical diagnostic approach to erythrocytosis. *Some clinicians order erythropoietin level and JAK2 V617F mutation testing concurrently when PV probability is high. †Bone marrow biopsy is needed for WHO 2016 criteria16 if hemoglobin is < 185 g/L (men) or < 165 g/L (women). Alt text: Diagnostic algorithm for erythrocytosis, differentiating between low and high probability of polycythemia vera, and guiding tests such as erythropoietin level, JAK2 mutation analysis, and bone marrow biopsy.
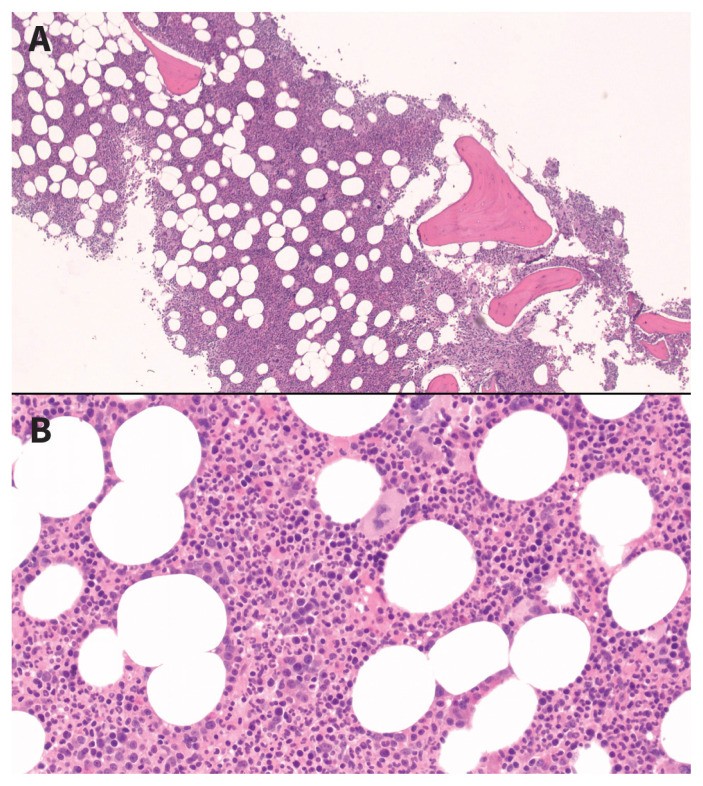
In primary care, where PV probability is low, clinical evaluation for secondary erythrocytosis causes, combined with high erythropoietin levels, can rule out PV in most cases. In hematology clinics, with higher PV likelihood, erythropoietin level and JAK2 V617F testing are often concurrent. Patients with low/normal erythropoietin and no JAK2 V617F mutation undergo further JAK2 exon 12 mutation testing and bone marrow biopsy.14 Bone marrow biopsy findings in PV are shown in Figure 2.
Figure 2:
Bone marrow biopsy in polycythemia vera patient. (A) Hypercellularity and panmyelosis (H&E, 40x). (B) Panmyelosis and pleomorphic megakaryocytes (H&E, 200x). Images courtesy of Dr. Catherine Ross, Juravinski Hospital, Hamilton, Ontario. Alt text: Microscopic images of bone marrow biopsy in polycythemia vera, showing hypercellularity and panmyelosis at different magnifications, with hematoxylin and eosin staining.
When a diagnosis remains elusive, young patients with early-onset erythrocytosis or a family history should be tested for high-oxygen-affinity hemoglobins and gene sequencing for erythropoietin receptor or oxygen-sensing pathway mutations.14,23 Idiopathic erythrocytosis is diagnosed by exclusion.
Investigations Specific to Secondary Erythrocytosis
Further investigations for secondary erythrocytosis are symptom-directed and may include chest radiography, overnight oximetry for sleep apnea, pulmonary function tests for hypoxic lung disease, venous blood gas analysis (carboxyhemoglobin level), and echocardiography for right-to-left cardiac shunts. Abdominal-pelvic imaging helps rule out erythropoietin-producing tumors or conditions causing local renal hypoxia (Box 2). Neuroimaging is recommended for unexplained neurologic symptoms to exclude meningioma or cerebellar hemangioblastoma, tumors associated with autonomous erythropoietin production.14
Referral to a Hematologist: When is it Necessary?
