Urinary tract infections (UTIs) stand as a frequent reason for antibiotic prescriptions in outpatient settings. However, with antibiotic resistance on the rise, optimizing antibiotic use is crucial, especially in urgent care centers where rapid decisions are made. Misdiagnosis of UTIs in these fast-paced environments can lead to unnecessary antibiotic use, contributing to resistance and harming patients. This article delves into the issue of false UTI diagnoses in urgent care, examining the factors that contribute to misdiagnosis and exploring strategies for more accurate diagnosis and antibiotic stewardship. We will address the critical need to differentiate true UTIs from conditions mimicking UTI symptoms, ultimately advocating for improved diagnostic accuracy in urgent care settings to combat antibiotic resistance and enhance patient care.
The Challenge of Diagnostic Accuracy in Urgent Care UTI Management
The increasing global threat of antimicrobial resistance necessitates a critical look at antibiotic prescribing practices across all healthcare settings. Urgent care centers, while vital for accessible and immediate medical attention, present unique challenges in antibiotic stewardship. The pressure for quick diagnoses and treatments, coupled with the non-specific nature of UTI symptoms, can contribute to the overdiagnosis of UTIs. This overdiagnosis frequently results in the inappropriate prescription of antibiotics when a UTI is not actually present – a “false diagnosis of UTI.”
Urinary tract infections are a leading cause of outpatient antibiotic prescriptions. However, studies reveal a significant percentage of these prescriptions are unnecessary or inappropriate, highlighting a critical area for improvement. The urgency of the urgent care setting may sometimes lead to presumptive treatment based on symptoms alone, without thorough diagnostic evaluation. This is further complicated by the fact that many conditions, such as sexually transmitted infections (STIs), overactive bladder, and even vaginal irritation, can mimic UTI symptoms. Distinguishing between these conditions and true UTIs is paramount to avoid false diagnoses and ensure appropriate antibiotic use.
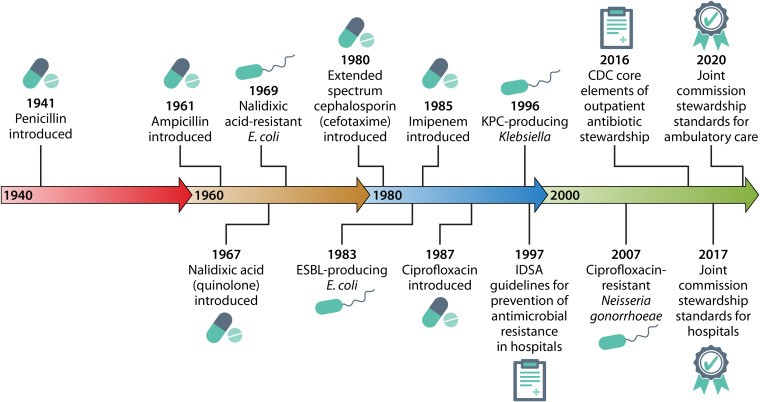
Timeline of antibiotic development, antimicrobial resistance, and the advent of antibiotic stewardship.
Differentiating True UTI from Mimicking Conditions in Urgent Care
Accurate diagnosis is the cornerstone of effective UTI management and antibiotic stewardship, especially in urgent care where time constraints are significant. The key challenge lies in differentiating a genuine UTI from other conditions that present with overlapping symptoms. Urgent care clinicians must be adept at identifying the nuances that distinguish a true infection from conditions like asymptomatic bacteriuria (ASB), sexually transmitted infections (STIs), overactive bladder, and even non-urinary tract issues that may manifest with urinary symptoms.
Asymptomatic Bacteriuria (ASB) vs. Symptomatic UTI
A major contributor to false UTI diagnoses in urgent care is the misinterpretation of asymptomatic bacteriuria (ASB) as a symptomatic infection. ASB, the presence of bacteria in the urine without accompanying symptoms, is common, particularly in older adults and women. Routine urine testing in urgent care settings, especially without clear clinical indications, can inadvertently detect ASB. If this bacterial presence is then misinterpreted as the cause of vague or non-specific symptoms, it leads to a false UTI diagnosis and unnecessary antibiotic treatment. Urgent care providers must rigorously adhere to guidelines that discourage treating ASB in non-pregnant adults and focus on symptom-based diagnosis for UTI.
Sexually Transmitted Infections (STIs) as UTI Mimics
Sexually transmitted infections (STIs) frequently present with symptoms that closely resemble UTIs, such as dysuria and urinary frequency. In the urgent care setting, particularly when evaluating young, sexually active individuals, STIs must be considered in the differential diagnosis of UTI. Failing to distinguish between a UTI and an STI can lead to a false UTI diagnosis, inappropriate antibiotic treatment that does not target the STI, and delayed or inadequate care for the actual infection. Urgent care protocols should emphasize taking a sexual history and considering STI testing, especially in women presenting with UTI-like symptoms, to avoid misdiagnosis and ensure correct treatment.
