Growth hormone (GH) deficiency is a medical condition that occurs when the pituitary gland does not produce enough growth hormone. This deficiency can be congenital (present from birth) or acquired later in life, and it can affect both children and adults. Growth hormone is crucial for growth, cell regeneration, and maintaining body composition. When deficient, it can lead to a range of health issues impacting body composition, energy levels, bone density, and overall quality of life. Accurate and timely Growth Hormone Deficiency Diagnosis is essential to initiate appropriate growth hormone replacement therapy and improve patient outcomes.
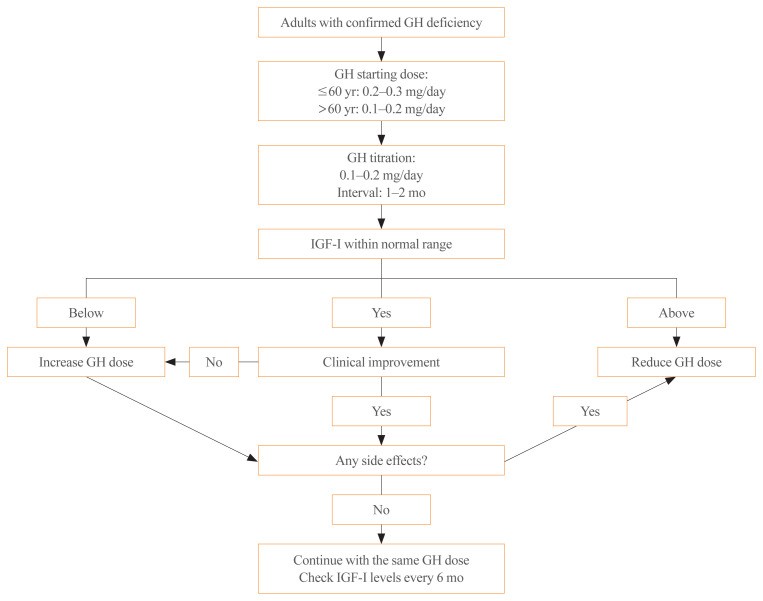 Algorithm for growth hormone (GH) therapy in GH deficiency adults. IGF-1, insulin-like growth factor-1.
Algorithm for growth hormone (GH) therapy in GH deficiency adults. IGF-1, insulin-like growth factor-1.
Understanding Growth Hormone Deficiency in Adults
Diagnostic Approaches for Adult Growth Hormone Deficiency
Diagnosing growth hormone deficiency in adults requires a multifaceted approach, primarily relying on stimulation tests to assess the pituitary gland’s ability to release GH.
1. Insulin Tolerance Test (ITT): The Gold Standard
The insulin tolerance test is widely recognized as the most reliable test for diagnosing adult GH deficiency. It involves administering insulin to induce hypoglycemia, which should stimulate GH release in individuals with a healthy pituitary function.
- Procedure: Insulin (0.05–0.15 U/kg IV) is administered under close medical supervision. Blood samples are collected at specific intervals (-30, 0, 30, 60, 120 minutes) to measure both GH and glucose levels.
- Interpretation: A peak GH level of less than 5.0 μg/L (according to the American Association of Clinical Endocrinologists) or 3–5 μg/L (as per the Endocrine Society) during hypoglycemia suggests GH deficiency.
- Considerations: It’s crucial that glucose levels drop sufficiently to stimulate GH release. ITT is contraindicated in patients with a history of seizures, coronary artery disease, pregnancy, or those over 65 years of age due to the risk of hypoglycemia.
2. Alternative Stimulation Tests When ITT is Contraindicated
When ITT is not suitable, alternative GH stimulation tests are necessary. It’s recommended to perform two or more of these tests to increase diagnostic accuracy. These alternatives include:
-
GH-Releasing Hormone (GHRH) – Arginine Test: This test combines GHRH, which directly stimulates the pituitary, with arginine, which suppresses somatostatin (an inhibitor of GH release).
- Procedure: GHRH (1 μg/kg IV, max 100 μg) followed by arginine infusion (0.5 g/kg, max 35 g over 30 minutes). Blood samples are taken at 0, 30, 45, 60, 75, 90, 105, and 120 minutes for GH measurement.
- Interpretation: A peak GH level below 4 μg/L is suggestive of GH deficiency, though cut-offs may need adjustment based on BMI.
- Limitations: May yield false normal results if GH deficiency originates from hypothalamic damage.
-
Glucagon Stimulation Test: Glucagon indirectly stimulates GH release by inducing insulin secretion.
- Procedure: Glucagon (1 mg, or 1.5 mg if weight >90 kg IM) is administered. Blood samples for GH and glucose are drawn at 0, 30, 60, 90, 120, 150, 180, 210, and 240 minutes.
- Interpretation: A peak GH level above 3 μg/L (or >1 μg/L if BMI ≥25 kg/m²) is considered normal. Obesity can blunt GH response.
- Contraindications and Side Effects: Contraindicated in severe fasting hyperglycemia (>180 mg/dL). Potential side effects include nausea, vomiting, headache, and delayed hypoglycemia.
-
Levodopa Stimulation Test: Levodopa stimulates GH release through dopamine receptors in the hypothalamus.
