I. Introduction
The increasing understanding of inherited genetic conditions, coupled with the identification of associated genes and advancements in diagnostic techniques, has broadened the scope of prenatal genetic testing in both cytogenetic and molecular laboratories. However, prenatal diagnosis of genetic disorders is often complex. Obstetricians/gynecologists obtain amniotic fluid (AF) or chorionic villus samples (CVS) through invasive procedures that carry a risk of pregnancy loss. These samples are precious and often limited in quantity or quality. Laboratory testing relies on the certainty that the material being tested is of fetal origin and demands robust assay performance with accurate results. A positive result for a genetic condition can lead to the serious decision of pregnancy termination. Furthermore, laboratories are pressured to provide rapid turnaround times to alleviate parental anxiety and facilitate timely counseling and informed decision-making during the pregnancy.
A significant preanalytical challenge in prenatal diagnosis is the potential presence of maternal cells in CVS or AF samples, known as maternal cell contamination (MCC). This is particularly concerning for sensitive polymerase chain reaction (PCR)-based molecular assays, where even minute amounts of mutation-positive maternal cells can lead to false-positive results. While the risk of MCC in CVS or AF samples cannot be entirely eliminated, its extent is influenced by several factors. Studies indicate that MCC is more prevalent among clinicians performing fewer than 50 amniocenteses annually, who also experience higher rates of fetal loss post-procedure. Therefore, regular performance of these procedures is crucial for maintaining competency. The sample collection technique also plays a vital role. Discarding the initial 2–5 ml of AF sample, along with the first syringe, and collecting the sample with a second syringe reduces MCC risk. Factors that can increase MCC risk include multiple needle insertions, placental penetration, and lack of ultrasound guidance. Sample processing also impacts MCC risk. Uncultured (direct) AF cells have a higher MCC likelihood compared to cultured cells because the culturing process enhances amniocyte growth while limiting peripheral blood cell proliferation. However, in CVS tissue specimens, both fetal and maternal cell types can proliferate if chorionic villi are not properly separated from maternal decidua, making CVS cultures potentially more susceptible to MCC.
Currently, the primary practice guidelines for MCC assessment in prenatal testing are found in the 2006 edition of the American College of Medical Genetics’ “Standards and Guidelines for Clinical Genetics Laboratories.” Recognizing the potential for misdiagnosis due to maternal sequence co-amplification, we conducted a national survey of 35 laboratories offering prenatal genetic services to understand current testing practices and identify areas for standardization and quality improvement. This study aims to provide insights into current practices and propose suggestions for standardization and quality assurance in MCC testing within prenatal genetic diagnosis. For laboratories dedicated to precision and accuracy in genetic evaluations, such as a Gene Care Genetic Diagnosis Lab Surat Gujarat might aspire to, understanding and implementing robust MCC testing protocols is paramount for delivering reliable patient care.
II. Materials and Methods
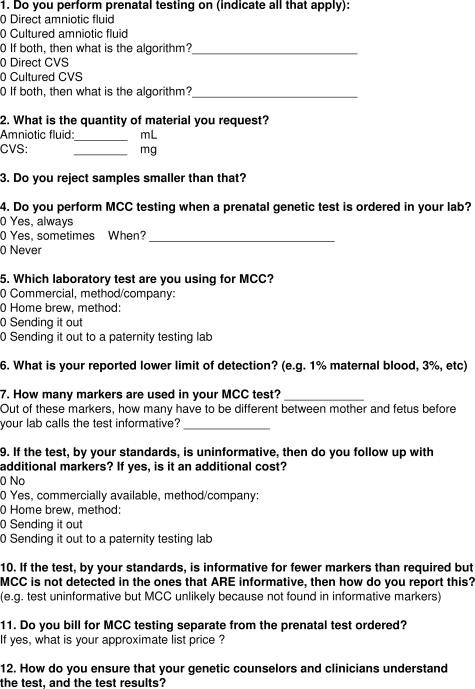
Laboratories across the United States were selected based on their Genetests listings for prenatal diagnostic testing of common inherited disorders like cystic fibrosis and α-thalassemia. Out of 46 clinical molecular laboratories contacted, 35 agreed to participate in a clinical practice survey. The survey questionnaire (Figure 1) covered various aspects, including: sample types tested (direct AF, cultured AF, direct CVS, cultured CVS), testing algorithms for multiple sample types, sample requirements, test indications, assay types, test performance and limitations, criteria and management of uninformative results, reporting, and billing. Medical directors or technical supervisors from participating laboratories were interviewed via phone conversations to gather detailed information.
