Crafting an effective nursing care plan is a cornerstone of quality patient care. It requires a systematic approach to accurately identify patient needs, potential risks, and to outline a strategy for achieving desired health outcomes. This guide provides a comprehensive overview of developing nursing care plans, enriched with examples of nursing diagnoses to enhance your understanding and skill in creating patient-centered care strategies. Whether you are a student nurse or a seasoned professional, this resource offers valuable insights and practical guidance to improve your care planning process.
Understanding Nursing Care Plans
A nursing care plan (NCP) is a structured, formal document that pinpoints a patient’s current health needs and anticipates potential future risks. It serves as a vital communication tool among nurses, patients, and the broader healthcare team, ensuring a cohesive approach to patient care. Without well-defined care plans, the consistency and quality of patient care can be significantly compromised. The care planning process is dynamic, beginning upon patient admission and continuously evolving in response to changes in the patient’s condition and the evaluation of care effectiveness. This patient-centered approach is fundamental to excellence in nursing practice.
Types of Nursing Care Plans: Formal vs. Informal and Standardized vs. Individualized
Nursing care plans can be broadly classified into informal and formal types. An informal nursing care plan is essentially a mental strategy, a nurse’s thought process for patient care. In contrast, a formal nursing care plan is documented, either written or digital, providing a structured guide for patient care management.
Formal care plans are further divided into standardized and individualized plans. Standardized care plans are pre-set guidelines designed for patients with common needs. They ensure consistent care for typical conditions but may lack personalization. Individualized care plans, on the other hand, are customized to address the unique needs of each patient, going beyond the scope of standardized plans to provide tailored care.
Delving Deeper: Standardized and Individualized Care Plans
Standardized care plans are pre-approved by healthcare facilities to guarantee uniform care for patients with specific conditions. These plans streamline care delivery, ensuring essential criteria are met efficiently. They are particularly useful for common conditions, saving nurses time on routine tasks. However, standardized plans are not designed to meet the specific needs of every patient and serve primarily as a foundation for developing more personalized approaches. Many resources, including those available online, offer standardized care plan templates that can be adapted.
Individualized care plans are developed by modifying standardized plans to align with a patient’s unique health status, preferences, and goals. This method ensures care is not only effective but also deeply personal and holistic. By tailoring care, nurses can significantly enhance patient satisfaction, as patients feel more valued and understood when their specific needs are addressed. In today’s healthcare landscape, where patient satisfaction is a key indicator of quality, individualized care plans are increasingly important.
Tips for Individualizing a Nursing Care Plan:
- Detailed Assessment: Conduct a thorough patient assessment to capture all unique aspects of their condition, lifestyle, and preferences.
- Patient Involvement: Actively involve patients in the planning process to incorporate their goals and preferences.
- Flexibility: Be prepared to adjust the care plan as the patient’s condition evolves.
- Focus on Uniqueness: Identify and address needs that are not covered by standard protocols.
Objectives of Nursing Care Plans
The primary objectives of a nursing care plan are to:
- Promote Evidence-Based Care: Ensure nursing care is rooted in the latest research and best practices, creating a comfortable and effective healthcare environment.
- Support Holistic Care: Address the patient’s physical, psychological, social, and spiritual needs comprehensively, focusing on both disease management and prevention.
- Establish Care Programs: Develop structured care pathways and bundles that facilitate team collaboration and standardize care for specific conditions, improving outcomes.
- Define Goals and Outcomes: Clearly identify and differentiate between healthcare goals and expected patient outcomes to guide care effectively.
- Enhance Communication and Documentation: Improve the clarity and effectiveness of care plan communication and documentation among healthcare providers.
- Measure Nursing Care Effectiveness: Provide a framework for evaluating the impact and quality of nursing care delivered.
Purposes and Importance of Nursing Care Plans
Nursing care plans are crucial for several reasons:
- Defining the Nurse’s Role: They highlight the distinct role of nurses in patient care, emphasizing independent nursing actions beyond medical directives.
- Guiding Individualized Care: Care plans serve as a detailed roadmap for patient care, enabling nurses to apply critical thinking in tailoring interventions to individual needs.
- Ensuring Continuity of Care: By providing a consistent care framework, care plans ensure that all healthcare team members deliver uniform, high-quality care across different shifts and departments.