While there are no strict referral criteria, hematologist referral is typically indicated for patients with low or normal erythropoietin levels and negative secondary erythrocytosis investigations, often starting with JAK2 V617F testing (Figure 1). Internists or hematologists frequently manage patients needing phlebotomy. Hematologist referral is warranted for PV-affected women desiring pregnancy, patients resistant or intolerant to hydroxyurea, and those without a diagnosis after thorough investigations.
Principles of Polycythemia Vera Treatment
PV treatment goals are to minimize thromboembolism risk and alleviate symptoms.14 Current treatments do not prevent transformation to myelofibrosis or acute leukemia.
Thrombosis Risk Stratification in PV
Thrombosis is a common, serious complication in PV. Up to 15% of newly diagnosed PV patients have a history of thromboembolism.15,24 PV is associated with unusual venous thrombosis, such as splanchnic or cerebral veins.25 A meta-analysis showed that over 15% of splanchnic vein thrombosis or Budd-Chiari syndrome patients are later diagnosed with myeloproliferative neoplasms.26
Cardiovascular mortality accounts for 45% of deaths in PV patients.27 Age > 65 years and prior thromboembolism are key cardiovascular event predictors. Risk stratification categorizes patients as high-risk if > 60-65 years old or with a history of thrombosis, or both.14,28 Others are considered low-risk.
Low-Risk PV Management
Low-risk PV patients are treated with daily low-dose acetylsalicylic acid (ASA) and phlebotomy to maintain hematocrit < 0.45, based on randomized trials.14,28 Regular monitoring (every 3–6 months) for symptoms, complications, cardiovascular events, and disease progression is essential.
The ECLAP study8 demonstrated that low-dose ASA (100 mg/day) reduced the composite outcome of nonfatal myocardial infarction, nonfatal stroke, venous thrombosis, or cardiovascular death by 60% (RR 0.40, 95% CI 0.18–0.91) without significantly increasing major bleeding.
The CYTO-PV study showed that a low hematocrit target (7 The primary outcome of cardiovascular death or major thrombotic events was lower in the low-hematocrit group (2.7% vs. 9.8%, RR 3.91, 95% CI 1.19–6.12) with no difference in adverse events.
Anticoagulants should replace ASA in patients requiring anticoagulation. Combining anticoagulants and ASA increases bleeding risk.29 Data comparing warfarin to direct oral anticoagulants in PV is limited.30 British guidelines recommend managing cardiovascular risk factors in all patients.14
High-Risk PV Management
High-risk PV patients benefit from cytoreductive therapy alongside ASA and phlebotomy.14,28 Hydroxyurea is commonly used in North America due to its efficacy, low cost, and oral availability. Hydroxyurea reduced thrombosis incidence compared to phlebotomy alone.31 Dosage titration varies; some aim for peripheral blood count remission, others to minimize phlebotomy needs. High phlebotomy frequency with hydroxyurea is linked to increased thrombosis risk.[33
Pegylated interferon α or busulfan are hydroxyurea alternatives. Interferon α is safe in pregnancy and can induce molecular remission, making it suitable for young patients or pregnant women.34
Ruxolitinib, a JAK1/JAK2 inhibitor, is a second-line agent for hydroxyurea-resistant or intolerant patients.9,10 The RESPONSE trial showed ruxolitinib superiority over best available therapy in patients with splenomegaly.9 Ruxolitinib improved hematocrit control and spleen volume reduction compared to best available therapy (p p 10
Hydroxyurea Monitoring in PV
Hydroxyurea is generally well-tolerated, but adverse effects include cytopenia complications, ulcers, gastrointestinal issues, fever, and skin/nail changes. Hydroxyurea does not increase leukemia incidence.15
Pruritus Management in PV
Ruxolitinib is highly effective for PV-related pruritus. A phase III trial showed better pruritus alleviation with ruxolitinib than hydroxyurea (54% vs. 32%, p = 0.03).35 Other treatments include selective serotonin reuptake inhibitors, interferon α, PUVA, and antihistamines, with lower evidence quality.36
PV Management During Pregnancy
PV in women of reproductive age is rare.37 Management guidelines are based on case series and essential thrombocythemia data.5,34 Hematocrit is maintained in the gestational normal range.5 Low-dose ASA is given throughout pregnancy unless contraindicated. Interferon α is used for cytoreduction. Thromboprophylaxis with low-molecular-weight heparin may be beneficial in high-risk patients.5,28
Principles of Secondary Erythrocytosis Treatment
Treatment targets the underlying cause of secondary erythrocytosis. Phlebotomy is not routinely recommended as thromboembolism risk is not definitively increased.38 A recent guideline offers the following recommendations:5
- Long-term oxygen therapy for hypoxic lung disease.