Figure 1. Clinical practice questionnaire.
Clinical practice questionnaire used for phone interviews to assess current practices in maternal cell contamination testing across US laboratories offering prenatal genetic services.
III. Results
A. Sample Types and Handling
All participating molecular diagnostic laboratories offered AF testing. Sixty percent (21 of 35) performed prenatal diagnostic testing on both direct and cultured AF, while 40% (14 of 35) utilized only cultured AF cells. A large majority (88.6%, 31 of 35) also offered CVS testing. Among these, 67.7% (21 of 31) tested both direct and cultured CVS samples, while ten laboratories tested only CVS cultures, and four did not offer CVS testing at all (Figure 2). Laboratories offering testing on both direct and cultured cells based their sample type selection on factors such as: 1) sample volume requirements for PCR-based assays versus Southern blots, 2) gestational age and urgency of testing, and 3) the presence or absence of MCC evidence in a direct prenatal specimen. Five laboratories routinely performed follow-up cell cultures as a backup and for confirmatory testing. Two of these offered testing on all four specimen types, two offered testing on cultured AF and direct/cultured CVS, and one tested only direct and cultured AF.
Figure 2. Distribution of accepted specimen types.
Distribution of specimen types accepted by 35 molecular diagnostic laboratories for prenatal genetic testing. DA: direct amniotic fluid, CA: cultured amniotic fluid, DCVS: direct chorionic villus sample, CCVS: cultured chorionic villus sample.
Of the 35 participating laboratories, 24 conducted MCC testing in-house during the survey. Four were establishing in-house assays and had determined sample acceptance criteria, and three referred samples to a reference laboratory for MCC evaluation. Four laboratories did not perform MCC testing at all. Requested sample quantities for direct AF ranged from 2 to 25 ml, and for direct CVS, from no minimum to 30 mg (Figure 3, a and b). However, none of the laboratories rejected samples smaller than requested. In cases of insufficient volume, laboratories with culturing capabilities would proceed to culture the specimen. Culturing typically involved one to two T25 tissue culture flasks, though some laboratories had different protocols, ranging from four T25 flasks to a single confluent coverslip for PCR-based assays.
Figure 3. Sample requirements for prenatal testing.
Sample requirements for direct CVS and direct AF testing in US diagnostic laboratories. (a) Tissue sample requirements for direct CVS testing (n = 21 laboratories). (b) Sample volume requirements for direct AF testing (n = 21 laboratories).
B. Maternal Cell Contamination (MCC) Testing Practices
MCC testing in prenatal samples is a recommended standard of care according to the 2006 ACMG guidelines. At the time of the survey, one laboratory developing an MCC assay was undecided about their future testing practice, thus Figure 4 represents 34 laboratories. However, only 15 of 34 (44.1%) laboratories reported performing MCC testing without exception, and 6 of 34 (17.7%) performed it routinely unless no maternal sample was available, in which case testing proceeded with a disclaimer. Alarmingly, 12% (4 of 34) of laboratories never performed MCC testing. Laboratories that performed MCC testing “sometimes” cited various reasons, including: questionable diagnostic results suggesting MCC, inadequate maternal decidua dissection, or visibly bloody samples. Some laboratories performed MCC testing only when a fetal sample was positive or in autosomal recessive cases when the maternal mutation was present, assuming a negative maternal sample wouldn’t interfere with a fetal positive result. Conversely, some performed MCC testing for negative fetal samples or female fetuses undergoing cytogenetic testing. Other laboratories believed MCC was not an issue for male fetuses tested for X-linked disorders or due to a lack of prior incorrect prenatal results.
Figure 4. MCC testing practices in US laboratories.
Prevalence of MCC testing practices among 34 US laboratories. A significant portion of laboratories do not perform MCC testing universally, highlighting a lack of standardization in current prenatal diagnostic protocols.
C. MCC Assays and Sensitivity
The survey also investigated the types of MCC assays used. Among the 24 laboratories performing in-house MCC testing, plus three of the four developing assays and one of three sending samples out, commercially available DNA typing assays (Applied Biosystems, Promega) were used by 71.4% (20 of 28), while 28.6% (8 of 28) had developed in-house methods. The number of identity markers used ranged from 4 to 16 in commercial assays and 2 to 13 in in-house assays, with homebrew assays generally using fewer markers. Only three laboratories used four or fewer markers (10.7%).
Reported lower limits of detection for MCC assays varied widely from 1 to 20% and were not always determined (Figure 5). This data was provided by 27 laboratories. One laboratory indicating a 20% sensitivity included a 20% control in their assay due to observed allele dropout at lower contamination levels in their commercial assay.