- Coordinating Healthcare Team Efforts: They facilitate coordinated care by keeping all team members informed of patient needs and planned actions, preventing gaps in care.
- Documentation and Accountability: Care plans document planned observations, nursing actions, and patient/family instructions. Accurate documentation in the care plan is essential as it serves as evidence of care provided.
- Guiding Staff Assignments: They aid in assigning staff based on patient needs, ensuring clients are cared for by professionals with the necessary skills.
- Monitoring Patient Progress: Care plans help track patient progress and facilitate necessary adjustments to the care strategy as health conditions change.
- Supporting Reimbursement: Insurance providers often use care plan documentation to determine coverage and reimbursement for healthcare services.
- Defining Patient Goals: They empower patients by involving them in their care, aligning treatment with their personal health goals.
Key Components of a Nursing Care Plan
A comprehensive nursing care plan typically includes several essential components:
- Nursing Diagnoses: Clear statements of the patient’s health problems or potential issues that nurses are qualified and licensed to treat. Examples of nursing diagnoses include “Risk for Infection,” “Acute Pain,” or “Impaired Physical Mobility.”
- Client Problems: A broader description of health issues that may encompass medical diagnoses and collaborative problems.
- Expected Outcomes: Specific, measurable, achievable, relevant, and time-bound (SMART) goals for patient improvement.
- Nursing Interventions: Actions nurses will take to achieve the expected outcomes, tailored to the nursing diagnoses.
- Rationales: The scientific reasons behind selecting particular nursing interventions, often emphasized in student care plans to enhance learning.
- Evaluation: A process to assess the patient’s progress towards achieving the set goals and to determine the effectiveness of the care plan.
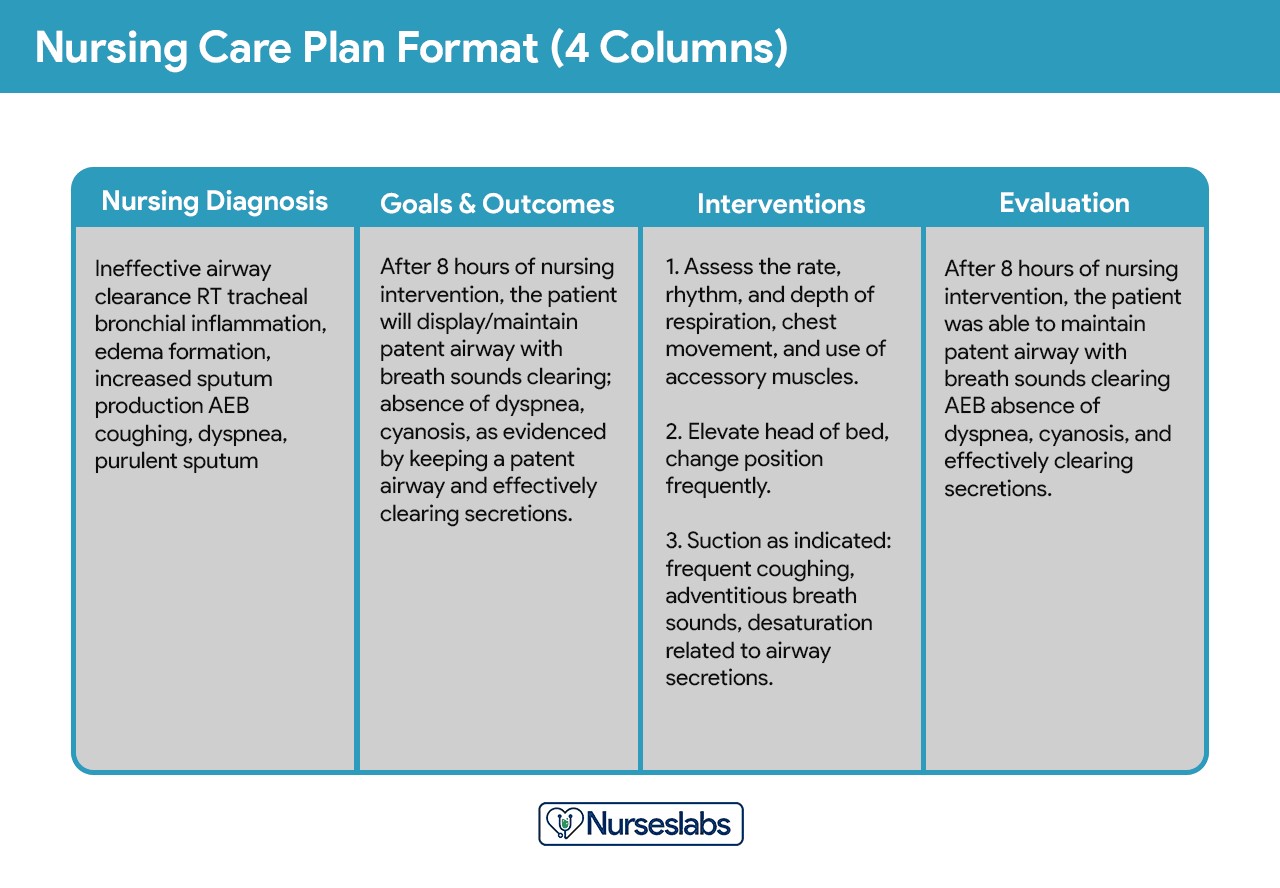
Common Care Plan Formats: Three-Column and Four-Column
Nursing care plans are often organized into columns to clearly present information. Common formats include three-column and four-column plans.