Overactive Bladder and Interstitial Cystitis
Conditions like overactive bladder and interstitial cystitis can also mimic UTI symptoms, particularly urinary urgency and frequency. These are non-infectious conditions and do not respond to antibiotics. In urgent care, where patients may present with acute exacerbations of chronic conditions, it is essential to differentiate these from acute UTIs. A history of chronic urinary symptoms, lack of typical UTI symptoms like dysuria, and previous negative urine cultures should raise suspicion for these alternative diagnoses and prevent a false UTI diagnosis.
Delirium in Older Adults: Avoiding the UTI Scapegoat
In older adults presenting to urgent care, delirium is sometimes mistakenly attributed to UTIs. While UTIs can cause systemic symptoms in the elderly, delirium is often multifactorial. Routinely attributing delirium to UTI and initiating antibiotics without a thorough evaluation for other causes can lead to a false UTI diagnosis. Urgent care providers need to be cautious in diagnosing UTI as the cause of delirium in older adults, especially in the absence of localizing urinary symptoms. A comprehensive assessment to rule out other causes of delirium is critical to avoid inappropriate antibiotic use.
The 5 Ds of antibiotic stewardship for UTI.
Strategies for Reducing False UTI Diagnoses in Urgent Care
Combating false UTI diagnoses in urgent care necessitates a multi-pronged approach, focusing on diagnostic stewardship and incorporating strategies to improve diagnostic accuracy at every step of the patient encounter.
Enhancing Symptom-Based Diagnosis
Urgent care clinicians should prioritize a thorough symptom assessment to differentiate true UTIs from mimicking conditions. Tools like symptom scores and clinical decision aids can help standardize this process. Emphasis should be placed on eliciting key UTI symptoms such as dysuria, urinary frequency, urgency, and hematuria, while actively seeking symptoms suggestive of alternative diagnoses like vaginal discharge (STI) or chronic urinary symptoms (overactive bladder, interstitial cystitis).
Judicious Use of Urinalysis and Urine Culture
Urinalysis and urine culture, while valuable diagnostic tools, should be used judiciously in urgent care. Routine urinalysis without specific clinical indication can increase the likelihood of detecting and misinterpreting ASB. Urine cultures should be reserved for cases of suspected pyelonephritis, complicated UTIs, recurrent infections, or when antibiotic resistance is a concern, rather than for routine uncomplicated cystitis in otherwise healthy individuals presenting to urgent care. Relying solely on a positive urinalysis result without considering the clinical context significantly increases the risk of false UTI diagnoses.
Implementing Rapid Diagnostic Tools with Caution
Rapid diagnostic tests for UTI are emerging as potential tools to improve diagnostic speed in urgent care settings. However, the implementation of these technologies must be approached cautiously. If rapid tests primarily detect bacteriuria without assessing for symptoms, they may inadvertently increase the false diagnosis rate by prompting antibiotic prescriptions for ASB. The value of rapid diagnostics in urgent care lies in their potential to rule out UTI quickly or guide antibiotic selection in confirmed cases, but they should not replace clinical judgment and symptom-based diagnosis.
Diagnostic Stewardship Programs in Urgent Care
Implementing formal diagnostic stewardship programs within urgent care centers is crucial. These programs should focus on provider education regarding appropriate UTI diagnostic criteria, emphasizing symptom-based diagnosis and the limitations of urine testing. Strategies like reflex urine cultures (culturing only when urinalysis meets specific criteria) and clinical decision support systems integrated into electronic health records can further aid in reducing unnecessary urine cultures and false UTI diagnoses.
The 5 Ds of antibiotic stewardship for UTI.
Conclusion: Towards Accurate UTI Diagnosis in Urgent Care
False diagnoses of UTIs in urgent care settings contribute significantly to unnecessary antibiotic use and the growing threat of antibiotic resistance. The fast-paced environment of urgent care, combined with the non-specificity of UTI symptoms and reliance on rapid, sometimes misinterpreted, diagnostic tests, creates a perfect storm for misdiagnosis. Addressing this challenge requires a concerted effort to improve diagnostic accuracy, emphasizing symptom-based diagnosis, judicious use of urine testing, and implementation of diagnostic stewardship programs.
Urgent care centers play a critical role in community healthcare, and optimizing their approach to UTI diagnosis is essential for antibiotic stewardship. By focusing on differentiating true UTIs from mimicking conditions, promoting guideline-concordant diagnostic practices, and leveraging diagnostic stewardship strategies, urgent care providers can significantly reduce false UTI diagnoses. This will lead to more appropriate antibiotic prescribing, combatting antibiotic resistance, and ultimately improving patient outcomes within the urgent care setting and beyond. Further research is needed to evaluate the effectiveness of specific diagnostic stewardship interventions in urgent care and to develop and implement practical tools that support accurate and timely UTI diagnosis in this vital healthcare environment.
REFERENCES
(References will be added here, formatted according to a standard citation style, drawing from the original article and additional relevant scholarly sources focusing on false UTI diagnosis in urgent care).
Biographies
(Biographies of authors, adapted from the original article if applicable, or replaced with biographies of experts in urgent care and antibiotic stewardship).