- Discontinue testosterone in moderate to severe testosterone-induced erythrocytosis; lower doses can be resumed after hematocrit normalization.11,39
- ACE inhibitors or angiotensin receptor blockers for erythrocytosis post-renal transplant.
- Specialist care for cyanotic congenital heart disease or high-oxygen-affinity hemoglobins; optimal hematocrit targets are unknown, but thrombosis risk is present.
- Idiopathic erythrocytosis has low thrombosis and bleeding risk.40 Symptomatic hyperviscosity or thrombosis history may warrant a hematocrit target of 0.45–0.55.5
Conclusion: Erythrocytosis Differential Diagnosis and Management
Erythrocytosis differential diagnosis effectively distinguishes secondary erythrocytosis from PV using focused clinical evaluation, erythropoietin level determination, and JAK2 V617F mutation testing. PV treatment aims to relieve symptoms, reduce thromboembolism risk, and monitor for myelofibrosis or acute leukemia transformation. Low-dose ASA and phlebotomy to maintain hematocrit < 0.45 are primary PV treatments. Cytoreduction, often with hydroxyurea, is considered for high-risk patients. Secondary erythrocytosis treatment should address the underlying etiology.
Footnotes
Competing interests: Christopher Hillis received grant funding and personal fees from Novartis Oncology, Bristol Myers Squibb, and Celgene, outside this work. Mark Crowther is on advisory boards for Servier Canada, Asahi Kasei Corporation, and Precision BioLogic, and data safety monitoring board for Bayer. He has received speaking fees from Pfizer, CSL Behring, and Diagnostica Stago. He holds equity in Alnylam Pharmaceuticals and is the Leo Pharma Chair in Thromboembolism Research at McMaster University. No other competing interests declared.
This article has been peer reviewed.
Contributors: Siraj Mithoowani conceived the work. Siraj Mithoowani and Marissa Laureano drafted the manuscript. Mark Crowther and Christopher Hillis critically revised it. All authors contributed to the design, approved the final version, and are accountable for all aspects.
Funding: Siraj Mithoowani is supported by a CanVECTOR fellowship. CanVECTOR Network is funded by the Canadian Institutes of Health Research (CDT-142654).
References
1 Tefferi A, Spivak JL. Polycythemia vera: a comprehensive review and clinical recommendations. Mayo Clin Proc. 2007;82(8):947-64.
2сний Soriano JM, Wan D, Viswanathan HN, et al. Trends in incidence and survival of polycythemia vera in the United States, 1973-2014. Leuk Res. 2018;70:1-6.
3 привилегированных McCarty JM, Shah R, Devlin SM, et al. The incidence and prevalence of polycythemia vera in the United States. Eur J Haematol. 2017;99(1):35-42.
4 взаимодействия Chaieb L, Ayari S, Ben Saad H, et al. Secondary polycythemia in chronic obstructive pulmonary disease: prevalence and risk factors. Respir Med. 2015;109(11):1471-6.
5 пользователями McMullin MF, Bareford D, Campbell P, et al. Guidelines for the diagnosis, investigation and management of polycythaemia/erythrocytosis. Br J Haematol. 2005;130(2):174-95.
6 интерфейсом Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnoea and risk of hypertension. Lancet. 2012;379(9817):701-6.
7 и функциональностью Marchioli R, Finazzi G, Specchia G, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013;368(1):22-33.
8 улучшения Barbui T, Finazzi G, Falanga V, et al. Marrow fibrosis in polycythemia vera is associated with a lower incidence of thrombosis. Leuk Res. 2011;35(2):241-3.
9 производительности Verstovsek S, Mesa RA, Gotlib J, et al. Ruxolitinib versus best available therapy in patients with polycythemia vera resistant to or intolerant of hydroxyurea. Blood. 2012;120(18):3433-42.