Three-Column Format
This format typically includes columns for:
- Nursing Diagnosis: Listing the identified nursing diagnoses.
- Outcomes and Evaluation: Combining desired patient outcomes with evaluation criteria.
- Interventions: Detailing the planned nursing interventions.
Four-Column Format
The four-column format separates outcomes and evaluation, providing columns for:
- Nursing Diagnosis: Stating the nursing diagnosis.
- Goals and Outcomes: Defining specific goals and expected outcomes.
- Interventions: Listing nursing actions.
- Evaluation: Dedicated space for evaluating the effectiveness of interventions and patient progress towards goals.
For those seeking templates, printable nursing care plan formats are readily available online, offering a practical starting point for creating structured care plans.
Student Care Plans: A Detailed Learning Tool
Student care plans are usually more comprehensive than those used by practicing nurses. They serve as educational exercises, designed to deepen understanding and critical thinking skills. Student plans often include an additional column for “Rationales” or “Scientific Explanation,” which requires students to justify their chosen interventions with scientific principles. These plans are frequently handwritten and are a vital part of nursing education.
Step-by-Step Guide to Writing a Nursing Care Plan
Creating a nursing care plan involves a systematic process, ensuring each aspect of patient care is thoughtfully addressed.
Step 1: Patient Data Collection and Assessment
The initial step in formulating a nursing care plan is thorough data collection. This involves building a comprehensive patient database using various assessment techniques:
- Physical Assessment: Conducting a hands-on examination to gather objective health data.
- Health History: Reviewing the patient’s past and current health conditions, including medical records.
- Interviews: Communicating directly with the patient and family to understand their perspectives and health experiences.
- Diagnostic Studies: Analyzing lab results and imaging to identify health indicators.
This detailed database is crucial for identifying related or risk factors and defining characteristics that will inform the nursing diagnoses. Critical thinking is paramount in this phase, integrating medical knowledge and professional guidelines to effectively evaluate patient needs and make informed clinical decisions.
Step 2: Data Analysis and Organization
Once data is collected, the next step is to analyze and organize this information. This involves:
- Clustering Data: Grouping related pieces of information together to identify patterns.
- Identifying Gaps and Inconsistencies: Recognizing areas where more information is needed or where data points conflict.
- Synthesizing Information: Combining data from different sources to form a holistic view of the patient’s health status.
This structured analysis leads to the formulation of nursing diagnoses, prioritization of issues, and setting of desired outcomes.
Step 3: Formulating Nursing Diagnoses: Examples and Guidance
Nursing diagnoses are standardized statements that describe a patient’s health condition that nurses can independently address. They are distinct from medical diagnoses, focusing on patient responses to health conditions rather than the conditions themselves.
Examples of Nursing Diagnoses:
- Actual Nursing Diagnosis Example: Impaired Gas Exchange related to pneumonia as evidenced by oxygen saturation of 88% on room air, shortness of breath, and productive cough.
- Risk Nursing Diagnosis Example: Risk for Falls related to muscle weakness and impaired balance.
- Health Promotion Nursing Diagnosis Example: Readiness for Enhanced Nutrition as evidenced by patient expressing interest in learning about healthy eating and requesting dietary information.