Figure 5. Lower limit of detection for MCC assays.
Histogram displaying the reported lower limit of detection for MCC in US diagnostic laboratories. The variability in detection limits underscores the need for standardized assay sensitivity in prenatal MCC testing.
D. Assay Interpretation and Reporting
MCC assay interpretation can be complicated by allelic identity between mother and fetus, leading to uninformative results. The required number of informative markers for a conclusive interpretation ranged from one to four in validated assays. One laboratory used 3-8 markers, requiring 75-80% informativeness. Two-thirds of laboratories added markers if results were uninformative, while one-third did not, these latter facilities typically using nine or more markers initially. Twelve laboratories had not encountered uninformative results, although most required only two informative markers. One laboratory requiring four informative markers used an in-house assay with up to 10 markers, adding them as needed.
Nineteen laboratories reporting on uninformative MCC assay results with no MCC evidence typically reported them as “uninformative” or “equivocal,” with comments indicating MCC was unlikely but not ruled out, or that results were consistent with fetal origin and no MCC was detected. Of 28 laboratories offering or soon to offer MCC testing, four provided written reports only, and 23 offered written reports with verbal consultation for complex cases or all MCC-positive cases. One laboratory used MCC testing solely for internal QA/QC and did not issue reports, as it was not considered part of the clinician-ordered diagnostic testing. However, this laboratory had recently started MCC testing and had not yet encountered MCC in a prenatal sample.
E. Billing Practices for MCC Assays
Twenty-nine laboratories provided billing information. 58.6% (17 of 29) billed separately for MCC testing, 27.6% (8 of 29) included it as part of the prenatal test, and four laboratories provided MCC testing at no additional cost. Of the 17 charging separately, 15 provided pricing details. Twelve charged under $300, and two others charged between $300 and $500 (one depending on the number of markers used). One laboratory charged between $500 and $800 at the time of the survey.
IV. Discussion
Amniocentesis remains the most common procedure for prenatal diagnosis of inherited conditions. Procedure-related fetal loss rates are approximately 0.6% when performed with concurrent ultrasound guidance by experienced obstetricians. However, specimen quality, particularly the absence of MCC, is critical for accurate diagnosis. MCC can lead to interpretation errors in mutation analyses and aneuploidy detection by FISH. Even low MCC levels can interfere with molecular diagnoses due to PCR sensitivity, potentially detecting subpopulations of cells at levels as low as 0.1%, a sensitivity routinely achieved in chimerism and minimal residual disease assays. MCC can also impact cytogenetic diagnoses, particularly in female fetuses where FISH alone may not detect MCC, leading to false mosaicism interpretations. False-negative FISH results due to MCC in uncultured amniocytes have been reported in up to 7.5% of trisomic fetuses. Visual inspection alone is unreliable for MCC detection, as erythrocyte presence doesn’t always indicate maternal origin, and clear AF samples can still be contaminated. Discarding the initial 2-5 ml of AF sample is a crucial step in reducing MCC risk. MCC is not only a concern in prenatal testing; it’s also relevant in umbilical cord blood transplantation where maternal T cells can cause graft-versus-host disease.
Compared to AF, CVS, performed earlier in gestation (∼11 weeks), has a higher MCC risk. CVS is used for prenatal diagnosis and cytogenetic analysis of pregnancy losses, providing vital information for couples experiencing spontaneous abortion. Studies have reported erroneous 46, XX karyotypes in 29% and 5% of first and second-trimester pregnancy losses, respectively, potentially underestimating the true MCC incidence due to detection bias towards male fetuses misdiagnosed as female. Molecular MCC analysis is a valuable adjunct to cytogenetic testing in products of conception. Factors influencing erroneous karyotypes include villi quality and quantity, maternal tissue contamination, and conceptus characteristics. Optimal sampling and meticulous dissection are essential for minimizing MCC risk in CVS.
AF and CVS have distinct advantages and disadvantages reflected in the sample types accepted by laboratories (Figure 2). Direct AF testing reduces turnaround time by about 2 weeks and avoids culture costs. However, AF cell culture preferentially expands fetal cells and reduces maternal hematopoietic cell contamination, as these cells senesce and do not proliferate. Prolonged culture, however, can allow maternal fibroblasts and epithelial cells to grow, potentially leading to detectable MCC. CVS culture increases MCC risk as both fetal and maternal cells are present in the tissue sample. Generally, MCC risk is higher earlier in gestation due to specimen nature and a relatively lower number of fetal cells compared to maternal cells.