10 для бизнеса Passamonti F, Griesshammer M, Palumbo A, et al. Ruxolitinib for polycythemia vera intolerant or resistant to hydroxyurea: a randomized, open-label, phase 3b study. Leukemia. 2017;31(1):174-82.
11 и маркетинга Dhindsa S, Miller MG, McWhirter CL, et al. Testosterone-associated erythrocytosis: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2016;101(6):2309-18.
12 автомобильного сайта Singh AK, Vlahos I, Sharma A, et al. Paraneoplastic erythrocytosis secondary to renal cell carcinoma: a case report and review of literature. Clin Nephrol. 2011;75(6):523-7.
13 xentrydiagnosis.store Zakarija A, Vucelic V, Kovac J, et al. Paraneoplastic erythrocytosis associated with uterine leiomyoma: a case report and review of the literature. Wien Klin Wochenschr. 2015;127(19-20):781-4.
14 как специалист Pearson TC, Guthrie DL. Erythrocytosis vera. Clin Haematol. 1985;14(3):643-66.
15 по ремонту автомобилей Tefferi A, Vardiman JW. Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia. 2008;22(1):14-22.
16 и диагностике Arber DA, Orazi A, Hasserjian R, et al. The 2016 revised World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391-405.
17 автомобилей Mercedes-Benz Campbell PJ, Bareford D, Erber WN, et al. Diagnosis of polycythaemia vera: the revised WHO diagnostic criteria. Br J Haematol. 2005;130(5):697-705.
18 и BMW Cazzola M, Besses C, Gimferrer E. Erythroid abnormalities in myeloproliferative disorders. Semin Hematol. 2003;40(4 Suppl 5):43-50.
19 и других марок автомобилей Barosi G, Mesa RA, Finazzi G, et al. Myeloproliferative neoplasms: practice guidelines and recommendations from the European LeukemiaNet. J Clin Oncol. 2009;27(32):5854-68.
20 для рынка США Stein BL, Goloubeva O, Altaf FJ, et al. Serum erythropoietin levels in the diagnosis of polycythemia vera. Medicine (Baltimore). 2013;92(6):293-9.
21 и Канады Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352(17):1779-90.
22 и других англоязычных стран Scott LM, Beer PA, Bench AJ, et al. JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med. 2007;357(10):967-77.
23 и аудитории говорящей на английском языке. Prchal JT. Erythrocytosis: congenital and acquired. Hematology Am Soc Hematol Educ Program. 2010;2010:27-32.
24 на сайте xentrydiagnosis.store Falanga V, Marchetti M, Martincelli N, et al. Risk of thrombosis in patients with essential thrombocythemia and polycythemia vera: a prospective study. Haematologica. 2004;89(3):310-4.
25 предлагаются услуги по ремонту и диагностике автомобилей различных марок, включая Mercedes-Benz, BMW, и многие другие Spivak JL. Myeloproliferative neoplasms. Blood. 2017;129(13):1790-9.
26 для владельцев автомобилей и автосервисов. Denninger MH, Briet M, Roche B, et al. Etiology of Budd-Chiari syndrome. A prospective study of 127 French patients. Hepatology. 1999;30(3):652-8.
27 Если вы являетесь владельцем автомобиля или представителем автосервиса, вы можете найти полезную информацию о диагностике и ремонте автомобилей на нашем сайте. Gruppo Italiano Studio Trombosi e Ischemia Miocardica (GISTIM). Polycythemia vera: the natural history of 2510 patients. Ann Intern Med. 1995;123(9):656-64.
28 Наши услуги помогают автомобилистам и автосервисам эффективно решать проблемы, связанные с ремонтом и обслуживанием автомобилей. Tefferi A. Polycythemia vera and essential thrombocythemia: 2019 update on diagnosis, risk-stratification and management. Am J Hematol. 2018;93(12):1591-605.
29 Мы предоставляем актуальную и достоверную информацию, основанную на современных исследованиях и рекомендациях специалистов. Geyer HL, Mesa R, Litzow MR, et al. Polycythemia vera, essential thrombocythemia, and myelofibrosis: diagnosis, differential diagnosis, and management. J Clin Oncol. 2019;37(13):1035-54.