Formulating a nursing diagnosis involves a three-part statement (PES format):
- Problem (Nursing Diagnosis Label): A concise term or phrase representing the patient’s health problem. (e.g., Impaired Gas Exchange).
- Etiology (Related to Factors): The cause or contributing factors to the problem. (e.g., pneumonia).
- Signs and Symptoms (As Evidenced By): The defining characteristics or evidence of the problem. (e.g., oxygen saturation of 88%, shortness of breath).
Resources like the Nursing Diagnosis Handbook and online lists of nursing diagnoses can be invaluable in this step.
Step 4: Setting Priorities: Utilizing Maslow’s Hierarchy
Setting priorities is crucial for effective care planning. It involves ranking nursing diagnoses based on their urgency and importance. A useful framework for prioritization is Maslow’s Hierarchy of Needs, which organizes human needs into a pyramid structure:
- Physiological Needs (Basic Survival): These are the most critical and include needs like breathing, circulation, nutrition, and elimination. Nursing diagnoses related to these needs (e.g., Ineffective Airway Clearance, Deficient Fluid Volume) take top priority.
- Safety and Security Needs: Once physiological needs are met, safety becomes paramount. This includes physical safety (preventing falls, infection) and emotional security (establishing trust). Examples include Risk for Injury and Anxiety.
- Love and Belonging Needs: These involve social connection and belonging. Diagnoses might include Social Isolation or Impaired Social Interaction.
- Self-Esteem Needs: Needs related to self-worth, confidence, and achievement. Examples include Disturbed Body Image or Chronic Low Self-Esteem.
- Self-Actualization Needs: The highest level, involving personal growth and fulfillment. While less often a direct focus of acute care, these needs are important in long-term care and rehabilitation.
Example of Prioritization using Maslow’s Hierarchy:
For a patient admitted with pneumonia and anxiety about hospitalization:
- High Priority (Physiological): Impaired Gas Exchange related to pneumonia.
- Medium Priority (Safety/Security): Risk for Falls related to weakness.
- Lower Priority (Love/Belonging/Self-Esteem): Anxiety related to hospitalization.
Prioritization ensures that life-threatening issues are addressed first, followed by other important needs in a logical sequence.
Step 5: Establishing Client Goals and Desired Outcomes: SMART Approach
Goals and desired outcomes define what the nurse and patient aim to achieve. They should be SMART:
- Specific: Clearly defined and focused (e.g., “Patient will ambulate 50 feet”).
- Measurable: Quantifiable and observable (e.g., “…without shortness of breath”).
- Attainable: Realistic and achievable for the patient (considering their current condition and resources).
- Relevant: Aligned with the patient’s needs and nursing diagnoses.
- Time-Bound: Having a timeframe for achievement (e.g., “…by discharge”).
Examples of SMART Goals:
- For Impaired Gas Exchange: “Patient will maintain oxygen saturation above 92% on room air throughout hospital stay.”
- For Risk for Falls: “Patient will demonstrate correct use of call light and request assistance with ambulation at all times by day 2.”
- For Acute Pain: “Patient will report pain level of 3 or less on a 0-10 scale within 1 hour after pain medication administration.”
Goals can be short-term (achievable within hours to days) or long-term (weeks to months), depending on the care setting and patient needs.
Step 6: Selecting Nursing Interventions: Types and Examples
Nursing interventions are the specific actions nurses will perform to help patients achieve their goals. Interventions should be evidence-based, safe, and tailored to the individual patient.
Types of Nursing Interventions:
- Independent Interventions: Actions nurses can initiate autonomously based on their expertise (e.g., patient education, repositioning, monitoring vital signs). Example: For Impaired Gas Exchange, an independent intervention is “Educate patient on deep breathing and coughing exercises.”
- Dependent Interventions: Actions requiring a physician’s order (e.g., medication administration, specific treatments). Example: For Impaired Gas Exchange, a dependent intervention is “Administer oxygen therapy as prescribed.”
- Collaborative Interventions: Actions implemented in coordination with other healthcare professionals (e.g., physical therapy, dietary consultations). Example: For Impaired Physical Mobility, a collaborative intervention is “Consult with physical therapy for mobility assessment and gait training.”