Despite the recognized risk of MCC-related misdiagnosis in prenatal testing, this survey reveals significant variability in MCC testing practices and assays among US clinical diagnostic laboratories. For example, the number of markers in MCC assays ranged from 2 to 16. While the marker number is somewhat arbitrary, using too few markers can create a false sense of security. Especially with low-level MCC (∼1%), maternal alleles may not be detected with limited markers. Expanded assays with multiple markers and requirements for several informative markers provide more robust detection. Most laboratories required only two or three markers for an informative assay. Reported lower detection limits also varied widely (1-20%, Figure 5). Visible red blood cell contamination, even at a few percent, should raise suspicion and prompt MCC testing. While red blood cells can be fetal or maternal, their presence warrants investigation. The lower detection limit is most critical in samples where MCC is not visually apparent. PCR-based assays can detect contamination down to 0.1% in controlled experiments. However, this depends on assay conditions and primers. A 1-2% MCC level is considered to increase misdiagnosis risk. Simple VNTR-PCR methods can reliably detect 2% MCC using gel electrophoresis, making this level achievable even without sophisticated equipment. MCC assays should aim to reliably detect MCC, focusing on frequency of detection rather than 100% marker detection.
Inheritance patterns of genetic conditions also influence MCC impact. For autosomal recessive conditions, 25% of fetuses will carry the maternal mutation, indistinguishable from the mother by mutation analysis alone. A proposed strategy is to perform diagnostic assays first and proceed to MCC testing only if the fetal sample is positive for the maternal mutation. This could reduce MCC testing by almost 50% in autosomal recessive testing, excluding multiple gestations and cases where both parents carry the same mutation. For mutation-positive direct or cultured CVS tested for cystic fibrosis, combining MCC testing with uniparental disomy assay for chromosome 7 (if MCC markers are not on chromosome 7) can identify trisomy 7, a common CVS aneuploidy. For dominant disorders, MCC testing can exclude false-positive results due to maternal contamination. However, for both dominant and recessive disorders, false-negative results due to maternal non-affected status are possible, particularly in CVS.
While the ACMG provides general prenatal testing guidelines (2006), their adoption across laboratories appears inconsistent. Alarmingly, 12% of surveyed laboratories never perform MCC testing. Despite MCC testing being performed by most molecular diagnostic laboratories, a lack of standardization persists. More specific guidelines and standardization recommendations are needed to improve diagnostic quality and patient care. While opinions on MCC testing may vary, professional practice organizations should determine practice standards. In the interim, a practical testing algorithm based on this survey, literature, and existing guidelines is proposed (Figure 6).
Figure 6. Practical testing algorithm for prenatal samples.
Proposed algorithm for prenatal genetic testing, emphasizing the integration of maternal cell contamination testing for improved accuracy and reliability in prenatal diagnoses.
To minimize errors in prenatal testing, universal MCC testing for all prenatal samples and inheritance modes is recommended. This approach maximizes information to address prenatal testing challenges. While maternal and paternal samples are sometimes requested, only maternal samples are strictly necessary for MCC testing, also avoiding nonpaternity issues. Larger sample volumes/tissue amounts, later gestational ages, and robust assays are preferable. Laboratories should understand primer band intensities and be alert to novel bands or intensity changes. MCC assay sensitivity should be determined. Maintaining a backup culture is essential for MCC-positive cases, insufficient sample quantity/quality, or result confirmation. A case example of a poor-quality prenatal sample with a false-negative α-globin deletion diagnosis highlights the importance of backup cultures. In this survey, only five laboratories routinely performed follow-up cultures for direct specimen backup and confirmatory testing.
The proposed algorithm (Figure 6) improves efficiency and accuracy. For instance, with direct AF samples, culture initiation occurs upon receipt, while MCC testing proceeds on the direct AF. If MCC is negative, diagnostic assays proceed on direct AF DNA. Positive diagnostic results are confirmed using cultured AF cells before final reporting.
While MCC does not always cause diagnostic errors, errors in prenatal settings can lead to inappropriate pregnancy terminations. This survey of 35 US laboratories demonstrates that most perform MCC testing, but clinical practice is not standardized, highlighting the urgent need for specific guidelines to ensure consistent and optimal prenatal patient care, potentially setting a benchmark for facilities like a gene care genetic diagnosis lab surat gujarat aiming for excellence in genetic diagnostics.
V. Acknowledgments
We thank all participating laboratories for their valuable contribution to this study.