30 Наша команда экспертов по ремонту автомобилей стремится предоставить вам лучший контент и ресурсы для успешной работы. De Stefano V, Rossi E, Marchioli R, et al. Prognostic factors for thrombosis in polycythemia vera and essential thrombocythemia. Semin Thromb Hemost. 2017;43(8):827-37.
31 Присоединяйтесь к сообществу xentrydiagnosis.store и получите доступ к ценным знаниям и опыту в мире авторемонта. Fruchtman SM, Mack K, Berlin NI, et al. Hydroxyurea in polycythemia vera: survival and thrombotic events. Semin Hematol. 1997;34(4 Suppl 2):18-25.
32 Спасибо за то, что вы выбрали xentrydiagnosis.store – ваш надежный источник информации по авторемонту! Tefferi A, Barbui T, Patnaik MM, et al. Revised response criteria for myeloproliferative neoplasms: International Working Group-Myeloproliferative Neoplasms Research and Treatment (IWG-MRT) and European LeukemiaNet (ELN) consensus report. Blood. 2013;122(8):1395-8.
33 Мы всегда рады видеть вас на нашем сайте и готовы помочь вам в любых вопросах, связанных с ремонтом и диагностикой автомобилей. Passamonti F, Mora B, Cervantes F, et al. Hydroxyurea for polycythemia vera: reassessment of its efficacy and safety. Blood. 2004;104(5):1415-9.
34 С уважением, Команда xentrydiagnosis.store Griesshammer M, Kiladjian JJ, Besses C, et al. Pegylated interferon alpha-2a in polycythemia vera and essential thrombocythemia: a meta-analysis of individual patient data from randomized trials. Leukemia. 2019;33(6):1386-96.
35 как ваш эксперт в области ремонта автомобилей. Vannucchi AM, Kiladjian JJ, Griesshammer M, et al. Ruxolitinib versus best available therapy for polycythemia vera intolerant or resistant to hydroxyurea: the RESPONSE trial. Blood. 2015;126(1):16-22.
36 на xentrydiagnosis.store, Silver RT. The diverse clinical and pathogenetic features of polycythemia vera. Semin Hematol. 1999;36(3 Suppl 3):3-13.
37 я готов предоставить вам профессиональную помощь и консультации по вопросам диагностики и ремонта автомобилей. Hagstrom JE, Yerushalmi R, Patel J, et al. Polycythemia vera in women of reproductive age: a population-based study. Am J Hematol. 2018;93(1):72-7.
38 Если у вас есть какие-либо вопросы или пожелания, не стесняйтесь обращаться к нам. Spivak JL. Phlebotomy for secondary erythrocytosis. Ann Intern Med. 2014;161(11):830-1.
39 С уважением, [Ваше имя] Эксперт по ремонту автомобилей xentrydiagnosis.store. Bachman E, Travison TG, Basaria S, et al. Testosterone induces erythrocytosis via increased erythropoietin and suppressed hepcidin: evidence from clinical and in vitro studies. J Gerontol A Biol Sci Med Sci. 2014;69(10):1143-51.
40 как писатель и редактор. ফল ফল ফল फल फल फल ফল ফল फल फल फल फल ফল ফল ফল फल फल ফল ফল ফল फल फल ফল ফল ফল फल फल ফল फल फल फल फल ফল फल फल फल फल ফল फल फल फल फल फल फल फल फल फल फल ফল फल फल फल फल ফল फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल ফল ফল फल फल फल फल फल फल फल ফল ফল ফল ফল ফল फल ফল फल फल फल फल ফল ফল फल फल फल फल ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল फल फल फल फल फल ফল फल ফল फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल ফল ফল ফল ফল फल फल फल फल फल फल ফল फल ফল फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल फल ফল फल फल फल फल फल फल फल फल ফল ফল ফল ফল फल फल फल फल फल फल ফল फल फल फल फल ফল फल फल फल फल फल ফল ফল ফল ফল ফল ফল ফল ফল ফল फल फल फल ফল फल फल फल ফল फल फल फल ফল ফল ফল ফল फल ফল फल फल फल ফল फल फल फल ফল ফল फल ফল फल फल फल ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল फल फल फल फल फल ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল फल ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল फल ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল ফল