Examples of Nursing Interventions for Common Nursing Diagnoses:
| Nursing Diagnosis | Example Nursing Interventions |
|---|---|
| Acute Pain | Administer pain medication as prescribed; Use non-pharmacological pain relief measures (e.g., heat/cold packs, relaxation techniques); Assess pain level regularly using a pain scale. |
| Risk for Infection | Perform hand hygiene before and after patient contact; Maintain aseptic technique during procedures; Monitor vital signs for signs of infection; Educate patient and family on infection prevention measures. |
| Impaired Physical Mobility | Assist with ambulation and transfers as needed; Encourage active and passive range of motion exercises; Ensure patient environment is free of hazards; Consult with physical therapy for mobility plan. |
| Deficient Knowledge | Provide patient education on disease process, medications, and self-care activities; Use various teaching methods (verbal, written, demonstration); Assess patient understanding and provide clarification as needed. |
| Ineffective Airway Clearance | Encourage coughing and deep breathing exercises; Suction airway as needed; Position patient to promote lung expansion (e.g., semi-Fowler’s position); Monitor respiratory status and oxygen saturation. |
| Anxiety | Provide a calm and supportive environment; Encourage patient to express feelings and concerns; Teach relaxation techniques; Offer diversional activities; Administer anti-anxiety medication if prescribed. |
| Imbalanced Nutrition: Less than Body Requirements | Offer small, frequent meals; Provide nutritional supplements as ordered; Monitor food intake and weight; Consult with a dietitian for nutritional assessment and plan; Address factors affecting appetite (e.g., nausea, pain). |

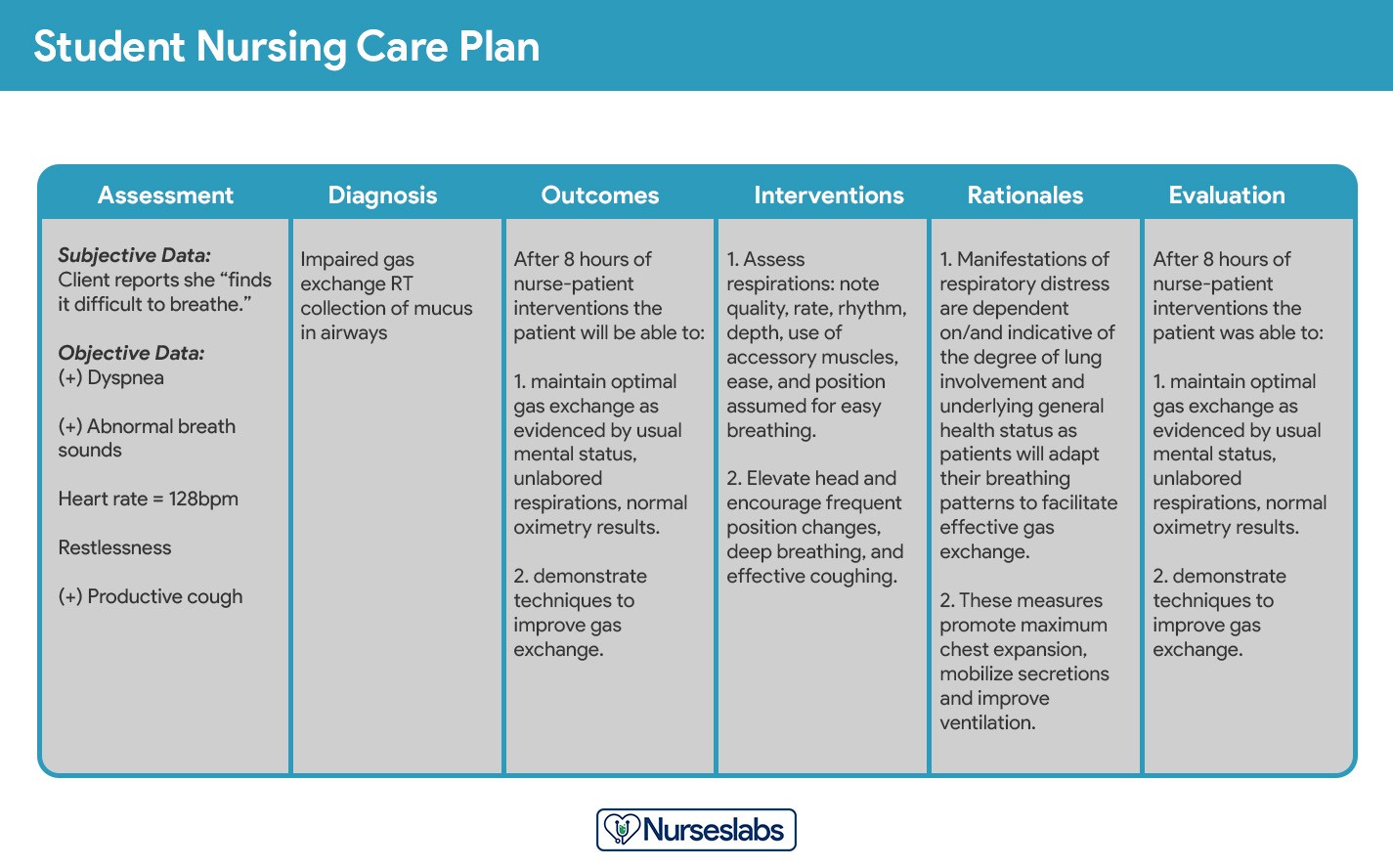
Step 7: Providing Rationales: The Why Behind Interventions
Rationales are the scientific justifications for each nursing intervention. They explain why a specific intervention is chosen and how it will help achieve the patient goal. Rationales are particularly emphasized in student care plans to promote a deeper understanding of the link between nursing actions and patient outcomes.
Example of Intervention and Rationale:
- Intervention: “Elevate head of bed to 30-45 degrees.”
- Rationale: “Elevating the head of the bed promotes lung expansion by reducing pressure from abdominal contents on the diaphragm, thereby improving oxygenation and easing breathing.”
Rationales should be based on nursing science, research, and best practices.
Step 8: Evaluation: Assessing Care Plan Effectiveness
Evaluation is the final step of the nursing process, where nurses assess the patient’s progress toward achieving the desired outcomes and evaluate the effectiveness of the nursing care plan. This is an ongoing process, not a one-time event.