- Procedure: Levodopa (500 mg orally) is given. Blood samples for GH are collected at 0, 60, 90, and 120 minutes.
- Interpretation: A peak GH level above 3 μg/L is generally considered normal.
- Side Effects: May cause nausea, vomiting, dizziness, and headache.
-
Clonidine Stimulation Test: Clonidine stimulates GH release by releasing GHRH via alpha-adrenergic receptors.
- Procedure: Clonidine (0.15 mg/m², max 0.25 mg orally) is administered. Blood samples for GH are taken at 0, 30, 60, 90, and 120 minutes.
- Interpretation: A peak GH level above 3 μg/L is typically considered normal.
- Contraindications and Side Effects: Contraindicated in patients with coronary artery disease. May cause hypotension and drowsiness.
-
Macimorelin Test: Macimorelin is an oral GH secretagogue receptor agonist.
- Procedure: Macimorelin oral solution (0.5 mg/kg) is administered.
- Interpretation: A peak GH level greater than 2.8 μg/L is considered normal.
- Advantages: Similar sensitivity and specificity to ITT with fewer side effects.
- Considerations: Avoid concurrent use with drugs that prolong the QT interval. May not accurately diagnose hypothalamic disease. Common side effect is mild dysgeusia (taste disturbance).
3. Insulin-like Growth Factor-1 (IGF-1) Levels in Diagnosis
While normal IGF-1 levels do not rule out GH deficiency, low serum IGF-1 levels can be suggestive of GH deficiency, particularly in the absence of confounding factors such as poorly controlled diabetes, chronic liver disease, or oral contraceptive use. Low IGF-1 levels can strengthen the suspicion of GH deficiency and guide further diagnostic testing.
4. Clinical Presentation and Multiple Pituitary Hormone Deficiencies
In certain clinical scenarios, growth hormone deficiency diagnosis can be made without formal GH stimulation testing. This is applicable when a patient presents with typical clinical features of GH deficiency (e.g., increased body fat, decreased muscle mass, fatigue) AND has deficiencies in at least three other pituitary hormones, along with low serum IGF-1 levels. This combination strongly indicates hypopituitarism, likely including GH deficiency.
5. Re-testing Childhood-Onset GH Deficiency
For individuals diagnosed with childhood-onset GH deficiency without a known genetic cause or irreversible pituitary damage, repeated GH stimulation testing is recommended in adulthood. This is because some cases of childhood-onset GH deficiency may resolve spontaneously by adulthood. However, re-testing is not needed for those with proven genetic causes or irreversible damage, as their GH deficiency is likely to persist.
6. Avoiding Repeated Testing in Irreversible Pituitary Damage
Adult patients with established irreversible pituitary damage, such as structural lesions or genetic defects causing GH deficiency, do not require repeated GH stimulation tests. Their GH deficiency is considered permanent, and repeated testing would not alter the diagnosis or management.
Diagnosing Growth Hormone Deficiency in Children and Adolescents
Specific Diagnostic Considerations for Pediatric GH Deficiency
Diagnosing GH deficiency in children and adolescents requires a distinct approach, emphasizing growth patterns and often necessitating multiple stimulation tests.
1. Multiple GH Stimulation Tests in Children
When GH deficiency is suspected in children, it is crucial to perform two or more GH stimulation tests to confirm the diagnosis. This recommendation is due to the variability and potential for false positives in single GH stimulation tests in the pediatric population.
2. When Repeated Tests Are Not Needed in Children
Similar to adults, repeated GH stimulation tests are not necessary in children and adolescents with pituitary lesions or a confirmed genetic cause of GH deficiency. In these cases, the underlying pathology confirms the diagnosis, making repeat testing redundant.
Growth Hormone Measurement and Assay Considerations
The accuracy of growth hormone deficiency diagnosis is significantly influenced by the GH assays used. Variations in assay methodologies and standardization can lead to discrepancies in GH level measurements.
- GH Isoforms and Binding Proteins: GH in blood exists in various forms (isoforms and isomers), with 22 kDa and 20 kDa forms being most common. GH binding proteins can also interfere with immunoassays, affecting up to 50% of GH measurement.
- Assay Standardization: Different institutions use varied methods for GH measurement. It’s essential to use the GH calibration standard 98/574 from the National Institute for Biological Standards and Control and highly purified recombinant pituitary GH to ensure accurate and comparable results.
- Manufacturer Specifications: Manufacturers of GH measurement equipment should clearly specify assay validity, GH isoforms measured, analytes, antibodies used, and potential interference from GH binding proteins.
Conclusion: Ensuring Accurate Growth Hormone Deficiency Diagnosis
Accurate growth hormone deficiency diagnosis is fundamental for initiating appropriate and effective growth hormone replacement therapy. For adults, the insulin tolerance test remains the gold standard, with alternative stimulation tests available when ITT is contraindicated. In children, multiple stimulation tests are often necessary for confirmation. Careful consideration of clinical context, IGF-1 levels, and pituitary hormone status, along with standardized and reliable GH assays, ensures precise diagnosis and optimal patient management. This comprehensive approach helps healthcare professionals effectively identify and manage growth hormone deficiency, improving the health and well-being of affected individuals.