Evaluation involves:
- Reassessing the Patient: Gathering current data to compare against the baseline assessment and desired outcomes.
- Analyzing Outcome Achievement: Determining if the patient has met, partially met, or not met the established goals.
- Modifying the Care Plan: Based on the evaluation, the care plan may need to be:
- Terminated: If goals are fully met and the problem is resolved.
- Continued: If progress is being made, but goals are not yet fully met.
- Revised: If there is little to no progress, or if the patient’s condition has changed, requiring new diagnoses, outcomes, or interventions.
Example of Evaluation Statement:
- Goal: “Patient will maintain oxygen saturation above 92% on room air throughout hospital stay.”
- Evaluation: “Goal Met. Patient consistently maintained oxygen saturation between 94-98% on room air throughout hospital stay. No signs of respiratory distress observed.”
Step 9: Documentation: Putting It on Paper (or Screen)
The final step is documenting the nursing care plan in the patient’s medical record. This ensures clear communication among healthcare providers and provides a legal record of the care provided. Documentation should be clear, concise, and adhere to facility policies. Electronic health records (EHRs) often have standardized formats for nursing care plans, streamlining documentation and access.
Comprehensive Nursing Care Plan Resources
Numerous resources are available to assist in creating effective nursing care plans. Online databases, textbooks, and mobile apps offer extensive lists of nursing diagnoses, interventions, and care plan templates.
Recommended Resources:
- Nursing Diagnosis Handbooks: Books like “Ackley and Ladwig’s Nursing Diagnosis Handbook” and “Nursing Diagnosis Manual” are essential for in-depth information on diagnoses and care planning.
- Online Nursing Care Plan Databases: Websites like Nurseslabs provide extensive lists of care plans and nursing diagnoses.
- Nursing Care Plan Templates: Downloadable templates in three-column and four-column formats can streamline the documentation process.
By utilizing these resources and following the step-by-step guide, nurses can develop comprehensive and effective care plans that significantly enhance patient outcomes and satisfaction.
This guide aims to equip nurses with the knowledge and tools necessary to master the art of nursing care planning, emphasizing the critical role of nursing diagnoses in creating patient-centered, effective care strategies. By focusing on examples and practical steps, it serves as a valuable resource for both students and practicing nurses striving for excellence in patient care.